Description
This is a group of allergic pathologies caused by the formation of hypersensitivity to aerosol allergens and accompanied by acute inflammation of the skin and mucous membranes. The clinical picture includes sneezing, runny nose, odor disturbance, itching, redness and swelling of the tissues of the nasal cavity and conjunctiva. The diagnosis of hay fever requires consultation with an allergist-immunologist, skin tests, general clinical examinations and special laboratory examinations. Treatment includes eliminating contact with the allergen, taking antihistamines, and conducting specific allergen immunotherapy.
Allergic rhinitis according to ICD 10
Allergic rhinitis is an inflammation of the nasal mucosa.
It is accompanied by a profuse flow of mucous masses from the nasal passages, bouts of sneezing, swelling and a feeling of nasal congestion. Despite the presence of unpleasant symptoms that bring significant discomfort and interfere with the quality of life, many patients do not consider this illness to be a disease, so they are in no hurry to see a doctor, but engage mainly in self-medication: watching advertisements on television, buying “magic” drops and uncontrollably accepted. Friends! This is completely wrong!
Hay fever is an independent disease, as confirmed by the international classification of diseases (ICD 10). In our country, the proportion of people susceptible to allergic rhinitis reaches almost forty percent.
The ICD is a list of all known diseases. Each diagnosis is assigned a unique alphanumeric code. For the average person, these codes do not carry any meaning.
However, this classification is used in healthcare in every country in the world and clearly structures absolutely all diagnoses that exist today. It is reviewed and updated every ten years. Judging by the number 10 in the title, it is not difficult to guess that the ICD has already been revised ten times.
Allergic rhinitis is classified under the category “Other upper respiratory tract diseases”. The ICD 10 code value for this disease is J30.
In turn, hay fever is divided into narrower varieties of the disease, each of which has its own code. Below is an excerpt from this document - opposite each diagnosis is its ICD 10 code:
- J30.0 - vasomotor rhinitis;
- J30.1 - allergic rhinitis provoked by pollen of flowering plants;
- J30.2 - other seasonal allergic rhinitis;
- J30.3 - other allergic rhinitis;
- J30.4 – hay fever of unknown origin (that is, after all the research results, the cause of the disease could not be found).
Types of disease
Hay fever has several varieties, differing in different periods of occurrence. There are year-round, seasonal, episodic and occupational hay fever.
A year-round runny nose is considered chronic. It bothers the patient no more than a couple of hours a day, but this condition lasts about nine months a year. As a rule, it is caused by household allergens. It does not bring any noticeable discomfort or decreased performance.
Seasonal runny nose appears during the period of active flowering of plants, lasts from several days, but the emerging symptoms bring discomfort to the patient and interfere with full-fledged life activities.
Episodic occurs only upon contact with an allergen, for example, animal fur or saliva. At the same time, the symptoms of the disease are very pronounced.
Occupational rhinitis is a relatively new subtype of the disease. It is caused by constant contact of a person with a certain allergen due to his profession (for example, confectioners, pharmacists, workers in woodworking enterprises).
Causes of the disease
Of course, the primary cause of the disease is contact with an allergen. But not everyone gets sick!? The following reasons contribute to the development of hay fever:
- lack of sleep, chronic fatigue;
- contaminated air;
- heredity;
- stress;
- anatomical features of the structure of the nasal cavity and nasopharynx;
- prolonged contact with the allergen;
- problems with blood clotting;
- frequent colds;
- diseases of the gastrointestinal tract;
- taking antibiotics.
Diagnosis and treatment
To make a correct diagnosis, you need to consult an ENT doctor. He will conduct a rhinoscopy (examination of the nasal cavity), prescribe the necessary tests (general blood count, blood test for the presence of antibodies, tests for allergens, etc.).
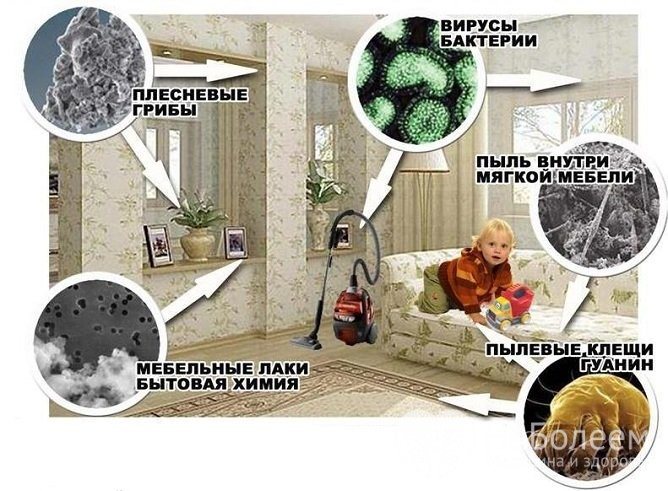
Treatment for rhinitis should begin with eliminating exposure to the allergen. If you are allergic, there should be no animals, dust, soft toys or carpets in the house.
