Allergic arthritis is an inflammatory reaction in joint tissues that occurs as a result of the body's response to any substances or bacteria. The pathology is provoked by an allergen, which can be an object, medication, bacteria, wool or food. Mostly allergic arthritis manifests itself in one of the joints, but often progresses, involving new cartilage tissue and turning into polyarthritis. Both children and adults are equally susceptible to the disease.
Infectious allergic polyarthritis
- home
- Diseases
- Infectious-allergic polyarthritis: what it is, causes, symptoms and treatment
Arthritis is an inflammatory disease of a joint.
If the inflammatory process affects two or more joints, doctors use the term “polyarthritis.” One of the varieties of this disease is infectious-allergic polyarthritis. Its essence lies in acute inflammation of the tissues located near the joints, accompanied by their swelling due to the accumulation of a large volume of fluid.
This is a completely reversible process, it does not destroy joints, does not impair their mobility and does not cause disability. Unlike other types of arthritis, the disease ends with complete recovery, although it has a tendency to relapse.
Precautionary measures
The best way to protect yourself from arthritis recurrence is to follow these basic guidelines:
- when going to the hospital, be sure to warn doctors and nurses about the presence of allergies to certain substances;
- It is important to avoid the allergen as much as possible: do not use drugs with an irritant, exclude them from food and everyday life. If contact with the allergen is mandatory and cannot be avoided, antihistamines are used;
- maintaining a high level of immunity;
- maintaining a healthy lifestyle;
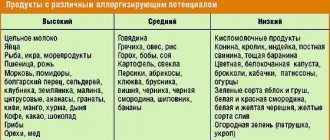
- adhere to a diet that excludes: canned food, smoked foods, fatty and spicy foods. Fruits and vegetables rich in minerals, vitamins and other beneficial microelements are added to the diet.
- avoiding excessive physical activity.
Allergic arthritis has specific symptoms, since the symptoms worsen after ingestion of the allergen. Mostly, the doctor is able to quickly determine the type of disease. Correct diagnosis is the key to selecting the best treatment regimen. If all the doctor’s orders are followed, the patient has a favorable prognosis for a full recovery.
Causes of the disease
The impetus for the development of inflammation is an allergic reaction of the immune system to the entry of pathogens into the body. They can be pathogens of bacterial and viral infections. The most aggressive allergens include staphylococci and streptococci.
Thus, the development of the disease is influenced by two factors: the entry of an infectious agent into the body and the subsequent occurrence of an allergic reaction. They determine the name of this form of arthritis.
Modern studies have revealed a clearly visible relationship between infectious-allergic polyarthritis and infectious diseases of the respiratory system. Usually the disease begins after tonsillitis, sinusitis, pharyngitis and other respiratory tract infections.
But not all people who have had the infections listed above have joint problems. There is reason to believe that the development of the disease is possible only if other unfavorable factors are added: genetics, weak immunity, changes in hormonal levels.
In general, the clinical picture is not much different from the manifestations of ordinary arthritis and has the following characteristics:
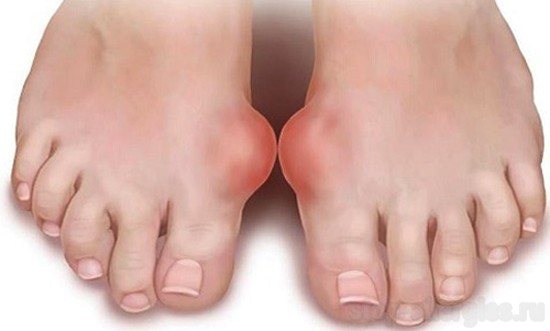
- Swelling of the joints.
- Redness around the joints.
- Itching.
- Painful sensations, especially pronounced when moving.
- Increased body temperature.
- Sometimes there is difficulty breathing.
- A blood test determines the presence of antibodies to infectious agents and increased levels of ESR and leukocytes.
After 10-14 days, all symptoms disappear, even if no treatment has been carried out. Laboratory tests also do not reveal any abnormalities. However, in the case of a new infection, there is a high probability of relapse.

Treatment
Treatment is carried out comprehensively, the basis of treatment is complete cessation of contact with the allergen.
Inflamed joints require complete rest. They are softly bandaged to give the correct physiological position. Dry heat and compresses with analgesic liquid ointments are prescribed. If the effusion accumulated in the cavity slowly resolves or inflammation and pain do not go away for a long time, then more active thermal treatment is carried out: paraffin treatment, ozokerite treatment, peat applications, diathermy courses.
General treatment of an allergic reaction is also carried out in parallel. Antiallergic antihistamines are prescribed: Suprastin, Zyrtec and others. Nonsteroidal anti-inflammatory drugs relieve swelling, reduce pain and inflammation, but their use is contraindicated for people who suffer from peptic ulcers or have had them in the past. According to strict indications, glucocorticoid hormonal drugs are prescribed orally, which effectively fight inflammation and enhance the effectiveness of analgesics.
If the general allergic reaction is excessively expressed (blood pressure is reduced, the person loses consciousness or swells, begins to choke), it is necessary to immediately call an ambulance, and then any manifestations and treatment of arthritis fade into the background.
Remember that if you have ever had arthritis due to any allergen, then if you come into contact with it again, there is a high probability of joint inflammation occurring in a more severe form.
- Author: Marina
Rate this article:
(13 votes, average: 3.3 out of 5)
Popular materials from the section - General Medicine
Once upon a time, the advent of X-rays made a real revolution in the field of diagnostics. Decades have passed, and this examination method is no longer the most progressive. X-rays have been replaced by safer and more informative diagnostic procedures...
In radio wave surgery, the American device, Surgitron, is widely used. This radio knife allows you to remove various tumors without traumatizing surrounding tissues...
Medical reform Suprun 2020. What to expect from the new medical reform in Ukraine? How much will the quality of medicine improve and what are the advantages of online medicine for Ukrainians? Read here...
Human behavior directly depends on hormones. To understand the basic concept of people’s behavior in a given situation, you need to get to the very essence of the processes occurring in the body...
Oral and maxillofacial surgery is a kind of lifeline for those who have suffered a facial injury or have congenital and/or acquired not entirely desirable features of the face or oral cavity….
