Anaphylactic shock is a lightning reaction that occurs when the body is hypersensitive as a result of repeated introduction or entry of an allergen into the body.
Adrenaline is administered as first aid , which quickly relieves the symptoms of anaphylaxis in a matter of seconds, making it the drug of choice for anaphylactic shock. If the drug was administered at home by someone other than a medical professional, it is necessary to contact a doctor afterwards, even if symptoms of anaphylaxis no longer appear.
This type of shock manifests itself after the penetration of the antigen into the body, when the body’s defense mechanisms are triggered, reacting inadequately to the allergen.
Various substances (dust, pollutants, some foods, bee stings and medications) act as allergens. Often anaphylactic reactions develop after the administration of drugs , which is why it is so important to check the body’s reactivity to certain types of drugs that cause anaphylactic shock.
Anaphylactic shock develops within a few minutes to five hours from the moment the allergen enters the body. If a person has hypersensitivity to an allergen, then no matter how or in what dosage the allergen entered the body, anaphylaxis will certainly manifest itself. With an increased dose of the allergen, the anaphylactic reaction is more pronounced.
If anaphylaxis causes bronchospasm or airway stenosis, hypoxia occurs. With complete stenosis and bronchospasm (when air does not enter the lungs), no more than five minutes remain for help. After this, irreversible changes occur in the brain, which leads to the clinical death of the patient.
Statistics
Every year, 100 out of 100,000 people are hospitalized with an anaphylactic reaction (data for 2020). Moreover, back in 1990 this figure was two times lower - 50 people, and in the 80s it was 20 people per hundred thousand population. The annual increase in anaphylaxis cases is believed to be caused by dietary diversity and an increase in the number of different types of drugs that cause allergic reactions in some people.
Causes
An anaphylactic reaction is caused by the poison of wasps, bees, bedbugs and other stinging insects, as well as food. The hyperreactivity reaction appears, most often, after the first meal (the allergen enters the body) or after several, when the body develops sensitization to the allergen. Most often, anaphylactic reactions are caused by peanuts and other nuts, seafood, wheat, eggs, milk, fruits and vegetables, chickpeas, and sesame seeds. Peanut allergies account for 20% of all food allergies .
Eczema, allergic rhinitis, asthma are diseases in which the risk of an anaphylactic reaction increases when exposed to an allergen to which the patient is hypersensitive. As a rule, patients know what exactly they are allergic to and try to avoid contact with these allergens. Hypersensitivity reactions are caused by foods, cigarette smoke, cat hair, etc.

Penicillin antibiotics, as well as vaccines and serums, also cause a severe anaphylactic reaction in sensitive people. Therefore, before their administration to such patients, special tests are performed to detect an allergic reaction.
Major triggers that can lead to anaphylaxis
Doctors have identified the main groups of triggers that provoke the development of anaphylactic shock much more often than others. The main drugs that cause violent reactions in the body are:
- antibiotics (primarily penicillin and streptomycin);
- B vitamins (most often vitamin B1);
- diclofenac;
- novocaine;
- analgin;
- radiopaque agents containing iodine;
- immune sera;
- blood substitutes.
In cases where it is known that the patient is at risk of developing anaphylactic shock, medications should be administered with extreme caution and under constant medical supervision.
Also among the most common provocateurs of the disorder are the poisons of stinging insects, primarily wasps and bees, as well as nuts and seafood.
Pathogenesis and symptoms
With anaphylactic shock, there is a sharp decrease in blood pressure to a minimum, which leads to hypoxia, since the blood does not deliver oxygen and necessary substances to organs and tissues. Cyanosis (blueness of the skin) or redness and severe urticaria appear.
The heart rhythm is disturbed, the pulse becomes weak, thread-like, clouding of consciousness and dizziness are observed.
Stenosis of the respiratory tract occurs due to swelling of the mucous membrane of the pharynx and throat, which is a consequence of the effect of histamine on the blood vessels. The patient tries to inhale, while whistling and wheezing are heard, which indicate a narrowing of the respiratory space. The swelling spreads to the entire face, affecting the eye area, cheeks, and neck.