There should be a humidifier and an air washer in the room where you sleep, then the air will become much cleaner and more humidified.
We also recommend purchasing a good vacuum cleaner with powerful suction, antibacterial filters and filtration of dust and dirty air through water! After using this vacuum cleaner at least once, you will see in the dirty water what you breathe!
If you are allergic to flowers, you should avoid trips outside the city to nature or stay away from parks or flower beds.
To relieve an exacerbation, antihistamines (Suprastin, Tavegil, etc.), vasoconstrictors (Otrivin, Xylometazoline), saline solutions (Aquamaris), antiallergic drops (Vibrocil) are prescribed. It is better not to purchase corticosteroid (hormonal) nasal sprays yourself!
One way or another, treatment should be prescribed and carried out exclusively under the supervision of an otolaryngologist. Only an experienced, competent ENT doctor will prescribe effective drug therapy and relieve the disease.
Please make an appointment and come!
We will help you cope with the manifestations of allergic rhinitis!
We will be glad to see you in our clinic and will be happy to help you!
Source: https://zen.yandex.ru/media/id/5ab4a825fd96b102b0c8c3e2/allergicheskii-rinit-po-mkb-10-5c7f4f1cc0c8ed00b49b721e
Additional facts
Hay fever in children (hay fever, pollen allergy) is a seasonal allergic disease associated with inflammation of the mucous membranes and skin. The clinical picture mainly includes rhinitis, dermatitis, and conjunctivitis. Without proper therapy, the pathology progresses and turns into bronchial asthma with subsequent complications. It is found in 3.7% of the pediatric population, and the number of patients is increasing every year. Most often, such an allergic reaction is recorded in countries and regions with a large number of flowering plants and a dry climate. The initial detection of hay fever is observed at the age of 5-9 years; in children under 3 years of age, pollen allergies are extremely rare.
Hay fever in children
Hay fever - what is it?
Hay fever disease: ICD 10 code – J30.1. Also called:
- allergic rhinitis;
- allergies caused by plant pollen;
- hay fever;
- seasonal allergies.
Hay fever (hay fever) is the name given to an immediate allergic reaction that manifests itself within a few minutes after pollen contacts the mucous membranes of the nose, eyes or respiratory tract. At the same time, many people with pollen allergies run the risk of being hypersensitive to the flowering of several plants at the same time.
The fundamental factor due to which allergic hay fever develops is considered to be disturbances in the functioning of the immune system.
Seasonal hay fever is divided into 3 types, depending on the period of pollination of all kinds of plants. There are spring, summer and autumn hay fever.
Allergy hay fever can occur at different times of the year, and in some cases, occur almost all year round, depending on the flowering time of individual plants.
As a rule, in the spring, from March to May, the first wave of allergies is caused by pollen from trees: birch, ash, elm, hazel, maple, spruce, alder, willow, oak, lilac, pine. And also flowers: coltsfoot, dandelion, etc.
In the summer, from June to August, allergens from nettle, hazel, poplar, sunflower, apple tree, etc. cause illness.
In the summer-autumn period from July to October, pollen allergens of weeds and cereal grasses are activated: wormwood, ragweed, wheatgrass, etc.
Please note that the flowering calendar for plants may vary depending on the area in which you live. In the southern regions, flowering begins much earlier than in the rest.
Causes
The main cause of hay fever is plant pollen, which has pronounced allergenic activity and is common in certain regions of the world. Of the thousands of species of flowering plants, about fifty are considered allergens. The etiological factor is grasses, trees and weeds that grow and grow in the wild. To cause hay fever, the pollen must come from plants that are widely present in the area, pollinated by wind and, in rare cases, insects. It must be light and small in size (no more than 35 microns) and transported over long distances. Pollen concentration is influenced by many factors, with the highest values recorded during the day in dry and windy weather.
Causes of allergic rhinitis in children
The appearance of the disease in a baby may be associated with a hereditary predisposition to allergic diseases. The family history often includes bronchial asthma, allergic urticaria, diffuse neurodermatitis and other atopic pathologies diagnosed in one or more family members.

