Causes of bronchial asthma
Hereditary predisposition plays the greatest role in the development of the disease. If the mother has allergic manifestations, then there is a 60% chance that the child will acquire similar diseases during his life.
There are certain criteria based on which a child is at risk of developing asthma:
- one of the parents has bronchial asthma;
- the child has a confirmed diagnosis of atopic dermatitis;
- there is sensitivity to food and aeroallergens;
- there is an increase in the number of eosinophils in the general blood test of more than 4%;
- existing wheezing in the child, which is not associated with infections.
Preschool children
It is also not always possible to suspect the development of the disease in older children. Signs of asthma in a 2-year-old child may be blurred. For example, their breathing may become faster and more irregular during sleep. This also happens during physical activity.
Characteristic manifestations of the disease also include frequent sneezing, periodic coughing, and restless sleep. Often children do not even notice that they are coughing in their sleep. This happens reflexively. If the child sleeps separately, then the parents may not even hear the cough. Therefore, it is necessary to observe the child, if the kindergarten teacher says that the baby coughs during sleep.
Preschoolers cannot always describe their feelings, so parents must monitor their condition. For example, signs of asthma in a 5-year-old child may appear during active play. You should consult a doctor if your baby begins to cough after a short run. Active movement can cause chest pain and a feeling of squeezing.

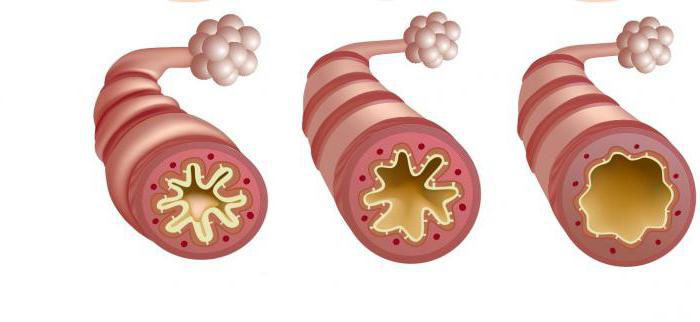
Mechanism of disease development
Chronic inflammation of the bronchi causes the development of bronchial hyperreactivity (reaction of the bronchi in the form of bronchospasm to various types of irritants). The course of the disease is aggravated by the appearance of edema and hypersecretion of mucus in the bronchi.

You can have bronchial hyperreactivity, but not have bronchial asthma.
Features of the course of the disease
It is important to know how asthma can manifest itself before an attack begins. Signs in a child may be: moodiness, irritability, tearfulness, headache, obsessive dry cough.
In most cases, attacks begin in the evening or at night. Initially, there is a cough, noisy breathing, and shortness of breath. Children often get scared, start crying, and rush around in bed. The initial manifestations of asthma in children are often expressed in the form of broncho-obstructive syndrome due to acute respiratory infections. Also, against the background of colds, an attack of asthmatic bronchitis may begin. It is characterized by shortness of breath, which makes it difficult to breathe, and a wet cough.
Atopic bronchial asthma is characterized by the rapid development of an attack. Timely use of bronchospasmolytics allows it to be stopped. But with the infectious-allergic form, attacks develop slowly, symptoms increase gradually. It is not immediately possible to stop an attack by taking bronchospasmolytics.
After the condition normalizes, the sputum begins to cough up, and the shortness of breath goes away. In some cases, the condition improves only after vomiting.
Classification of bronchial asthma
1. By etiology:
- allergic (atopic);
- non-allergic (non-immune).
2. By severity:
- mild: intermittent, persistent;
- moderate;
- heavy.
3. By level of control:
- controlled;
- partially controlled;
- uncontrollable.
4. According to the period of illness:
- exacerbation;
- remission;
5. Based on the presence of complications:
- complicated:
- atelectasis;
- pneumothorax;
- pneumosclerosis;
— subcutaneous/mediastinal emphysema;
- cor pulmonale.
- uncomplicated.
Symptoms of bronchial asthma in children