With anaphylactic shock, pulmonary edema and fluid accumulation in the pleural cavity are possible, which significantly complicates breathing and causes respiratory failure.
One of the complications of anaphylaxis is a spasm of the bronchial muscles, which causes respiratory arrest. The patient requires urgent artificial pulmonary intubation.
First aid
What to do if a person develops anaphylactic shock? First, call the doctors. After the call, first aid is provided, including the following actions:
- Eliminate sources of allergens if known. Further contacts with them will strengthen the reaction.
- Lay the victim on a horizontal, flat surface, and raise his legs, for example, by placing him on a pillow. The head should be turned to the side to prevent the person from choking on their own vomit.
- Remove all objects located there from the oral cavity: leftover food, chewing gum, dentures.
- Clear the airways: remove mucus, remove the sunken tongue (if you lose consciousness).
- Open the windows for fresh air.
- If there is no pulse, begin resuscitation. To massage the heart, clasp your palms together and rhythmically press on the sternum so that it drops about 5 centimeters. Every few pushes, perform artificial respiration while covering your mouth (if the airways are swollen, this may not be effective).
Help with anaphylaxis - administration of adrenaline
As mentioned earlier, first aid for anaphylactic shock is the administration of adrenaline. This is a hormone that is produced in the human body in the adrenal medulla. The secretion of adrenaline increases in situations that require the mobilization of all the vital forces of the body: during stress or danger, during injuries or burns, etc.
Adrenaline affects the body systems in different ways:
- The hormone affects the adrenergic receptors of human blood vessels, promoting vasoconstriction. The pressure in the vascular bed increases and blood flow resumes.
- Stimulation of bronchial adrenergic receptors eliminates respiratory failure in the patient. Adrenaline increases the ionotropic effect on cardiac myocardiocyte cells, thereby increasing the number of myocardial contractions.
- Suppresses the release of cytokines by inhibiting basophils and mast cells, neutralizes the effect of histamine on the walls of blood vessels.
Anaphylaxis is regarded as a serious condition of the patient, which, without timely administration of adrenaline, causes death. Therefore, it is important to quickly and correctly select the dose of the drug. A single dose is 0.2-0.5 ml of 0.1% adrenaline, injections are given intravenously or subcutaneously. In the clinic, patients in a coma are given adrenaline by drip along with sodium chloride (saline).
For laryngeal edema, bronchospasm and pulmonary edema, respiratory failure, glucocorticosteroids (Methylprednisolone, Dexamethasone, Prednisolone, Hydrocortisone) are added, which enhance the effect of adrenaline and improve the patient's condition. Glucocorticosteroids are administered immediately in large doses: Methylprednisolone is administered 500 mg, Dexamethasone - 100 mg, Methylprednisolone - 150 mg (5 ampoules).

Synthetic antishock drugs based on adrenaline
Adrenaline hydrochloride . A widely used synthetic substitute for natural adrenaline. Acts on alpha and beta adrenergic receptors of blood vessels, causing vasoconstriction. It has the strongest effect on the vessels of the abdominal cavity and mucous membranes, and to a lesser extent on the muscle vessels. Increases blood pressure. Acts on beta-adrenergic receptors of the heart, enhancing its work and increasing the number of heart contractions.
Increases blood glucose levels (hyperglycemia) and accelerates metabolism in the body. Relaxes the muscles of the bronchi and intestines. Strengthens the tone of skeletal muscles.
Algorithm for a nurse to act in case of anaphylactic shock
Immediate care for anaphylactic shock is a mandatory action for the nurse. The patient’s life depends on the correctness of actions; this must be remembered. Therefore, it is so important to know the sequence of actions and strictly follow them in the event of a case of anaphylactic shock.
Anaphylactic shock is an acute systemic type I allergic reaction of a sensitized organism to repeated administration of an allergen, clinically manifested by hemodynamic disturbances with the development of circulatory failure and tissue hypoxia in all vital organs and threatening the patient’s life.
Medical assistance is provided immediately at the scene of anaphylactic shock.