The most common cause of hay fever is grass and plant pollen.
Most often, hay fever develops due to pollen from trees and grasses of the Asteraceae, Chenoceae or Poaceae family. It can also be caused by fungal spores. The appearance of poplar fluff coincides with the flowering of plants whose pollen provokes rhinitis. Pooh actively collects pollen and carries it to places where it would not otherwise reach.
The seasonality of the annual development of pronounced clinical manifestations of allergic rhinitis after its asymptomatic or erased course depends on the climatic characteristics of the region in which the child lives and practically does not change from year to year.

Allergies can develop as a result of contact with mold
The year-round form occurs in children who are in frequent contact with allergens located at home or in their environment. These include: hair and particles of the epidermis of pets, various chemical compounds, mold, household dust containing micromites. Symptoms occur throughout the year and may worsen regardless of the season.
Pathogenesis
The antigen enters the body mainly through the upper respiratory tract, after which activation of the immune system begins. The first organ where inflammation develops is the nasopharynx. Here the pollen interacts with macrophages, trying to absorb and neutralize it. A little later, T and B lymphocytes and eosinophils are activated, interleukins are produced and specific IgE antibodies are synthesized. The latter protein structures are fixed in mast cells and basophils of target organs: skin, mucous membranes of the respiratory system, conjunctiva. An allergic reaction develops upon repeated contact with the antigen. As a rule, the process of re-penetration of the allergen, its fixation in tissues and the development of inflammation takes from 5 to 10 minutes if the pollen concentration at the time of contact is high. An antigen-antibody complex is formed, mast cells are activated and secrete inflammatory mediators, among which histamine plays a major role.
Classification
There is no official classification of hay fever recognized by an academic council. In clinical practice, the disease is usually divided depending on the severity of the pathology and the area of inflammation. The course and severity of symptoms of the disease are mild, moderate and severe. The location distinguishes: • Allergic eye diseases.
An inflammatory reaction accompanied by redness and swelling of the conjunctiva (allergic conjunctivitis), eyelid margins (allergic blepharitis), and cornea (allergic keratitis).
• Respiratory allergies.
Includes damage to parts of the respiratory system - rhinosinusitis, adenoiditis, laryngitis, otitis media.
• Allergic dermatoses.
They indicate skin changes, the formation of atopic dermatitis and urticaria.
• Combined pathologies.
They are common, consisting of two or more types of hay fever.
Symptoms
The clinical picture of hay fever depends on the area where pollen settles and the degree of activation of the body's immune forces. Thus, when the nasal mucosa is inflamed, the child experiences severe itching and a tickling sensation. There are paroxysmal sneezing, which are combined with mucous discharge from the nose. At the same time, the tissues are hyperemic and swollen, causing difficulty breathing. As hay fever progresses in children, the inflammatory process spreads to the sinuses, auditory tubes and larynx. When the eyes become inflamed, redness of the conjunctiva and dry tissue are observed, which leads to rupture. The child complains of a feeling of “sand” in the eyes, roughness, and inability to look at bright light. In some cases, a secondary infection occurs, the symptoms are supplemented by pain, purulent discharge from the conjunctival cavity, and, extremely rarely, an increase in body temperature. Cardiovascular changes caused by hay fever cannot be excluded; they are characterized by an increase in heart rate, changes in blood pressure and muffled heart sounds. These disorders are temporary and do not require additional therapy when the underlying disease ceases to resolve on its own. Nervous system changes may occur, including recurrent burning headaches, sleep disturbances, weakness and dizziness. These symptoms are a consequence of a lack of oxygen due to swelling of the nasal mucosa. Hay catastrophe may be accompanied by signs of digestive tract distress if pollen enters the digestive tract through food. In this case, the clinical picture is complemented by nausea and diarrhea. Impaired sense of smell. Diarrhea (diarrhea). Loss of smell. Nausea.
Treatment of allergic rhinitis in children
After confirming the diagnosis, the allergist determines how and how to treat allergic rhinitis, taking into account the medical history, age and general health of the child. Preventive measures aimed at reducing the patient’s contact with allergy pathogens are of primary importance. In order to determine what type of allergens cause inflammation, allergy tests are necessary.
In case of allergic rhinitis, it is necessary to pay sufficient attention to the prevention of the disease
The most difficult thing is to avoid contact with natural sources of the disease. During the flowering period of plants, it is important to limit the child from direct exposure to them: avoid walking on windy days, after a thunderstorm, in places where there is freshly cut grass, use sunglasses, and close the windows when traveling in a car. Dr. Komarovsky recommends daily wet cleaning in a house where there is an allergy sufferer.