Treatment of influenza includes symptomatic treatment (fever reduction and pain control, hydration), as well as antiviral treatment and immunity boosting….
Poor nutrition, overeating, bad habits - all this can negatively affect the functioning of the intestines and other digestive organs. Because these internal organs work both day and night to remove toxins from the body….
Any deviations in the appearance of nails are a signal of a health problem. The most common problem is brittle nails. In this article we will look at ways to deal with this nuisance...
Surely, many have heard the word “osteopathy”. However, not everyone knows its essence and meaning. And this is very bad, because it means a unique technique for diagnosing and improving the health of the human body...
Hemorrhoids are a common disease. It occurs in men, women and even children. The disease can be treated well, the main thing is to choose the right drug. And there are no problems with this today - there are enough drugs on the shelves of pharmacies...
Sometimes our body reacts inappropriately to various antigens, which subsequently leads to allergies. It turns out that an allergic reaction can manifest itself not only with a runny nose, rashes and asthmatic symptoms, but also with joint inflammation.

This pathology is called allergic arthritis. Arthropathy of allergic origin has become diagnosed much more often. This pathology is especially common in people suffering from atopy (hereditary tendency to allergic reactions), chronic forms of joint pathologies, women, and children.
As a result of an immune reaction to the antigen, a subacute or acute inflammatory process develops in the tissues of mainly large joints. In other words, such arthritis appears in the form of an allergic reaction.
Factors influencing the development of pathology
The main cause of allergic arthritis is an immune disorder, which can be caused by any allergenic substance such as wool, pollen, household chemicals, medications, dust or dust mites. When an allergen substance enters the body, the immune system begins to produce special antibodies for protection. If any disruption occurs in immune activity, protein antibodies begin to accumulate in the joint tissues, provoking the development of inflammatory processes.

If a person prone to allergies suffers from chronic joint pathologies, then he is included in the risk group for developing allergic arthropathy. Recent years have been characterized by a steady increase in allergy sufferers, which is associated with low-quality products that contain various additives and preservatives that increase the body’s allergenic sensitivity.
An allergic reaction can occur even from familiar foods if the immune defense is weakened. There are cases where allergic arthropathy occurred as a result of hypothermia, physical overexertion or stress.
Allergic arthropathy can develop:
- Due to a reaction to a food allergy;
- Against the background of medical interventions such as antibiotic therapy, administration of serum or any injection, taking painkillers;
- Allergic reactions to household chemicals or cosmetics;
- Reaction to animals, their fur or secretions;
- Constant contact with chemicals, especially those whose activities are related to pharmacology or the petrochemical industry, are especially at risk of developing allergic arthritis.
Signs of allergic arthritis
The pathology is usually characterized by acute and lightning-fast development, immediately after the penetration of an allergenic substance into the body, but long-term development is also possible, although this happens extremely rarely. Allergic arthropathy develops when the allergen comes into repeated contact with the body, since during the first contact the immune system became familiar with the allergenic agent and developed antibodies against it. In other words, upon first contact, an immune response was formed.
In general, allergic joint inflammation is characterized by the following symptoms:
- Large joints are usually targeted;
- The soft tissues around the lesion suddenly swell, the surface of the skin turns red and becomes hot;
- Pain appears during palpation or physical activity, intensifying after rest;
- General health worsens, weakness, depression, and lethargy appear;
- Skin rashes, itching or hives characteristic of allergies;
- Other allergic symptoms such as bronchospasms, Quincke's reaction or angioedema, bronchial asthma, atopic dermatitis;
- Allergic arthritis is often accompanied by rhinoconjunctival symptoms - itching, tearing and other signs of inflammation of the ocular mucosa;
- Uncharacteristic symptoms such as tachycardia, diarrhea, nausea and vomiting, hyperthermia.
Options for the development of pathology
The course of allergic arthritis is defined as a typical inflammation of the synovial joint membrane. It occurs according to all the rules for the development of an allergic reaction. Inflammation may appear immediately or will make itself known a couple of days or a week after the allergen has had an impact. The first signs of allergic arthropathy resemble symptoms of a cold - fatigue appears, the heart rate increases, lacrimation appears, and the temperature begins to rise. Then pain appears in the joint tissues, and urticaria appears on the body. Then the rest of the above symptoms develop.

A similar picture can be observed over a couple of days. At times, it goes away spontaneously when the allergen stops penetrating the body. This factor distinguishes this form of arthritis from other arthropathies.
If contact with the allergen continues, then relapses of inflammatory and allergic processes are observed. In isolated cases, long-term allergic arthropathy may develop, which is most typical when exposed to drugs. Then the patient experiences severe pain, pronounced inflammatory symptoms, and an accumulation of exudate may begin in the joint tissues.
Sometimes allergic arthropathy develops in a slightly different form, acquiring an infectious-allergic nature. The reason for this is:
- Infectious factor. This includes genitourinary, intestinal, and respiratory infections caused by streptococci, Pseudomonas aeruginosa, staphylococci, etc.
- Pathologies of a severe nature. These include tuberculosis, diabetes, brucellosis. A separate category includes arthritis of gonorrheal origin, which is also a variant of the infectious-allergic form of joint inflammation.
Therapy methods
The therapy takes an integrated approach, where the main principle is the absolute exclusion of further contact with the allergen substance. It is recommended to gently bandage the joints, giving them a physiologically correct location. In general, the therapeutic process is based on the following principles:
- Taking anti-allergy antihistamines like Suprastin, Diazolin, Allercaps, Diphenhydramine, etc.;
- In case of acute arthropathy, analgesic drugs like Baralgin, Spazmolgon and anti-inflammatory drugs are prescribed - Meloxicam, Ibuprofen, Diclofenac, Ketoprofen, etc.;
- The use of chondroprotective drugs that form cartilage tissue and provide a sufficient level of synovial fluid. These medications are especially recommended for the development of recurrent arthropathy;
- If allergic arthropathy is characterized by a severe course, then hormonal medications from the group of corticosteroids and glucocorticoids are additionally prescribed;
- If the provoking agent, in addition to the allergen, is also an infectious agent, then weekly antibiotic therapy with Erythromycin, Amoxicillin or a drug to which the agent is particularly sensitive is indicated;
- Local treatment with ointment or gel preparations - Indomethacin, Rumakar, Fastum-gel, Cinepar, Dolgit, etc.