Common classical symptoms
General symptoms that may indicate the presence of bronchial asthma:
- dyspnea;
- wheezing;
- cough;
- increased symptoms after contact with an allergen, with a change in temperature, or with physical activity.
Basic Concepts
Exacerbation of the disease - a condition in which there is an increase in shortness of breath, cough, wheezing, there is a need to take short-acting bronchodilators, the presence of nighttime symptoms, and possible disturbance of sleep and physical activity.
Asthma control is the disappearance of symptoms of the disease during basic therapy.
Remission is the complete absence of bronchial asthma after discontinuation of medications, as well as the preservation of normal external respiratory function in a child.
Symptoms reflecting the severity of bronchial asthma
Clinical symptoms vary depending on the severity:
- mild: symptoms of difficulty breathing appear less than once a week. Attacks of bronchial asthma are episodic in nature and, as a rule, resolve spontaneously or after taking a short-acting bronchodilator. There are no nighttime symptoms, sleep is not disturbed. The child tolerates physical activity calmly. Spirometry reveals FEV1 (forced expiratory volume in 1 second) and PEF (peak expiratory flow) levels of more than 80%. Daily fluctuations in bronchial patency are no more than 20%. During the period of remission there are no symptoms. The external respiration function does not change and remains normal;
- moderate: shortness of breath appears more than once a week. Attacks of moderate severity require constant daily medication (basic therapy). Nighttime symptoms appear regularly. The child develops limited tolerance for physical activity. Spirometry indicators (FEV1 and PEF) are 60 - 80%. Daily fluctuations in bronchial patency are 20 - 30%. Incomplete clinical and functional remission is observed;
- severe: symptoms of difficulty breathing bother the patient several times a week or daily. Frequent severe and regular nighttime asthma symptoms in children require basic therapy. The child's sleep is disturbed, and the tolerance to physical activity is significantly reduced. FEV1 and PEF decrease sharply and are less than 60% of predicted. There is an increase in daily fluctuations in bronchial patency - more than 30%. The child develops respiratory failure of varying severity; complete remission cannot be achieved.
In addition to the above symptoms, there may be an increase in the number of respiratory movements and heart rate, the participation of auxiliary muscles in the act of breathing, and during a severe attack the patient’s speech is difficult. The more severe the exacerbation, the more pronounced the changes in the body: a drop in oxygen saturation, an increase in the partial pressure of carbon dioxide, a decrease in oxygen.
Symptoms by level of control
You can also divide the symptoms of the disease according to the level of control over bronchial asthma:
- controlled: with this type there will be an absence of daytime and nighttime symptoms, limitation of mobility, need for emergency medications (or less than 2 times a week), and exacerbations. FEV1 and PEF values remain normal;
- Partially controlled asthma is diagnosed when any of the manifestations are observed during the week: daytime symptoms more than 2 times a week, there is a limitation in activity, sleep disturbance, there is a need for emergency medications (more than 2 times a week), spirometry readings are more than 80% , exacerbations develop 1 time or more per year;
- uncontrolled bronchial asthma is diagnosed in the presence of 3 or more signs of partially controlled asthma. Exacerbations occur within a week.
When examining the patient, attention will be drawn to the “bloated” shape of the chest, shortness of breath, wheezing that can be heard from a distance, as well as a forced posture (the patient sits with his hands on his knees).
Allergic asthma attack
An attack of allergic asthma should be understood as a reaction on the part of the human immune system in which bronchospasm appears in response to exposure to an allergen. It is this that constitutes an attack as such, accompanied by a contraction of the muscle tissue surrounding the respiratory tract. As a result of this pathological condition, the muscles become inflamed and filled with viscous, thick mucus. At the same time, the supply of oxygen to the lungs is sharply limited.
To eliminate an attack of atopic allergy, a whole range of measures is required. First of all, they are aimed at relieving the symptoms of the disease. A calm and relaxed state during an attack is a necessary component; if a person begins to worry and worry, then his situation only gets worse. Slow inhalations and exhalations, a flow of fresh air (not cold), and a horizontal body position will help cope with an attack of atopic asthma in a matter of minutes.
Ideally, you should have a medication inhaler. Its use will quickly relieve a suffocating attack and restore the functioning of the smooth muscles of the respiratory organs.
Asthmatic status. Extremely dangerous for human life is this form of manifestation of atopic asthma, in which an asthmatic condition called status asthmaticus develops. It is a long-term suffocation that cannot be treated with traditional medications, in which a person is simply unable to exhale air. This state develops from some clouding of consciousness to its complete loss. At the same time, the person’s general well-being is extremely difficult. Lack of necessary treatment can lead to disability and even death.
Diagnosis of bronchial asthma
To confirm the diagnosis, it is necessary to perform a number of examinations:

