Author Vladan Djuric
Updated: 12/06/2019 10:35 Published: 12/04/2019 21:18
Health » Health and prevention » First aid
Anaphylaxis is one of the most complex allergic reactions that can lead to serious consequences. Doctors told us what to do in case of anaphylactic shock.
0 shared
It is known that an allergic reaction occurs when an allergen enters the human body. The immune system begins to react to the foreign substance by releasing immunoglobulins. The sensitivity of the body increases several times, which increases the likelihood of contracting a virus or infection.
When the allergen interacts again with familiar cells of the immune system, mediators are released. They cause an inflammatory process. A person may experience symptoms such as itching and swelling.
The allergic condition tends to develop. The number of mediators increases, and the immune system reacts to allergens, disrupting the functioning of organs. In this case, even death is possible.
Allergens can be any substance. They are most often found in medications, such as antibiotics. Medicines containing muscle relaxants and anesthetics are also included in the group of drugs with allergens. Foreign substances can even be found in vaccines.
Doctors say that some of the allergens are found in meat products. Clinical studies show that meat may contain antibiotics and muscle relaxants. Foods that contain allergens include all citrus fruits, food additives, seafood and legumes.
The source of the allergen is also insect bites, especially bee bites.
Allergens can occur during periods of increased pollen activity. It has also been proven that anaphylactic shock develops when combining sports training with nutritional supplements or the use of medications.
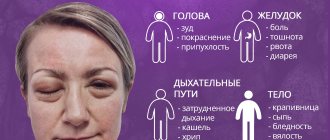
Signs of anaphylactic shock
The clinical manifestations of anaphylactic shock largely depend on the exposure to which allergen that provoked the acute allergic reaction.

This type of pathological condition of the body is accompanied by the occurrence of the following symptoms:
- redness of the skin in the area of contact of the body with a potential irritant;
- severe itching of the epithelial tissues and mucous membrane of the oral cavity, larynx, which only intensifies;
- a sharp decrease in blood pressure;
- a feeling of severe pain that appears immediately after contact with the allergen;
- dizziness;
- nausea;
- attacks of spasmodic pain inside the abdomen;
- diarrhea;
- vomiting if the allergen gets inside the gastrointestinal tract;
- multiple swelling of the mucous membranes;
- feeling of suffocation and lack of air;
- loss of consciousness;
- a burning sensation in the chest area (this symptom of anaphylactic shock occurs in the case of an allergic reaction to a drug that was administered intravenously);
- narrowing of the lumen of the bronchi, which leads to disruption of the gas exchange process;
- pale facial skin;
- cyanosis of the surface of the lips, fingers and toes;
- collapse of all life support systems of the body.

The above symptoms of anaphylactic shock can appear within 1-2 minutes. In most cases, people who are in close proximity to the victim do not always have time to understand the reason for the patient’s unsatisfactory state of health.
Epinephrine
Epinephrine is an adrenaline substitute also used medically for anaphylaxis. It acts on alpha and beta adrenergic receptors, increasing heart rate. The drug also has a vasoconstrictor effect, thereby increasing blood pressure, and helps expand the lumen of the bronchi during spasmodic allergic reactions. Additionally, it helps improve the conductivity of impulses in myocardial tissue, which reduces the need for oxygen in the heart muscle. The intensity of histamine production also decreases after the administration of epinephrine.
First aid for an attack
When the first signs of anaphylactic shock appear, a person should be provided with emergency medical care, which consists of performing the following algorithm of actions:
- The patient is placed in a horizontal position.
- It is necessary to free the victim’s neck and chest from clothing, the impact of which may complicate the act of breathing.
- A tourniquet should be applied above the area of the body where the drug was injected, a poisonous insect bite occurred, or exposure to another potential allergen occurred.
- Introduce adrenaline and glucocorticoids, which have anti-shock and anti-allergic effects, into the patient's body.
- Organize the patient's inhalation with an additional source of oxygen.