Arthropathic symptoms are usually easy to relieve, provided that treatment is prescribed in a timely manner and taking into account the characteristics of the pathology. Timely therapeutic measures and accurate execution of all medical prescriptions ensure a positive, lasting result. To avoid developing arthritis in the future, precautions must be taken. If the patient follows preventive recommendations, the prognosis of anti-arthritic therapy will be positive.
Allergic arthritis is an inflammatory allergic benign lesion of the joints, which occurs as a reaction of the body to various antigens, and has a completely reversible nature of the lesion. Thus, it is arthritis that occurs as a manifestation of a general allergic reaction.
Children are more susceptible to the disease. Usually occurs in people who have a tendency to develop allergies.
Arthritis can develop under the influence of a wide variety of allergens: medicinal, food, pollen, animal hair and others.
It occurs as an acute or subacute inflammation of the joint.
This type of arthritis is easily reversible, but relapses of the disease can often occur (if the allergen enters the body again or with “undertreated” allergic arthritis).
Allergic arthritis should not be confused with infectious-allergic arthritis. Infectious-allergic arthritis is one of the names of reactive arthritis. In reactive arthritis, no inflammatory substrate is found, while allergic arthritis occurs as a result of the accumulation of immune complexes, antibodies and other agents in the joint tissues.
Arthritis that occurs as a result of certain infectious and viral diseases (hepatitis B, rubella and others) also have an allergic mechanism of occurrence; they are described in detail in the section on infectious arthritis.
Pathogenesis of allergic arthritis
It is based on the body’s increased sensitivity to foreign substances (medicines, serum, food products, etc.).
As a result of allergens entering the body, antibodies begin to be produced against them, which subsequently combine with the foreign substance. Due to various defects of the immune system, these complexes are deposited in various tissues of the body, including the joints. Then a nonspecific inflammatory process occurs around them, and symptoms of arthritis appear. This mechanism works, for example, after the administration of certain medicinal serums (for example, antitetanus).
Another mechanism for the occurrence of allergic arthritis is the ingestion of haptens into the body. Haptens are substances that do not independently cause any pathological reactions, but when they enter the body, they can combine with other agents (for example, blood plasma or tissue proteins), and the substances thus obtained have the properties of allergens. This mechanism for the development of arthritis is characteristic, for example, of some medications.
Currently, reactions involving immunoglobulins E (IgE) and their role in the formation of allergic arthritis are being actively studied.
Symptoms of allergic arthritis
- the onset of the disease is usually acute - almost immediately after the allergen enters the body, less often - gradual (up to 4-12 days);
- usually develops after the allergen re-enters the body (since after the first hit an immune response against this substance should have been formed);
- characterized by damage to large joints;
- pain during movement, palpation, increasing after rest;
- sharp swelling of the joint, the soft tissues over it are hyperemic, warm to the touch;
- there may be itching, hives or an allergic skin rash;
- Rhinoconjunctival syndrome often occurs (lacrimation, itching and other manifestations of conjunctivitis);
- other manifestations of allergies (Quincke's edema, bronchospasm, angioedema) or exacerbation of chronic allergic pathology (atopic dermatitis, bronchial asthma);
- often – nonspecific symptoms (fever, tachycardia, nausea, vomiting, diarrhea and others).
Diagnosis of allergic arthritis
First of all, allergic arthritis is differentiated from reactive or infectious arthritis, since it has a similar acute course.
In most cases, making a diagnosis does not cause difficulties, because There is a clear connection between the entry of an allergen into the body and the development of arthritis.
The patient's allergic history also helps to make a diagnosis: the presence or absence of drug and food allergies, hay fever, bronchial asthma and other diseases.
In general blood tests, there may be an increase in the level of eosinophils (which usually does not happen with other types of arthritis), leukocytes, a slight acceleration of ESR (up to 20-25 mm/h, while with other types of arthritis, ESR accelerates to 35-40 mm/h) h and above).
According to the results of x-rays of the joint, no pathological changes are usually found, since this type of arthritis does not cause destruction of bone tissue.
Since changes in allergic arthritis are represented by swelling of soft tissues and the presence of effusion into the joint cavity, the main diagnostic method in this case is ultrasound examination of the joint. Swelling of the soft tissues of the joint, bursitis and synovitis are noted. Characterized by expansion of the articular cavity, the presence of effusion and sediment (suspension) in the joint fluid (i.e., it becomes heterogeneous, cloudy).
In difficult cases, a diagnostic puncture of the joint may be necessary, and eosinophils, specific immune complexes, and antibodies are found in the puncture.
Acute form of allergic arthritis
It is characterized by a more pronounced pain syndrome, accompanied by severe swelling and hyperemia of the articular tissues, and effusion into the joint cavity. Usually several joints are affected at once.
This form is accompanied by other pronounced phenomena of allergic reactions (Quincke's edema, exacerbation of bronchial asthma and others).
According to the results of ultrasound, significant swelling of the articular tissues, effusion in the joint cavity, and often the phenomena of bursitis and synovitis are determined.
All manifestations of acute allergic arthritis quickly stop with properly prescribed therapy.
Subacute (protracted) allergic arthritis
This form is less common, develops gradually and is more severe.
More often occurs under the influence of a drug allergen.
The pain is severe and usually requires the use of painkillers and hormonal medications. In the most severe forms, it is even possible to develop irreversible changes in the joint - the appearance of foci of necrosis of the articular ends, deformation of the surfaces of the joint.
Principles of treatment of allergic arthritis
- exclusion of the allergen;
- rest of the affected joint;
- antihistamines;
- hormonal drugs (for severe allergy symptoms, ineffectiveness of antihistamines);
- non-steroidal anti-inflammatory drugs (for pain relief).
Since the symptoms of arthritis usually disappear quickly and without a trace immediately after the start of therapy, there is no need for additional treatment methods (physiotherapy, exercise therapy, etc.).
Allergic arthritis - prognosis
Favorable. Basically, the disease is acute, the symptoms of arthritis quickly stop after the start of treatment. Rarely, the course is subacute, but even in this case, the inflammation is usually easily reversible immediately after starting therapy.