- Complete blood count (allows you to detect an increase in the number of eosinophils in the peripheral blood).
- Skin tests to determine the allergen that causes allergic reactions.
- Determination of general and specific immunoglobulin E.
- Consultation with an allergist (for allergen-specific immunotherapy), a pulmonologist.
- Spirometry (a method for assessing external respiration).
Spirometry is not informative to use in children under 5 years of age!
The method is used for older children; it allows one to assess the degree of airway obstruction, the severity of bronchial asthma, as well as the child’s condition at the time of examination. Spirography includes the determination of several indicators:
- FEV1 (forced expiratory volume in 1 second) is normally more than 80%;
- FVC (forced vital capacity of the lungs, allows you to evaluate the patency of the bronchial tree) - the norm is from 70% to 80%;
- the FEV1/FVC ratio (Tiffno index, expressed as a percentage) determines the presence or absence of normal bronchial patency, the norm is more than 70 - 75%;
- reversibility of bronchial obstruction - an increase in the volume of forced expiration (normally more than 12%) after the use of drugs.
- Peak flowmetry (determination of peak expiratory flow). This method should be used regularly, daily to monitor the treatment of bronchial asthma. In children, special nomograms are used. The child should measure peak expiratory flow in the morning before taking medications (usually the value is lower) and in the evening (it becomes higher), after which all changes should be recorded. The higher the peak expiratory flow rate (more than 30%), the more severe the disease.
- Detection of airway hyperresponsiveness. This method is provocative in nature, its use is advisable in the presence of symptoms characteristic of bronchial asthma, but in the absence of respiratory dysfunction. The provocation consists of using physical methods (running for 6 minutes), chemical ones (methacholine), the latter is rarely used in children, mainly in adolescents, as it has a number of contraindications and side effects. After using the irritants, observe the reaction of the bronchi.
- X-ray examination of the chest organs and paranasal sinuses according to indications to exclude controversial issues when making a diagnosis.
- ECG and echocardiography are used because the disease affects the cardiovascular system in addition to the respiratory system.
- Sputum examination for differential diagnosis.
- Bronchoscopy is prescribed for special indications (for example, foreign body aspiration).
Unusual signs of asthma
In addition to the main symptoms, bronchial asthma can also manifest itself with other symptoms. The most common form of the disease is cough asthma, but asthma without cough and without shortness of breath is also possible.
Unusual symptoms of bronchial asthma include:
- intermittent “uneven” breathing;
- noises during sighs - “sighing”;
- apathy, lack of physical activity;
- increased excitability, inability to concentrate on anything;
- sleep disturbance.
Such symptoms more often appear in children and adolescents, therefore, in case of any breathing problems, the appearance of unclear signs or any of the symptoms described above, you must immediately consult a doctor for timely diagnosis and treatment.
source
Treatment of bronchial asthma in children

The main goal of treating bronchial asthma is to achieve complete control over it.
Basic principles of therapy
Elimination measures
Reduction or complete elimination of the causative allergen (hypoallergenic diet and lifestyle, possible change of territory in which the patient lives).
Mode
Treatment of bronchial asthma is carried out regularly, depending on the severity, at home. But there are some situations that require additional round-the-clock monitoring by medical workers. Indications for hospitalization:
- severe exacerbation;
- lack of quick response and effectiveness from the used bronchodilators;
- no improvement from taking hormonal drugs (within 2 - 6 hours);
- social disadvantage;
- life-threatening conditions associated with exacerbation of bronchial asthma or their presence in the child’s medical history.
Drug therapy