In the absence of medical equipment and increasing respiratory failure, artificial respiration is performed. At this stage of emergency care, the patient may require urgent intubation with connection to a ventilator.
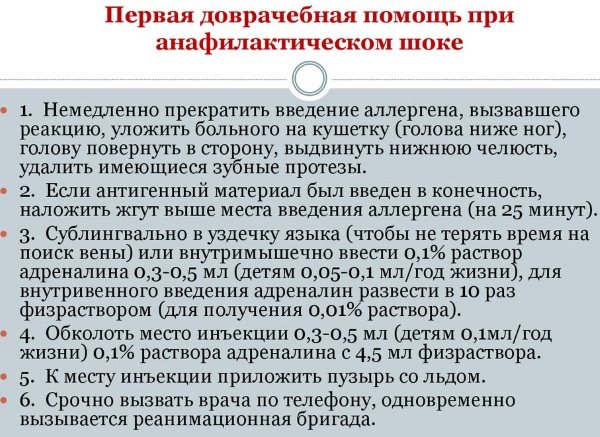
When artificial ventilation is not possible, tracheostomy is used. The walls of the victim’s larynx are pierced with 6 injection needles, which have a wide lumen diameter.
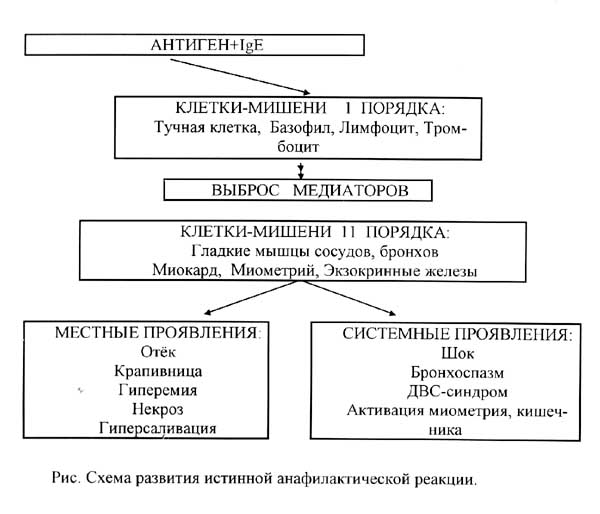
Mechanism of development of allergic shock
The occurrence of this pathology begins directly with the contact of the immune system with a specific allergen, as a result of which specific antibodies are produced, which in turn lead to the release of a huge number of inflammatory factors.
And these inflammatory factors further penetrate the tissue and organs, resulting in impaired circulation and blood clotting, which can lead to cardiac arrest.
Typically, anaphylactic shock develops when the body comes into repeated contact with the irritant, although in some cases this pathology can occur during the initial interaction with the allergen.
The first stage in the development of allergic shock is sensitization, that is, increased sensitivity of the body to a specific allergen.
And the second stage of this mechanism for the development of anaphylaxis is the anaphylactic reaction itself, which consists of a protective reaction of the immune system to the re-entry of the allergen into the body.

The development of anaphylaxis is directly related to decreased immunity of the body
After the irritant enters the blood again, specific substances are released, especially histamine, which is responsible for allergic reactions.
Such protective reactions of the body lead to the development of swelling and vasodilation, which in turn provokes breathing problems.
Allergic shock leads to the release of a huge amount of histamine, which disrupts the functioning of all systems and organs of the human body.
That is, we can say that the development of anaphylactic shock occurs in 3 successive stages:
- immunological stage;
- pathochemical stage;
- pathophysiological stage.