Prevention
Prevention of allergic arthritis - preventing re-entry of the allergen into the body. In the presence of allergic diseases, observation by an allergist-immunologist is indicated. If a person with an allergy does need to be given some kind of medicine (for example, an antibiotic), it is usually taken along with antihistamines.
If an allergic reaction in the form of arthritis has previously been noted to any antigen, then upon subsequent administration it usually occurs in a more severe form!
Doctor
Features of the disease in children and adults
Among adult survivors, there was a large percentage of young people, 75% of whom were women. Unfortunately, the disease tends to affect children as well. Infants are at high risk of becoming infected from their mother.
In children, the disease occurs in acute or subacute form with minor or moderate pain. Among other signs, skin rashes may appear, as well as an increase in the number of neutrophil granulocytes in blood tests. The child has no appetite, he is capricious all the time, complains of pain in the limbs, tries to move less and is reluctant to pick up objects and toys. Otherwise, the clinical picture is the same as in adults.
Types of headaches
If a person has a headache and does not know what the reason is, he needs to consult with many doctors: an otolaryngologist, an allergist, a neurologist, a surgeon, an orthopedist, an ophthalmologist and a dentist. The doctor will send the patient to undergo numerous tests and diagnostics to determine why the severe migraine occurred.
Headache is divided into two types: primary (occurs in 90-95% of cases), symptomatic or secondary (probability of occurrence is 5-10%).
Primary headaches include muscle tension headaches, sharp and cluster headaches, and migraines. Secondary pain is a symptom of a disease, for example, a brain tumor, vascular pathology of the brain, traumatic brain injury, allergies.
In the first case, the patient should take analgesics that will prevent the development or occurrence of migraine. Medicines reduce the intensity of pain. In case of symptomatic pain, it is worthwhile to treat the underlying disease as the cause of severe headache.
Diagnostics
Only an experienced doctor can make a correct diagnosis, since a number of diseases have a similar clinical picture, among which infectious-allergic polyarthritis is less common than other externally similar conditions. Its result should exclude ankylosing spondylitis, psoriatic and rheumatoid arthritis, and intermittent hydrarthrosis. Similar manifestations can also be observed with gout and borreliosis.
In order to ensure the most accurate diagnosis, studies such as blood tests, urine tests, synovial fluid tests, tests for tuberculosis, dysentery and other infections are carried out, ultrasound and x-ray examination of joints are prescribed.
Etiology and pathogenesis
Etiol, factors I.-a. There may be different microorganisms, but the leading role belongs to streptococcal infection.
As evidence of the participation of streptococcal infection in the development of I.-a. pp. provides evidence of a connection between the onset of the disease and a previously suffered sore throat or with an exacerbation of hron, tonsillitis, sinusitis, etc., as well as a persistent increase in anti-streptococcal antibodies. It is assumed that streptococcal infection, if there is a predisposition, can lead to the development of an allergic reaction in the form of synovitis (see).
Attention is drawn to unfavorable heredity: in families, almost 2/3 of patients with I.-a. rheumatism, bronchial asthma and other diseases of an allergic nature occur.
How to treat
For effective treatment, it is necessary to wage a war against the disease on three fronts at once:
- Suppression of infection.
- Relieving an allergic reaction.
- General improvement of health and increased immunity.
Antibiotics are used to fight pathogenic bacteria and viruses. Penicillins are considered the most effective here . If there are problems with their tolerability, then it is possible to replace them with drugs of the erymitromycin series.
To prevent the development of rheumatoid arthritis, you should take a prophylactic course of quinoline drugs. For the overall strengthening of the body, taking multivitamins is very important.
After completion of the acute phase, physiotherapeutic procedures are very useful: ultraviolet irradiation, diathermy, paraffin baths. During this same period, physical therapy is indicated.
Treatment usually takes 1-2 months. But if relapses do not stop and complications arise, surgery may be necessary.
Traditional medicine in the presence of this disease is ineffective and is fraught with complications. Qualified medical care is needed here.
Massage and exercise therapy
When the above measures provide an effect, procedures will be necessary to restore the normal functioning of the body:

In addition to medications, traditional medicine is also used to treat arthritis.
- Physical therapy (necessarily under the guidance of an experienced specialist) helps develop the joint.
- Dosing loads reduces the risk of injuries to weakened ligaments and muscles.
- Massage in the area of affected joints stimulates blood supply to tissues, promoting rapid regeneration.
Prevention
First of all, to minimize the likelihood of infectious diseases of the respiratory tract, you need to strengthen your immune system. This is facilitated by taking multivitamins.
In order to prevent allergies, a number of foods should be excluded from the diet: fatty foods, ice cream, red and orange vegetables and fruits.
People who have had infectious-allergic polyarthritis, after recovery, need to undergo a thorough examination to exclude hidden infection. To prevent relapses, prophylaxis in sanatorium-resort conditions is very useful. Sea, hydrogen sulfide and radon baths are recognized as the most effective preventive methods.
Clinical picture
I.-a. It is predominantly women who are affected. The onset of the disease in almost all patients is before 40 years of age, and in 3/4 of them - before 30 years.
The first symptoms of I.-a. p. most often occur 7-14 days after exacerbation of the focus of streptococcal infection, however, a shortening of this interval to 5-7 days or the development of arthritis during streptococcal infection is often noted. The disease usually begins acutely, less often subacutely. Joint pain appears, often worsening with movement, and swelling. Involvement of several joints, both large and small, often occurs simultaneously. In severe cases, an increase in skin temperature and redness may also be observed in the joint area. Joint movements are limited due to pain, less often due to exudative changes in the joints.
Changes in the joints disappear without a trace after 4-6 weeks. from the start of treatment, and their function is completely restored. In some cases, after a certain period of time (from 2 months to several years), relapses of the disease are observed, sometimes very frequent, which also end in a complete wedge, recovery without residual effects from the joints. The heart and other internal organs remain intact.
Laboratory parameters of peripheral blood (acceleration of ROE, leukocytosis), as well as immunol and biochemical tests (ASL-O, ASG, DPA, seromucoids, protein fractions of blood) deviate significantly from the norm only in the acute version of the disease. They are under the influence of treatment for 1-2 weeks. are normalized. During remission, all reactions to the presence of an inflammatory process are negative.