Pre-medical measures:
- immediately stop administering the drug and call a doctor through an intermediary, remain with the patient;
- apply a tourniquet above the injection site for 25 minutes (if possible), loosen the tourniquet for 1-2 minutes every 10 minutes, apply ice or a heating pad with cold water to the injection site for 15 minutes;
- place the patient in a horizontal position (with the head end down), turn the head to the side and extend the lower jaw (to avoid aspiration of vomit), remove removable dentures;
- ensure the supply of fresh air and oxygen;
- if breathing and circulation stop, perform cardiopulmonary resuscitation in the ratio of 30 chest compressions and 2 artificial breaths “mouth-to-mouth” or “mouth-to-nose”;
- administer a 0.1% solution of adrenaline 0.3-0.5 ml intramuscularly;
- prick the injection site of the drug at 5-6 points with a 0.1% solution of adrenaline 0.5 ml with 5 ml of a 0.9% sodium chloride solution;
- provide intravenous access and begin administering 0.9% sodium chloride solution intravenously;
- administer prednisolone 60-150 mg in 20 ml of 0.9% sodium chloride solution intravenously (or dexamethasone 8-32 mg);
Medical measures:
- Continue administering a 0.9% sodium chloride solution in a volume of at least 1000 ml to replenish the circulating blood volume; in a hospital setting - 500 ml of a 0.9% sodium chloride solution and 500 ml of a 6% solution of Refortan HES.
- If there is no effect, hypotension persists, repeat the administration of a 0.1% solution of adrenaline 0.3-0.5 ml intramuscularly 5-20 minutes after the first injection (if hypotension persists, injections can be repeated after 5-20 minutes), in a hospital setting if possible Cardiac monitoring should be administered intravenously at the same dose.
- If there is no effect, hypotension persists, after replenishing the circulating blood volume, administer dopamine (200 mg of dopamine per 400 ml of 0.9% sodium chloride solution) intravenously at a rate of 4-10 mcg/kg/min. (no more than 15-20 mcg/kg/min.) 2-11 drops per minute to achieve a systolic blood pressure of at least 90 mmHg. Art.
- If bradycardia develops (heart rate less than 55 per minute), inject a 0.1% solution of atropine 0.5 ml subcutaneously; if bradycardia persists, repeat the administration at the same dose after 5-10 minutes.
Constantly monitor blood pressure, heart rate, and respiratory rate.
Transport the patient to the intensive care unit as soon as possible.
You may never need to be treated for anaphylactic shock because it won't happen to you. However, the nurse should always be ready for immediate action according to the given algorithm.
Algorithm for a nurse to act in case of anaphylactic shock
Since anaphylactic shock occurs in most cases with parenteral administration of drugs, first aid to patients is given by nurses in the manipulation room. The actions of a nurse during anaphylactic shock are divided into independent actions and actions in the presence of a doctor.
First, you must immediately stop administering the drug. If shock occurs during an intravenous injection, the needle must remain in the vein to ensure adequate access. The syringe or system should be replaced.
A new system with saline solution should be in every manipulation room. If shock progresses, the nurse should perform cardiopulmonary resuscitation according to current protocol.
It is important not to forget about your own safety; use personal protective equipment, for example, a disposable artificial respiration device.
Prevention of allergen penetration
If shock develops in response to an insect bite, measures must be taken to prevent the poison from spreading throughout the victim’s body:
- - remove the sting without squeezing it or using tweezers;
- - Apply an ice pack or cold compress to the bite site;
- — Apply a tourniquet above the bite site, but for no more than 25 minutes.
Patient position in shock
The patient should lie on his back with his head turned to the side. To make breathing easier, free the chest from constricting clothing and open a window for fresh air. If necessary, oxygen therapy should be given if possible.
The nurse's actions to stabilize the victim's condition
It is necessary to continue removing the allergen from the body, depending on the method of its penetration: inject the injection or bite site with a 0.01% solution of adrenaline, rinse the stomach, give a cleansing enema if the allergen is in the gastrointestinal tract.
To assess the risk to the patient's health, it is necessary to conduct research:
- — check the status of ABC indicators;
- — assess the level of consciousness (excitability, anxiety, inhibition, loss of consciousness);
- — examine the skin, pay attention to its color, the presence and nature of the rash;
- — establish the type of shortness of breath;
- - count the number of breathing movements;
- - determine the nature of the pulse;
- - measure blood pressure;
- — if possible, do an ECG.