Treatment of bronchial asthma, that is, for each course of the disease, a certain treatment tactic is carried out. If it is impossible to achieve control over asthma or there is a severe course, then the doses of drugs are increased, depending on their effectiveness in the future. If it is possible to establish control and the symptoms do not bother the child for 3 months, then the doses of drugs are reduced and the body’s reaction is monitored with lower doses of drugs.
Pharmacotherapy of bronchial asthma is divided into 2 groups:
- basic (supportive, anti-inflammatory) therapy, which is aimed at preventing the development of exacerbations;
- symptomatic therapy allows you to stop attacks of the disease; these drugs are also called “first aid”.
There are several types of drug delivery to the child’s respiratory tract:
- metered dose aerosol inhaler (used in children over 5 years of age);
- breath-activated metered-dose aerosol inhaler (for children over 5 years of age);
- powder inhaler (over 5 years);
- spacer (for children over 4 years old, when using a face mask can be used in children under 4 years old);
- nebulizer (can be used for children from 0 years old).
Basic therapy
Inhaled glucocorticosteroid drugs and combination drugs
This group of drugs is the most effective method of combating exacerbations of bronchial asthma, that is, they are basic therapy. In children, drugs such as Beclomethasone, Budesonide, and Fluticasone are used. Dosages are developed for each age, as well as taking into account the severity of the disease. Depending on the effectiveness, dosages can be correlated, but the best alternative to large doses are combination drugs - Seretide (Salmeterol + Fluticasone), Symbicort (Formoterol + Budesonide). Studies have shown that combination drugs improve external respiration, help achieve remission, and also significantly improve the patient’s quality of life.
Leukotriene receptor antagonists
More often, drugs in this group are prescribed in addition to inhaled glucocorticosteroids, when low doses of the latter drugs are not effective enough. Leukotriene receptor antagonists can act as monotherapy for mild forms of bronchial asthma. Drugs in this group include: Montelukast, Zafirlukast.
Cromony
To date, cromones have the weakest anti-inflammatory effect. They should not be combined with other drugs, and they are also contraindicated in case of exacerbation of bronchial asthma.
Anti-IgE drugs
A relatively new class of drugs that is used in the treatment of severe bronchial asthma. The only drug studied is Omalizumab (Xolair), which is being used not only in Russia, but also in other countries of the world. The disadvantage is the high cost of the drug, as well as the subcutaneous route of administration.
Long acting theophyllines
This group of drugs is rarely used, and in some countries they are generally contraindicated for use in children due to severe complications (cardiac arrhythmia, death).
Long-acting β2-agonists
The group's drugs are divided into fast-acting (Formoterol) and slow-acting drugs (Salmeterol). These drugs are used together with inhaled glucocorticosteroids when the doses of the latter do not allow achieving adequate control of bronchial asthma.
Monotherapy with long-acting β2-adrenergic agonists without inhaled glucocorticosteroids is impossible, as it increases the likelihood of the patient’s death!
Emergency treatments
Inhaled short-acting β2-agonists
This group allows you to eliminate bronchospasm in the shortest possible time. The main representative of the group is Salbutamol.
Salbutamol is the “gold standard” for relieving bronchospasm!
Also included in the group is Fenoterol. It is possible to use a combination drug: Fenoterol + Ipratropium bromide.
Anticholinergic drugs (Ipratropium bromide) and short-acting theophyllines (Eufillin) have a limited role in the treatment of bronchial asthma in children.
There are several clinical stages of the disease
Depending on the stage of the disease, characteristic signs can vary significantly. Also, the symptoms of bronchial asthma in adults, children and adolescents have their own characteristics.
1. The risk of developing bronchial asthma in healthy people - at this stage there are no signs of the disease yet; there are certain disorders in the human body - in the endocrine, nervous or immune system, but these changes can only be identified as a result of a thorough examination. Such conditions make the human body more susceptible to various diseases, including bronchial asthma. It is especially important to pay attention to the growing body of children and adolescents; most often, the disease begins during a period of rapid growth and development of the body - in the first years of life or during puberty in adolescents.
2. Preasthma is a condition in which the first clinical symptoms of the disease appear; under unfavorable conditions, they can lead to the onset of the disease. Signs of pre-asthma include frequent colds, other allergic manifestations - vasomotor rhinitis, urticaria, conjunctivitis, obsessive cough, shortness of breath. Gradually, other signs of the disease may appear, but, at this stage, there are no attacks of suffocation.
Dispensary observation

A child diagnosed with bronchial asthma is assigned health group III - IV. The patient is observed until transfer to an adult clinic. The local pediatrician and allergist examine children with a frequency corresponding to the severity of the pathology. With a long interictal period, observation 2 times a year is possible. And if the child has a severe course of the disease, an examination is necessary once a month. An otorhinolaryngologist and dentist observe the patient 2 times a year to eliminate chronic foci of infection. General blood and urine tests are taken once every 3 months. Spirography is carried out 2 times a year. Other examinations are prescribed to the patient according to indications, in accordance with the existing concomitant pathology.
Children with mild and moderate forms of the disease can attend school and engage in physical education in the preparatory group, with the exception of release for 1 month after each attack. If a child is diagnosed with severe bronchial asthma, then such children are taught at home, and exams are carried out using a gentle method. Disability is established for 2 years.
Immunization of patients is carried out during the period of remission against the background of basic therapy.
Prevention
Prevention of bronchial asthma is a set of measures aimed at developing the disease and preventing exacerbations of the disease. There are primary, secondary, tertiary.
Primary prevention is aimed at people at risk of developing the disease (children with a family history). Recommendations for children: maintaining exclusive breastfeeding until the first 4 - 6 months of life. It is also necessary to exclude the impact of harmful vapors (tobacco smoke) on the child’s body.
Secondary prevention is aimed at children with existing allergic manifestations. For allergic diseases (allergic rhinitis, atopic dermatitis), compliance with all treatment principles is mandatory.
Tertiary prevention is carried out for children with an established diagnosis - a set of measures aimed at reducing the number of exacerbations, maintaining control over the disease, and improving the patient’s quality of life. Activities include: exclusion of allergens from food, establishment of a hypoallergenic lifestyle, regular examination by an ENT specialist and dentist, treatment of concomitant pathologies and adherence to all principles of basic therapy.