The diagnosis presents serious difficulties and is established taking into account the wedge, picture and laboratory data. X-rays of the joints are without patol, changes, sometimes you can detect widening of the joint spaces due to significant effusion in the joint. ECG and FCG without visible changes. I.-a. items should be differentiated primarily with rheumatic arthritis (see Rheumatism) and the initial stages of rheumatoid arthritis (see). Simultaneous damage to several joints against the background of infection or following it, the absence of “volatility”, somewhat greater persistence during the course, the relative duration of the articular syndrome, the intactness of the heart, a lesser effect from salicylates and the simultaneous disappearance of changes in the joints distinguish I.-a. n. from rheumatic. An important differential diagnostic criterion is the absence of I.-a. etc. signs of carditis and the development of heart defects even after several attacks. Unlike rheumatoid arthritis, I.-a. p. has a benign course, despite frequent relapses, and always ends in complete restoration of the appearance and function of the affected joints. With I.-a. there is no rentgenol. changes that are so characteristic of rheumatoid arthritis, although they may also be absent in the early stages of rheumatoid arthritis. In such cases, only dynamic observation allows a correct diagnosis. Test for rheumatoid factor in patients with I.-a. n. is always negative (see Rheumatoid factor).
Read also: Gymnastics for fingers for arthritis
Certain difficulties may arise when differentiating I.-a. with allergic arthritis in various infections and with specific arthritis. However, in these cases, signs of the underlying disease are found.
Treatment of the acute period of the disease consists of influencing the foci of chronic infection and eliminating sensitization of the body. To combat focal infection, antibiotics from the penicillin group and erythromycin are used; if there is intolerance to antibiotics, sulfonamides can be used.
Antimicrobial therapy is carried out under the guise of desensitizing agents. Therapy with salicylates is pathogenetic. Acetylsalicylic acid is recommended; if the patient has hypersensitivity to it, pyrazolone derivatives are recommended. In some cases, in acute cases of the disease, an accelerated course of treatment with prednisolone is carried out. Long-term, up to 1 year, use of quinoline drugs is also recommended to prevent the development of rheumatoid arthritis.
To prevent repeated attacks, complete sanitation of foci of infection is necessary.
From the very beginning of the disease, gentle treatment is recommended. gymnastics and physiotherapy - ultraviolet irradiation of the affected joints. After eliminating exudative changes in the joints, thermal procedures are recommended - diathermy, inductothermy and paraffin; shown san.-kur. treatment at resorts with hydrogen sulfide, radon or salt baths.
I.-a. n. completely curable.
Infectious allergic polyarthritis
Infectious-allergic arthritis is manifested by acute inflammation of the tissues adjacent to the joints (synovial membranes), which occurs due to the accumulation of large amounts of effusion in them. The disease is known for its tendency to relapse. More often the disease affects young women, but it also occurs in men and even children.
For this disease to occur, an infectious pathogen must penetrate the body, leading to allergization and inflammation in the joints. Accordingly, there are two reasons for the development of the disease: infection plus allergies.
The term "arthritis" is used when one joint is affected. But if the inflammation affects two or more joints, then the disease is already called infectious-allergic polyarthritis (translated from the ancient Greek “poly” - many).
Causes of allergic reactions in the throat
Your throat can hurt for a huge number of reasons, which means you shouldn’t immediately run to the pharmacy and self-medicate.
First, you need to carefully observe how you feel and try to determine the reasons for such feelings. Perhaps the pain is associated with eating hot or spicy foods that irritate the mucous membrane of the scalp. Sometimes, from excessively loud communication, pain appears from tired vocal cords, and a cold may actually occur. Allergies can be caused by smoke from a fire or cigarettes, or by pollen or dust; there are even allergies to cold.
Allergy manifests itself in the form of inflammation of the mucous membranes of the respiratory tract (swelling is possible), inflammation of the mouth and eyes. This is why pain is felt during swallowing. The surest sign of the difference between a cold and an allergy is the frequency of the disease. If a person gets sick many times during the year, then we can say for sure that this is a manifestation of an allergy.
Possible reasons
For a disease to occur, an organism that has an inferior immune system must be exposed to some infectious pathogen. This leads to the formation of a large amount of harmful substances, leading to the development of inflammation.
In essence, infectious-allergic arthritis is a delayed immunoallergic reaction of the body to any pathogenic pathogens.
Almost all types of pathogenic microorganisms can act as causative agents of the disease: various viruses, bacteria, intestinal and specific infections.
Signs of allergic arthritis
The pathology is usually characterized by acute and lightning-fast development, immediately after the penetration of an allergenic substance into the body, but long-term development is also possible, although this happens extremely rarely. Allergic arthropathy develops when the allergen comes into repeated contact with the body, since during the first contact the immune system became familiar with the allergenic agent and developed antibodies against it. In other words, upon first contact, an immune response was formed.

In general, allergic joint inflammation is characterized by the following symptoms:
- Large joints are usually targeted;
- The soft tissues around the lesion suddenly swell, the surface of the skin turns red and becomes hot;
- Pain appears during palpation or physical activity, intensifying after rest;
- General health worsens, weakness, depression, and lethargy appear;
- Skin rashes, itching or hives characteristic of allergies;
- Other allergic symptoms such as bronchospasms, Quincke's reaction or angioedema, bronchial asthma, atopic dermatitis;
- Allergic arthritis is often accompanied by rhinoconjunctival symptoms - itching, tearing and other signs of inflammation of the ocular mucosa;
- Uncharacteristic symptoms such as tachycardia, diarrhea, nausea and vomiting, hyperthermia.
Symptoms of the disease
Typically, manifestations of the disease begin 10-14 days after a person has had any infectious disease. Infectious-allergic arthritis begins with the appearance of signs of inflammation in the joints:
- increased body temperature;
- pain in the joints, which intensifies with the slightest movement (from the accumulation of intra-articular fluid);
- stiffness in movement and tension in the periarticular muscles due to pain;
- swelling, redness, and warmth around the joints;
- allergic skin rashes.
Often the disease occurs after such banal diseases as tonsillitis, ARVI or bronchitis. Both small and large joints can become inflamed. The knee and ankle joints are often affected. The illness lasts from 1 to 6 months. The patient's condition is usually satisfactory. Often, within two weeks of treating the disease (and even without it), the symptoms disappear, the pain goes away and movement in the joints is restored. This polyarthritis does not affect the heart, which is typical for rheumatism. Relapses of the disease occur after another infection or simple hypothermia.