The nurse establishes permanent venous access and begins administering medications as prescribed by the doctor:
- - intravenous drip of 0.1% solution of adrenaline 0.5 ml in 100 ml of physiological solution;
- — introduce 4-8 mg of dexamethasone (120 mg of prednisolone) into the system;
- - after stabilization of hemodynamics - use antihistamines: suprastin 2% 2-4 ml, diphenhydramine 1% 5 ml;
- - infusion therapy: rheopolyglucin 400 ml, sodium bicarbonate 4% -200 ml.
In case of respiratory failure, you need to prepare an intubation kit and assist the doctor during the procedure. Disinfect instruments, fill out medical documentation.
After stabilizing the patient's condition, he needs to be transported to the allergology department. Monitor vital signs until complete recovery. Teach the rules for preventing threatening conditions.
Section 5. ALGORITHM FOR EMERGENCY MEASURES IN ANAPHYLACTIC SHOCK
Section 4. LIST OF MEDICINES AND EQUIPMENT IN PROCEDURE ROOMS REQUIRED FOR TREATMENT OF ANAPHYLACTIC SHOCK
- Adrenaline solution 0.1% – 1 ml N 10 amp.
- Saline solution (0.9% sodium chloride solution) 400 ml bottles N 5.
- Glucocorticoids (prednisolone or hydrocortisone) in ampoules N 10.
- Diphenhydramine 1% solution – 1 ml N 10 amp.
- Eufillin 2.4% solution – 10 ml N 10 amp. or salbutamol for inhalation N 1.
- Diazepam 0.5% solution 5 – 2 ml. – 2 – 3 amp.
- Oxygen mask or S-shaped air duct for mechanical ventilation.
- System for intravenous infusions.
- Syringes 2 ml and 5 ml N 10.
- Tourniquet.
- Cotton wool, bandage.
- Alcohol.
- Ice container.
Anaphylactic shock is a pathological condition based on an immediate allergic reaction that develops in a sensitized body after the reintroduction of an allergen into it and is characterized by acute vascular insufficiency.
Causes : medications, vaccines, serums, insect bites (bees, hornets, etc.).
Most often characterized by a sudden, violent onset within 2 seconds to an hour after contact with the allergen. The faster the shock develops, the worse the prognosis.
Main clinical symptoms : sudden anxiety, feeling of fear of death, depression, throbbing headache, dizziness, tinnitus, feeling of tightness in the chest, decreased vision, “veil” before the eyes, hearing loss, heart pain, nausea, vomiting, pain in the abdomen, the urge to urinate and defecate.
On examination: consciousness may be confused or absent. The skin is pale with a cyanotic tint (sometimes hyperemia). Foam at the mouth and there may be cramps. The skin may have hives, swelling of the eyelids, lips, and face. The pupils are dilated, there is a boxy sound above the lungs, breathing is harsh, dry wheezing. The pulse is frequent, thread-like, blood pressure is reduced, heart sounds are muffled.
First aid for anaphylactic shock:
Source: https://stop-allergies.ru/algoritm-dejstviya-medsestry-pri-anafilakticheskom-shoke/
Indications for use
It is used for collapse (acute decrease in blood pressure), with a significant decrease in sugar levels (hypoglycemia), during an attack of bronchial asthma that is not controlled by fast-acting adrenergic bronchodilators, such as Salbutamol. Also used to eliminate anaphylactic reactions and ventricular fibrillation. Used for glaucoma and otorhinolaryngological diseases.
Dosage and route of administration
The drug is administered subcutaneously, intramuscularly and intravenously in a dosage of 0.3-0.75 ml of a 0.1% solution. For ventricular fibrillation, it is administered intracardially, for glaucoma - in the form of eye drops.
Symptoms
Symptoms depend on the type of allergen, the method of its penetration into the body, the individual reaction and sensitivity of the person. There are several groups of symptoms:
- Dermatological: unbearable itching, swelling of the skin, rashes in the form of urticaria (small blisters) or large spots, redness and hyperthermia (local increase in temperature), swelling. Symptoms occur in 90% of anaphylactic reactions and can appear in different parts of the body, but most often affect the face (eyelids, lips and cheeks), palms, inner thighs, soles of the feet, neck and genitals.