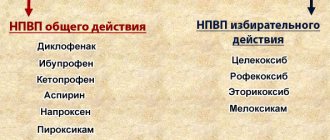
Groups of drugs used for severe allergic reactions
If signs of an acute allergic reaction appear, not only Prednisolone solution is used, but also a complex of other medications that can restore stable functioning of the heart, respiratory system and central nervous system. The table below lists the main types of medications that are used to relieve attacks of anaphylactic shock.
| Types of pharmacological groups | Purpose of drugs |
| Antishock | Medications of this type are used to stabilize the patient’s cardiovascular system, as well as prevent collapse. Antishock drugs stimulate more active work of the heart, endocrine glands, and excite receptors of the peripheral nervous system. An adrenaline solution is used as a medicine with anti-shock properties. |
| Antihistamines | Antihistamines suppress the pathogenic effects of allergens that initially provoked an acute reaction in the body. When using medications in this category, only those drugs that do not reduce blood pressure are used. For example, Tavegil, Diphenhydramine 1% concentration, Suprastin. The administration of the antihistamine Diprazine is strictly contraindicated, as it has a strong allergenic potential and can also lower blood pressure. |
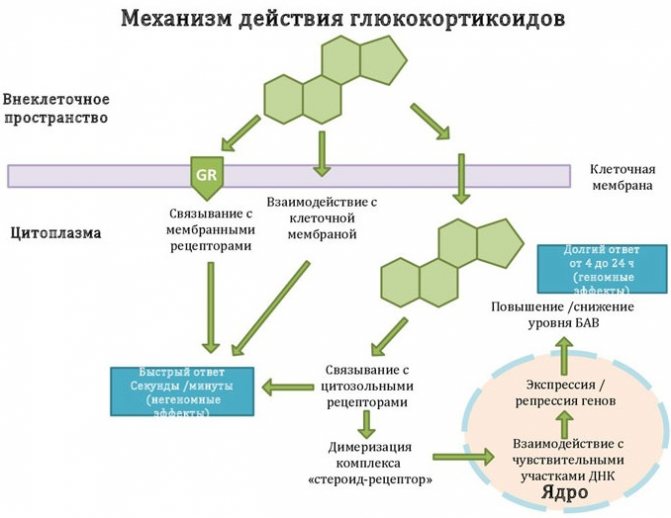
| Glucocorticosteroids | Glucocorticosteroids are potent drugs that relieve an attack of acute allergies, eliminate swelling and have an anti-inflammatory effect. A characteristic feature of medications in this group is that their effect appears after a certain period of time, but at the same time they have a prolonged effect. |
| Vasodilators | The dilation of the walls of blood vessels ensures an increase in the lumen inside the bronchial tree. After taking drugs of this group, the patient is able to breathe freely, signs of hypoxia, pallor and cyanosis of the skin disappear. For anaphylactic shock, an injection solution of Euphyllin is used, as well as other medications based on it (Aminophylline). |
The mechanism of action of Prednisolone for allergies
Prednisolone acts slowly in anaphylactic shock, but the medication has an excellent prolonged effect. Unlike drugs based on adrenaline, the implementation of the therapeutic properties of glucocorticoids occurs after several tens of minutes.
At the same time, medications in this category provide longer-term protection of the body from the occurrence of a repeated attack of anaphylactic shock. For example, if an excess amount of allergens is still present in the patient’s blood or digestive tract.
Prednisolone is a synthetic glucocorticoid, which is a complete analogue of hydrocortisone. The therapeutic properties of this medication are realized due to its pronounced antiallergic and immunosuppressive effects on the patient’s body.
Prednisolone is effective for anaphylactic shock due to its immunosuppressive properties
Prednisolone inhibits the proliferation of T-lymphocytes, which are directly involved in the acute immune reaction that occurs after contact with a potential allergen.
The constituent components of this drug slow down the release of cytokines from the structure of lymphocytes, reduce the intensity of the formation of specific antibodies, the appearance of which is also typical in conditions of anaphylactic shock.
The pronounced antiallergic properties of Prednisolone are manifested by reducing the intensity of production and secretion of mediators of the allergic reaction. The process of slower release of histamine basophils, as well as mast cells, starts. The quantitative indicator of free basophils and lymphocytes is reduced.
During the period of action of the constituent components of Prednisolone, the development of connective and lymphoid tissue almost completely stops, and the sensitivity of effector-type cells to potential allergens and irritants decreases.
The physiological process of formation of specific antibodies is inhibited, and the intensity of the immune response completely changes towards its weakening.