general information
This is accompanied by swelling of the legs, which is caused by allergies, severe pain and changes in the skin. In order to relieve swelling, it is recommended to take an antiallergic drug.

A qualified specialist will tell you what kind of medicine you need to take in order to remove swelling of the legs caused by allergies. Then the doctor must prescribe appropriate treatment for the patient.
Children at risk
Allergic arthritis in children occurs from infancy. Diagnosing this disease in children is much more difficult, since they often cannot explain what is bothering them and are simply capricious. The causes of this disease in children may be:
- past infectious diseases;
- hypothermia;
- reduced immunity;
- injury;
- lack of vitamins.
It is important to start treating your baby in a timely manner, otherwise he may subsequently suffer from this disease for the rest of his life. After recovery, you should carefully monitor the child’s well-being and get tested to prevent a relapse.
Is joint pain possible with ureaplasmosis?
It would seem, what effect of ureaplasma on joints can there be in principle? After all, ureaplasma is a pathogenic causative agent of an infectious disease of the genitourinary system. However, it is this microorganism that can cause reactive arthritis, of such a complex form that a person becomes disabled in a fairly short period of time.

Diagnostic measures
Typically, the diagnosis of infectious-allergic arthritis does not cause any particular difficulties. However, a distinctive (differential) diagnosis from other similar forms of arthritis (traumatic or urogenic, rheumatic fever, gout) is required.
The doctor summarizes the data on symptoms that have specific patterns for this disease.
To correctly diagnose infectious-allergic arthritis, the following research methods are used:
- clinical blood test (to determine ESR and leukocyte count);
- biochemical blood test with rheumatic tests (C-reactive protein, sialic acids, seromucoid);
- Ultrasound of the affected joints (to determine the fluid inside it);
- radiography of joints (to determine the degree of cartilage destruction);
- if necessary, perform a joint puncture (to study the effusion).

Prognosis of the course of the disease
Despite the rather unpleasant symptoms, the prognosis for the course of the disease is usually favorable:
- The acute stage lasts from 2 to 4 weeks.
- Relieving symptoms allows the patient to more easily tolerate joint inflammation.
- With adequate therapy, arthritis is completely cured without the formation of residual changes.
The main factors for successful treatment are timely treatment and compliance with the doctor’s recommendations. Without proper treatment, the disease can become chronic (from 2 months to six months with periodic relapses). The result is highly likely to be irreversible changes in the structure of the affected joint.
Healing procedures
Typically, treatment of the disease is carried out comprehensively and includes the following stages:
- pathogen control;
- relief of allergic manifestations;
- general strengthening of the body.
For these purposes, the following types of therapy are used:
- Antibiotics, often broad-spectrum (ceftriaxone, ciprofloxacin, amoxiclav, sumamed, etc.) They are used even if the causative agent of the disease is a virus, in order to prevent pathogenic microflora from multiplying with reduced immunity.
- Antihistamines to eliminate allergic reactions (loratadine, tavegil, suprastin).
- Non-steroidal anti-inflammatory drugs to alleviate the patient's suffering and relieve the manifestations of inflammation (movalis, diclofenac, nimesil).
- Hormonal anti-inflammatory drugs (dexamethasone, prednisolone).
- Immunity-boosting substances in the form of interferon preparations (cycloferon, laferon, viferon).
- Intra-articular administration of drugs to relieve inflammation and allergic reactions (diprospan).
- The use of physiotherapy on affected joints (UHF, electrophoresis, ultraviolet irradiation, paraffin wraps), physical therapy.
- Taking multivitamins and a diet that excludes fatty foods, colored fruits (orange and red), and chocolate.
- Sanatorium-resort treatment using baths (sea, radon, hydrogen sulfide).
In case of irreversible destruction of the cartilage tissue of the joint, reconstructive operations are used. After treatment, it is advisable to be examined and identify hidden sources of infection in the body.
For those who have had infectious-allergic arthritis at least once, the threat of recurrence of the disease remains relevant. Such a person needs to take care of his health and strengthen his immune system, avoiding in every possible way the development of infectious diseases.
Take care of your body and be healthy!
ethnoscience
Drug therapy together with physiotherapeutic procedures can be supplemented with traditional methods of treatment. These techniques allow you to relieve a significant part of the symptoms, stimulating the body's natural regeneration processes.
Sea bath
The best sea bath for joints is the sea. But if there is no opportunity to visit the resort, proceed as follows:
- Prepare a salt bath - approximately 1 kg of salt (preferably sea salt) per 10 liters of water.
- The water should be hot enough (from 40 degrees).
- The procedure time is from 15 minutes.
It is advisable not to immerse yourself completely in the bath, but to expose only the affected joints.
Vodka and mustard compress
If the disease cannot be cured completely, then at least compresses can help alleviate the condition. Here is one of the most effective recipes:

There are several most famous compress recipes
- Add 200 g of table salt to 500 ml of unflavored vodka.
- Add 100 g of strong mustard to the solution and leave for 7 days in a dark place.
- We apply the product to a linen bandage that we wrap around the joint. We wrap a layer of polyethylene on top.
- The duration of one procedure is up to 8 hours (but you need to ensure there are no burns).
Decoction of cherries and milk
To stimulate the human immune system and more effectively fight infection, we prepare the product according to the following recipe:
- Add 200-250 g of pitted cherries to 1 liter of whole pasteurized milk.
- Boil for 5-7 minutes over low heat.
- Store the cooled broth in the refrigerator. It should be taken 3 times a day, 1-2 tablespoons.
Propolis tincture
Despite the fact that bee products can be strong allergens, they are actively used in the treatment of allergic arthritis.
If there are no contraindications, you can prepare a propolis tincture:
- Add 15–30 g of propolis to 250 ml of drinking or medical alcohol.
- The composition is infused in a dark place for 5–7 days.
- The product should be taken on an empty stomach, 15 ml.
- The optimal duration of treatment is 14 days.
Infectious allergic polyarthritis
Most people do not imagine what upper respiratory tract diseases can lead to. One of the complications is infectious allergic polyarthritis.