- Respiratory: difficulty breathing and wheezing, inability to take a deep, full breath, rapid or shallow breathing. Such symptoms develop in half of patients with anaphylaxis.
- Respiratory: nasal discharge and congestion, sore throat and dry cough, swelling of the larynx, sneezing, hoarseness.
- Gastrointestinal: disturbances in the swallowing process, intestinal spasms and frequent urge to defecate, flatulence and bloating, diarrhea, as well as nausea, sometimes leading to vomiting. These signs occur in approximately 25-30% of cases.
- Cardiovascular: pain or heaviness in the sternum, increased heart rate (pulse), low blood pressure, dizziness and weakness, pre-drowsy states (up to complete loss of consciousness). All this manifests itself in 30-35% of cases of anaphylactic shock.
- Signs affecting the central nervous system: confusion, changes in coordination, blurred vision (fog before the eyes), severe headache, convulsions, fear, panic attacks. These symptoms rarely occur in severe forms of reactions.
Epinephrine
Synthetic adrenaline substitute. Stimulates alpha and beta adrenergic receptors, increases heart rate. Acts as a vasoconstrictor, increasing blood pressure. Acts as a bronchodilator (expands the lumen of the bronchi during spasms of allergic origin). Reduces renal blood flow, reduces motility and tone of the gastrointestinal tract.
Reduces the production of intraocular fluid, thereby reducing intraocular pressure, dilates the pupils (mydriasis). Strengthens the conduction of impulses in the myocardium, reduces the heart's need for oxygen. Reduces the production of histamine, leukotrienes, cytokines, reduces the number of basophils.
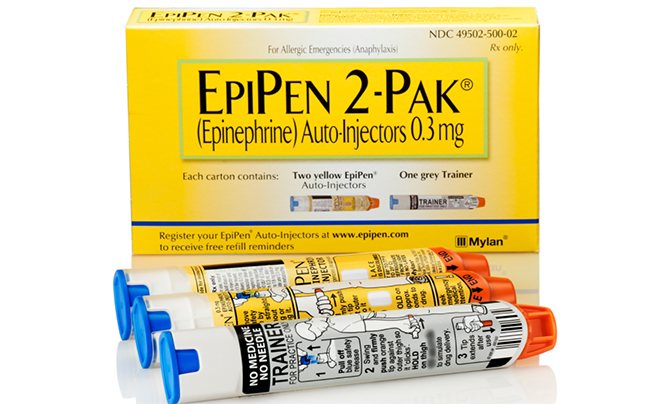
Removes potassium from cells, causing hypokalemia. Increases blood sugar levels, leading to hyperglycemia.
Indications for use
Epinephrine is used for anaphylactic , angioedema shock, which was caused by the use of drugs, food, as well as insect bites, reactions to blood transfusions. It is used to relieve attacks of bronchial asthma, COPD, asystole, and chaotic contraction of the ventricles. Effective for arterial hypotension, bleeding from superficial vessels. It is also used for hypoglycemia, during surgical interventions on the eyeball. Indicated for glaucoma.
Route of administration and dose
It is administered intravenously, intramuscularly and subcutaneously, as well as intracavernosally. It has the ability to penetrate the placenta, but does not cross the blood-brain barrier.
For anaphylaxis, epinephrine is administered intravenously at a dosage of 0.1-0.25 mg, diluted in 10 ml of sodium chloride. With this form of administration, the drug acts instantly. If an additional dose of epinephrine is required, the drug is administered by infusion or drip of 0.1 mg. For mild forms of anaphylaxis, the drug is used, diluted with water for injection, intramuscularly or subcutaneously at a dose of 0.3-0.5 mg. Effective in 3-5 minutes.
Adverse reactions
The reaction of the cardiovascular system to epinephrine is manifested by increased heart rate, angina pectoris, arterial hypertension, and irregular heart rhythm. An excited state, hand tremors, headache, bronchospasm, swelling of the mucous membranes, and rash are also observed. Possible nausea and vomiting, increased excretion of potassium in the urine.