After injection, the active substance of this drug in the form of prednisolone, converted in the form of sodium phosphate, quickly saturates the composition of the patient’s bloodstream, binding to plasma proteins by 90%. Metabolism of Prednisolone occurs in the liver tissues, and its excretion is carried out by the kidneys.
Metabolites that are formed as a result of the breakdown of this medication do not exhibit biochemical activity. About 20% of Prednisolone is excreted by the kidneys absolutely unchanged. The rest of the medication is utilized in the form of metabolites. The half-life of this substance is 2 to 3 hours after intravenous injection.
Pathogenesis
The pathogenesis of allergic reactions is studied quite a lot and acquires new features every year.
Today it distinguishes:
- immunological stage (entry of the allergen into the body, production of antibodies, their adsorption on the surface of mast cells). The stage passes without major symptoms. But the reaction to this allergen remains in the body’s immunological memory and occurs in a hypertrophied version when the aggressive agent is repeatedly exposed;
- immunochemical (interaction of re-entered allergens with existing antibodies). This releases histamine, kinins, and prostaglandins. These chemicals cause a nonspecific reaction in the body, the more intense the more of them are formed.
- stage of pathophysiological changes (in other words, manifestations of symptoms).
The course of all three stages can take place in a few seconds (maximum up to two hours), especially if the body is hypersensitized.
What drugs should be combined with Prednisolone for anaphylactic shock?
Prednisolone for anaphylactic shock is administered in combination with other drugs that stimulate the cardiovascular system, suppress the sensitivity of histamine receptors, and have an immunosuppressive and antiallergic effect.
During the manifestation of symptoms of anaphylaxis in combination with Prednisolone, the following medications should be used simultaneously:
- from 0.2 to 0.5 ml of Adrenaline solution of 0.1% concentration, which is administered subcutaneously or intravenously depending on the severity of the patient’s condition;

- Dexamethasone with a single dose of up to 20 mg of the active substance;
- Methylprednisolone in amounts up to 500 mg;
- 20 ml of Eufillin solution with a concentration of 2.4%, which are administered intravenously and very slowly;
- from 1 to 2 ml of a 1% solution of Diphenhydramine, Tavegil, or Suprastin.
The above drugs do not interact negatively with Prednisolone injection solution, but only enhance its anti-shock and anti-allergic properties. The combination of these medications allows you to stabilize the condition of a patient with signs of anaphylactic shock, as well as avoid negative consequences such as death.
Advantages of the drug in comparison with other antiallergic drugs
Prednisolone for anaphylactic shock is used for emergency therapy aimed at suppressing the body's acute immune response and eliminating signs of laryngeal edema.
The following main advantages of this drug over other antiallergic drugs are highlighted:
- does not cause a decrease in blood pressure;
- provides a prolonged therapeutic effect;
- eliminates the symptoms of an acute allergy attack, when most antihistamines are effective only for moderate allergic reactions;
- prevents the development of severe bronchial spasm;
- helps to quickly relieve swelling of the mucous membranes of the larynx;
- allows you to restore stable breathing to the patient and prevent death from hypoxia.
In combination with immunosuppressive and antiallergic properties, Prednisolone has a pronounced anti-inflammatory effect, which is extremely important in situations where anaphylaxis has developed after the bite of a poisonous insect or reptile. In this case, the medication will eliminate inflammation of epithelial tissues and also accelerate the process of their regeneration.
Additional or rare symptoms
Often the clinical picture of anaphylactic shock is accompanied by abdominal pain syndrome. More often it appears half an hour after the crisis.
Often these pains are confused with signs of perforation of a stomach or duodenal ulcer. The same symptom of irritated peritoneum, the same “acute abdomen”.
And only by the presence of other symptoms (drop in blood pressure, cardiovascular disorders, changes in the nature of the skin), as well as the corresponding medical history, can an immediate allergic reaction be reliably diagnosed.