Arthritis is inflammation in one area of a specific joint. If the pathological process covers more than two joints, then the prefix poly (multiple) is used. Thus, there are several types of polyarthritis.
An infectious-allergic type of polyarthritis is an acute inflammatory process of tissues adjacent to the joints (synovial membranes). These tissues swell due to the accumulation of a large amount of fluid in them, that is, effusion.
Inflammation is the body's aggressive response to an invading infection.
Can organs and parts of the human body hurt due to allergies?
Allergic reactions may be risk factors for developing chronic fatigue syndrome. It is a complex and debilitating disease that affects different parts of the body, with symptoms including poor sleep, weakness and pain in muscles and joints, headaches, and problems with concentration and memory.
Many people diagnosed with chronic fatigue syndrome have an oversensitive immune system, and often both conditions (CFS and allergies) occur at the same time. Environmental irritants (such as mold spores) and food allergies often contribute to the condition.
Coughing and sneezing during allergies can also cause pain, which is caused by tension in the back muscles and abdominal muscles. In general, when a person comes into contact with allergens, the entire immune system experiences inflammatory processes involving the sinuses, skin, respiratory tract, and joints.
The body works hard to get rid of external allergens, essentially exhausting itself, which leads to joint pain, back pain, neck pain and headaches.
Specifics of the disease
As a rule, such infections are staphylococci and streptococci; they are the strongest allergens for the immune system.
Thus, an infectious allergic type of polyarthritis is formed. Currently, the infectious allergic type of polyarthritis has not been thoroughly studied, but scientists have identified a clear relationship between this disease and respiratory tract infections.
The disease appears after diseases such as:
- tonsillitis,
- angina,
- sinusitis,
- pharyngitis.
It is not completely known why the joints do not begin to be affected in all people who have suffered a staphylococcal or streptococcal respiratory infection.
Modern medicine believes that for the development of arthritis to begin, several additional factors are needed:
- allergies specifically to these pathogens (which provokes allergic polyarthritis),
- weak immunity,
- hormonal dysfunctions,
- genetic predisposition.
Relatives of a large number of people who have polyarthritis suffer from rheumatism and asthma. It is worth emphasizing that these diseases are allergic in nature.
An important feature of the disease is that it is benign, that is, it cannot lead to joint deformation, limited mobility or disability. In this way, the infectious allergic type of polyarthritis is fundamentally different from infectious arthritis or rheumatism.
The disease appears and symptoms actively develop, but then it stops and disappears without a trace. Therefore, there is often no need to hospitalize a person. However, it is worth noting that this type of polyarthritis is characterized by relapses.
Many people believe that polyarthritis occurs only in older people. This is a misconception. It is known that women under 40 years of age suffer more from this disease. About 75% of the total number of patients are women.
To a large extent, polyarthritis is common in children. Parents should protect their child from viral and cold infections, and immediately begin treatment as soon as the child begins to complain of symptoms such as discomfort in the bronchi or sore throat.
What allergic diseases cause pain?
When talking about food allergies, shoulder pain or knee pain are not the symptoms with which it is associated. However, for people who have arthritis or other inflammatory joint diseases, food allergies can cause pain (due to inflammation).
Symptoms do not appear immediately, but may develop a day after consuming certain foods that cause allergic reactions. Sunflower seeds, walnuts, cashews, coconut and pineapple, but especially soy, can trigger migraines.
Back, neck and joint pain, headaches can cause environmental allergies. The truth is that the joint nature of pain is inevitable due to the connection of allergic reactions with inflammation.
Almost anything, including foods, dog dander, medications, and airborne allergens can cause an allergic reaction, and symptoms range from mild to severe, causing pain in multiple organs.
Heaviness in the heart, tightness or generalized pain in the chest, difficulty breathing with wheezing, coughing are symptoms of allergic asthma, before, during and after attacks, which can lead to damage to the scalp muscles. These muscles are located on the side of the neck, attaching the cervical vertebra to the 1st and 2nd ribs. Damage to the zygomatic muscle with a strong cough causes pain in the upper chest and radiates to the arms.
Chest pain is considered an early warning sign of asthma, meaning an attack is imminent unless action is taken. Studies have shown that chest tightness may be the only symptom of asthma in some patients and a subjective symptom. This means that what a person feels cannot be assessed from the outside.
Some patients describe the pain as a dull pain, while others describe it as a sharp, stabbing, cardiac type. But chest pain is often confused with cardiovascular diseases (tightness and heaviness in the chest are not always symptoms of asthma). Many heart diseases, digestive problems, muscle and nerve disorders can also cause these symptoms.
Angina, when the heart feels like it's going to jump out, associated with asthma, often occurs during exercise or at night.
If asthma is the cause of chest pain, treatment usually begins with inhaled corticosteroids.
Can my throat hurt if I have an allergy? The symptoms of allergic reactions are very diverse. For example, allergic laryngitis is a diffuse (widespread) or local inflammation of the larynx in response to chronic or acute irritation caused by an allergic agent. Irritation leads to redness (erythema) and swelling of any part of the larynx.
The onset of laryngitis is usually sudden and the condition worsens within three days. Main symptoms: hoarse voice or loss of voice, feeling like you need to clear your throat, sore throat. The child is more difficult to tolerate the disease; a high temperature may be observed, above 38 °C, the patient refuses to drink and eat, given that it is very painful to swallow, and has difficulty breathing.
The nose and throat are lined with glands that constantly produce mucus. This mucus keeps the upper respiratory tract moist and clean, protecting against infections. Throat discomfort, which can turn into pain and affect the larynx, is the most common symptom of a pollen allergy.
Typically, when we ingest an allergen (dust or pollen) in environmental allergies, we do not notice it, but our body immediately reacts by releasing chemicals that increase mucus production, leading to excessive and irritating discharge. For some allergy sufferers, the consequence is a severe runny nose, for others, excess mucus flows into the throat - a sign of postnasal drip (postnasal drip). Sore throat with allergies symptoms:
- tickling, soreness in the throat;
- cough;
- swelling and pain, which is especially disturbing when swallowing saliva and food;
The irritation, if left untreated, can lead to a streptococcal throat infection.