Side effects
Side effects may develop with the use of adrenaline. The most common ones are:
- tachycardia;
- hypertension;
- arrhythmia;
- angina attack.
Sometimes it is necessary to administer adrenaline if there are contraindications, but only if the patient is in a life-threatening condition, and the benefit of the substance is expected to be greater than the possible harm. Contraindications include:
- pregnancy;
- vascular atherosclerosis;
- diabetes;
- thyroiditis;
- history of essential arterial hypertension.
In emergency situations, medical personnel themselves decide whether it is possible to use adrenaline for a particular patient.
List of used literature
REFERENCES AND INTERNET RESOURCES
1. Bychkov A.A. — Diagnostic reference book. M: “Phoenix” 2013.
2. Koryagina N.Yu., Shirokova N.V. - Organization of specialized
nursing care - M.:
- GEOTAR - Media, 2013.
3. Lychev V. G. Karmanov 15. K. - Guide to conducting practical classes on the subject “Nursing in therapy with a course of primary health care”:
- educational manual M.:
- Infra Forum, 2014.
4. Makolkin V.I., Ovcharenko S.I., Semenkov N.N. - Nursing in therapy - M.:
- LLC Medical Information Agency, 2014.
5. Mukhina S.A., Tarnovskaya I.I. - Theoretical foundations of nursing - 2nd ed., revised. and additional - M.:
- GEOTAR - Media, 2020.
6. Mukhina S.A. Tarnovskaya I.I. - Practical guide to the subject “Fundamentals of Nursing”; 2nd edition in Spanish add. M.:
- GEOTAR - Media 2014.
7. Nurse - Scientific and practical magazine - "Medizdat".
8. Nurse - Scientific, practical and journalistic magazine - Publishing house "Russian Doctor".
9. Obukhovets T.P. From T.A. Blyarov Chernova O.V. - Fundamentals of Nursing - ed. 13th add. reworked Rostov n/a Phoenix — 2014
10. Ostrovskaya I.V. Shirokova N.V. Fundamentals of Nursing: Textbook. - M.: GEOTAR - Media. 2014
11. Shapkin V.E., Zazdravnoye A.A., Bobro L.N. Pasieshvili - Handbook of therapy with the basics of rehabilitation - M.:
- Phoenix 2014
12. Internal diseases, edited by F.I. Komarova, Moscow, ed.
Medicine, 2012
13. Medicines, M.D. Mashkovsky, Kharkov, ed. Torsing, 2013
14. Therapist’s Diagnostic Handbook, edited by C.A. Chirkina,
Minsk, ed. Belarus, 2013
15. Internal diseases in 2 volumes. Ed. A.I. Martynova M.: GEOTARD, 2014. (UMO stamp)
16. Internal diseases. Textbook for medical universities, ed. S.I. Ryabov 4th edition. St. Petersburg Specialist. Lit, 2020. (marked by the Ministry of Health of the Russian Federation)
17. Vinogradov A.V. Differential diagnosis of internal diseases. M.: MIA. 2011.
18. Makolkin V.I. Internal illnesses. Textbook for students. 5th edition. M.: Medicine, 2020. (UMO stamp).
19. Murashko V.V., Strutynsky A.V. Electrocardiography. Tutorial. M.: Medicine, 2014. (UMO stamp).
20. Clinical recommendations. Pulmonology. Ed. A.G.Chuchalina. – M.GEOTARD-Media, 2010.
21. Clinical recommendations. Rheumatology. Ed. E.L.Nasonova - M.GEOTARD-Media, 2020.
22. Orlov V.N. Guide to electrocardiography. M.: MIA, 2013.
23. Guide for emergency doctors. help. Edited by V.A. Mikhailovich, A.G. Miroshnichenko. 3rd edition. St. Petersburg, 2020.
24. Sumin S.A. Emergency conditions. Educational literature for students of medical universities and faculties. 3rd ed., M.: MIA, 2012. (MZ stamp).
Internet resources.
https://meduniver.com/Medical/Therapy/10002.html MedUniver
https://www.astromeridian.ru/medicina/