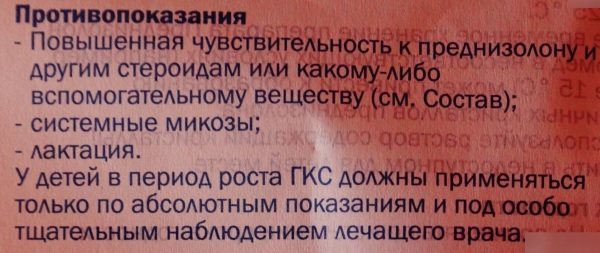
Contraindications for use
Prednisolone for anaphylactic shock is not used as an emergency treatment drug in the presence of direct medical contraindications.
This medication is prohibited for use in patients who have an individual intolerance to prednisolone and other chemicals based on it. Precautionary measures are justified by a significant risk of worsening the manifestations of an acute allergic reaction with further progression of already developed anaphylaxis.
At the same time, Prednisolone is prescribed with extreme caution to patients who have the following diseases:
- infectious and parasitic diseases of viral, bacterial or fungal origin;
- gastritis;
- diverticulitis;
- ulcerative damage to the walls of the stomach;
- tuberculosis, which is in a latent form;
- strongloidosis;
- AIDS, HIV and other immunodeficiency conditions of the body;
- chicken pox;
- ulcerative colitis, accompanied by a high risk of intestinal perforation or the formation of a purulent abscess;
- myocardial infarction;
- morbid obesity grade 3-4;
- severe form of heart failure;
- hypothyroidism, as well as thyrotoxicosis of the thyroid gland;
- diabetes;
- nephrourolithiasis;
- liver or kidney failure occurring in a chronic form of its development;
- osteoporosis of bone tissue;
- acute form of psychosis;
- angle-closure glaucoma;
- the presence of hypoalbuminemia, as well as pathological conditions that preceded its occurrence;
- polio.
Patients with these diseases should be under constant supervision by medical personnel throughout the entire period of antishock therapy. If signs of side effects or exacerbation of concomitant diseases appear, further use of Prednisolone is contraindicated.
Dangers and complications
The main danger of the disease is its lightning speed of development and the severity of clinical manifestations.
As a result of diagnostic defects, acute respiratory failure, pulmonary and cerebral edema, and acute cardiovascular failure can quickly develop.
The rate of development of such reactions is influenced not so much by the dose of the allergen as by the method of its administration.
Complications develop most quickly with the parenteral route of administration.
This applies to allergies to intravenous medications, including antibiotics.
The entry of an allergen into the blood immediately leads to blocking of vital centers of the brain, requiring immediate compensation therapy
After relief of the acute phase, complications may develop such as:
- myocarditis;
- myocardial infarction;
- nephritis, pyelonephritis;
- pneumonia and others;
- intestinal bleeding;
- hemiparesis;
- clouding of consciousness.
Precautions when using Prednisolone
During therapy with the drug Prednisolone, the following precautions must be taken to maintain health:
- periodic observation by an ophthalmologist;
- control over the cellular composition of peripheral blood, as well as glucose levels;
- checking blood pressure;
- maintaining a stable electrolytic balance;
- dosed intake of antacids and drugs containing potassium ions, which minimize the risk of side effects;
- refuse vaccination, since Prednisolone suppresses the occurrence of an adequate immune response (artificial immunization of the body should be carried out later, after discontinuation of the medication);
- carry out x-ray monitoring of the preservation of the mineral structure of the bones of the spine, upper and lower extremities.
During long-term therapy with Prednisolone, it should be taken into account that this drug increases the concentration of 11- and 17-hydroxyketocorticosteroids. In patients who have previously suffered a myocardial infarction or suffer from liver cirrhosis, these diseases may progress with further destruction of the affected tissues.
Dosages
The prednisolone dosage regimen for patients with signs of anaphylaxis is established by the attending physician, taking into account the severity of the patient's condition.
For adults
For patients of the adult age group who are in a state of anaphylactic shock, jet intravenous administration of Prednisolone is indicated in a dosage of 50 to 150 mg of the active substance. In particularly severe cases, this dose can be increased to 400 mg.