Damages the surface of the eyes, causing debilitating symptoms such as itching, redness, inflammation and soreness. Pollen, animal dander (eg dog fur), and other environmental antigens are major irritants. An overreaction of the immune system causes the body to release histamine and other active substances through mast cells. The blood vessels dilate and dilate, irritating the nerve endings. The result is increased tear secretion.
Sometimes our body reacts inappropriately to various antigens, which subsequently leads to allergies. It turns out that an allergic reaction can manifest itself not only with a runny nose, rashes and asthmatic symptoms, but also with joint inflammation.

This pathology is called allergic arthritis. Arthropathy of allergic origin has become diagnosed much more often. This pathology is especially common in people suffering from atopy (hereditary tendency to allergic reactions), chronic forms of joint pathologies, women, and children.
As a result of an immune reaction to the antigen, a subacute or acute inflammatory process develops in the tissues of mainly large joints. In other words, such arthritis appears in the form of an allergic reaction.
Diagnosis of the disease
It is quite difficult to recognize this type of polyarthritis. Successful diagnosis requires extensive medical experience. Infectious allergic arthritis occurs much less frequently than diseases such as:
Doctors often mistake the above for a real diagnosis, because the symptoms of many types of arthritis and allergies are very similar. A massive attack on the disease with powerful immunosuppressants, as well as gold salt preparations, is necessary.
When making a diagnosis, it is necessary to strictly exclude several similar diseases. For example, traumatic arthritis manifests itself in exactly the same way, but it does not have an infectious origin.
A similar picture is present in intermittent hydrarthrosis, however, it does not cause either general or local temperature. Urogenic arthritis develops similarly, but they are associated with infection of the genitourinary organs. Often the same symptoms can occur with gout, rheumatic fever, and borreliosis.
To exclude similar diseases, it is necessary to apply the entire range of diagnostic studies, which includes:
- blood and urine tests,
- examination of synovial fluid,
- tests for gonorrhea, dysentery, brucellosis,
- bacterial cultures of biological tissues,
- x-ray,
- tests for tuberculosis,
- Ultrasound of joints.
The clinical picture must be taken into account, which begins to appear 1-2 weeks after the onset of a respiratory, streptococcal or staphylococcal disease.
During this period, polyarthritis has characteristic stages:
- initial symptoms
- increased allergic symptoms,
- increased inflammation in the periarticular tissues.
When does the temperature rise?
The temperature during allergies can increase when allergens of different intensity and individual tolerance affect the body. These are foodborne pathogens, intolerable medications, foreign proteins, plasma, vaccines, various insect bites, and pollen. This list of allergens is not yet complete, since there are many types of allergies in people who are prone to them.

Symptoms and course of the disease
The symptoms of infectious allergic arthritis are almost no different from the symptoms of ordinary arthritis, which is not caused by either an allergy or an infection. This is about:
In all cases, the pain gets worse during movement.
It cannot be ignored that the symptoms of ordinary arthritis are quite severe. Symptoms of infectious allergic arthritis are mild or moderate.
Typically, treatment of bronchitis, tonsillitis or ARVI leaves behind damage to several medium or small vessels. The inflammatory process most often appears in the knee and ankle joints.
The person’s health is generally satisfactory, but the local and general temperature is elevated. Sometimes there may be difficulty breathing. The development of the inflammatory process is indicated by swelling of the joints, which are actively increasing.
In addition, a blood test reveals antistreptococcal or antistaphylococcal antibodies, while the number of leukocytes and ESR are higher than normal.
During the first two weeks of therapy, all symptoms go away. Freedom of joint movement is also completely restored.
X-ray examination shows no pathological changes. An important feature is that the infectious allergic type of polyarthritis, unlike rheumatism, in none of the cases affects the heart.
Unfortunately, this disease is characterized by relapses, which can appear against the background of repeated infections or even due to ordinary hypothermia of the body.
Therapy methods
The therapy takes an integrated approach, where the main principle is the absolute exclusion of further contact with the allergen substance. It is recommended to gently bandage the joints, giving them a physiologically correct location. In general, the therapeutic process is based on the following principles:
- Taking anti-allergy antihistamines like Suprastin, Diazolin, Allercaps, Diphenhydramine, etc.;
- In case of acute arthropathy, analgesic drugs like Baralgin, Spazmolgon and anti-inflammatory drugs are prescribed - Meloxicam, Ibuprofen, Diclofenac, Ketoprofen, etc.;
- The use of chondroprotective drugs that form cartilage tissue and provide a sufficient level of synovial fluid. These medications are especially recommended for the development of recurrent arthropathy;
- If allergic arthropathy is characterized by a severe course, then hormonal medications from the group of corticosteroids and glucocorticoids are additionally prescribed;
- If the provoking agent, in addition to the allergen, is also an infectious agent, then weekly antibiotic therapy with Erythromycin, Amoxicillin or a drug to which the agent is particularly sensitive is indicated;
- Local treatment with ointment or gel preparations - Indomethacin, Rumakar, Fastum-gel, Cinepar, Dolgit, etc.
Arthropathic symptoms are usually easy to relieve, provided that treatment is prescribed in a timely manner and taking into account the characteristics of the pathology. Timely therapeutic measures and accurate execution of all medical prescriptions ensure a positive, lasting result. To avoid developing arthritis in the future, precautions must be taken. If the patient follows preventive recommendations, the prognosis of anti-arthritic therapy will be positive.
Allergic arthritis, the symptoms and treatment of which will be described below, occurs against a background of increased sensitivity of the body to foreign substances and their breakdown products. It can develop against the background of any allergic reaction and become one of the manifestations of serum syndrome - the immune system’s response to the administration of drugs. An allergy to pollen can also result in joint damage. Arthritis also develops against the background of negative reactions of the body to foods and medications:
- antibiotics;
- analgesics;
- vaccines;
- serum.

Contact with chemicals used in the pharmaceutical, textile or oil refining industries can trigger a severe allergic reaction. This is explained by a dysfunction of the immune system, in which it incorrectly reacts to healthy cells, capturing and destroying them. Under the influence of an allergen, the body produces antibodies and immune complexes, which enter the circulatory system and penetrate the synovial cavity. Their accumulation contributes to the development of an inflammatory process called allergic arthritis. The deposition of such substances in tissues is a consequence of congenital defects of the immune system.