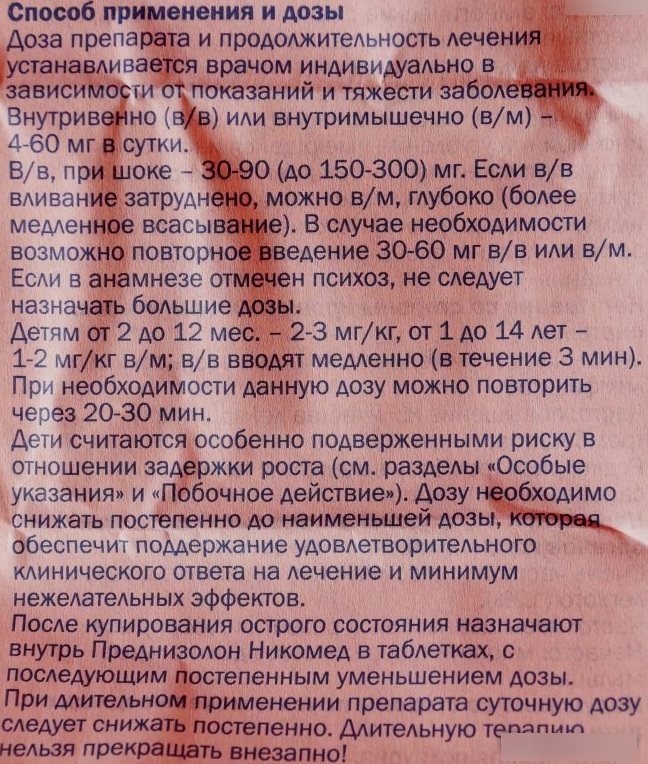
After stabilizing the patient’s condition and normalizing blood pressure, further administration of Prednisolone is carried out intravenously, but as part of a drip solution. Repeated use of this drug is possible within a time interval of 3-4 hours.
For adult patients, the average daily dose of Prednisolone ranges from 300 to 1200 mg, with its subsequent reduction as health improves. It is important to remember that abrupt cessation of therapy with this drug may provoke withdrawal symptoms.
For children by age
For children of all age groups, whose bodies are still growing, the use of Prednisolone is possible only in extreme cases, when there is a real threat to the child’s life.
The dose of glucocorticoid is determined individually by the attending physician, who assesses the severity of anaphylaxis. After the injection of the drug, the child remains in the inpatient department of the hospital under round-the-clock supervision of medical personnel.
Can the drug be used during pregnancy, breastfeeding?
For women who are pregnant, Prednisolone is prescribed only in extreme cases when there is a real threat to the life of the expectant mother. In this situation, the medication is used for symptomatic therapy to relieve acute manifestations of anaphylaxis.
A course of treatment with this medication causes disturbances in fetal growth and also leads to atrophic processes in the structure of the child’s adrenal cortex. Prednisolone is not used during breastfeeding of a newborn. In this case, it will be necessary to stop further lactation.
Prednisolone is an effective drug that belongs to the pharmacotherapeutic group of glucocorticoids. This medication has anti-inflammatory, immunosuppressive, and antiallergic properties.
Prescribing dosed Prednisolone can eliminate acute symptoms of anaphylaxis, stabilize blood pressure and relieve swelling of the mucous membranes. In case of anaphylactic shock, the first dose of glucocorticoid is administered intravenously using the jet method. Subsequently, the medication is used as part of drip solutions. The duration of therapy is determined by the doctor.
Adverse reactions
Side effects from the use of epinephrine include disturbances in heart rhythm and its acceleration, as well as agitation (sometimes with trembling of the hands), headache, rash and swelling of the mucous membranes. In rare cases, nausea and vomiting may occur. This condition requires medical intervention.
Anaphylactic shock is a deadly condition that requires medical attention from the very first minutes. If there is an increased risk of its development, a person always needs to have adrenaline for injection with him, which today is produced in special pumps for administration.