With allergic rhinitis, the nasal mucosa becomes pale and loose. In some cases, redness of the conjunctiva and slight or moderate hyperemia are noted.
Along with preventive measures, the most effective both for blocking the allergic response and reducing inflammation, and for improving the child’s quality of life, is drug therapy. Self-medication or the use of folk remedies without prior consultation with a specialist can lead to a worsening of the condition.
Antihistamines
Antihistamines are most often prescribed to patients with allergic rhinitis. Their action is to competitively block histamine receptors in the body, thereby inhibiting the effects mediated by it. Histamine is a neurotransmitter that affects the airways - causing bronchospasm and swelling of the nasal mucosa. Allergic reactions enhance its effect, so antihistamines from the group of H1-blockers are used to eliminate them. These include Fexofenadine, Loratadine, Cetirizine, Hydroxyzine and Diphenhydramine.

Loratadine is one of the commonly used antihistamines.
Taking antihistamines relieves itching, eliminates runny nose, coughing and sneezing. According to reviews, the most common side effect of these medications is drowsiness, which requires adjustment of the dosage regimen. For young children, antihistamines are prescribed in the form of syrup, for older children - in tablets. It is possible to use products in the form of nasal sprays and eye drops.
Glucocorticosteroids for local use
In addition to topical antihistamines, steroid sprays or drops are prescribed to children with hay fever to control nasal inflammation and relieve eye symptoms. Their therapeutic effect manifests itself after a few days, so the use of such drugs should begin some time before the flowering season.

When using local glucocorticosteroids, nosebleeds may develop
Sometimes when spraying the product, nosebleeds are observed. Its development is not related to the method of application of the spray, but is the result of an inflammatory process. Only in cases of heavy or prolonged bleeding is it necessary to consult a doctor to select a different dosage form of glucocorticosteroids.
For mild allergic rhinitis, Montelukast may be the drug of choice. It helps improve the quality of life in children with signs of rhinoconjunctivitis.
When eye complications occur against the background of allergic rhinitis, the use of eye drops is most effective. Like nasal sprays, it is best to start using them some time before the flowering season. Many drops contain cromoglycate, the effect of which is to block cells that secrete histamine.
Drops are used conjunctivally - instilled into the lower conjunctival sac of the eye. It is better for younger children to carry out the procedure in a lying position, holding their head, for older children - in a sitting position with their head tilted back.
Local glucocorticosteroids prescribed to children include:
- Flixonase – dosed nasal spray, used from 4 years;
- Sofradex is a glucocorticosteroid in combination with an antibiotic in the form of eye drops. Used in older children;
- Nasonex is a dosed nasal spray, prescribed to children from 2 years of age.
Antileukotrienes
Allergic rhinitis is often a concomitant disease of bronchial asthma and, when isolated, increases the risk of its development. Antileukotrienes are used to control the symptoms of asthma, promote narrowing of the lungs and reduce the likelihood of fluid accumulation in them. Clinical studies of such drugs have shown their effectiveness in monotherapy of hay fever, comparable to that when using new generation antihistamines.
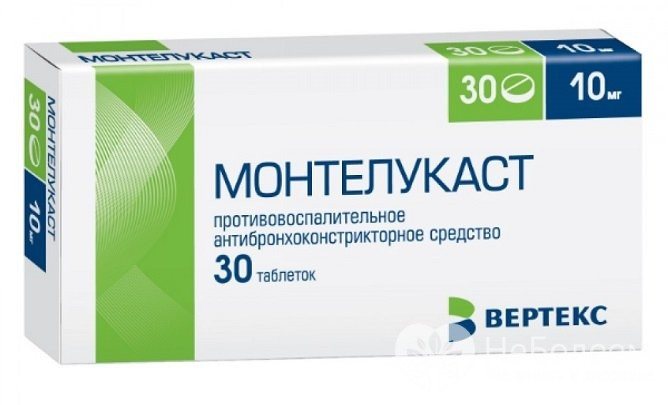
Children may be prescribed Montelukast as part of complex treatment.
For mild allergic rhinitis, Montelukast may be the drug of choice. It helps improve the quality of life in children with signs of rhinoconjunctivitis. Its use is also justified in cases of bronchial asthma accompanied by allergic rhinitis.
The drug is available in two forms - film-coated tablets and chewable tablets. Montelukast can be used in children over the age of 6 years, following the clinical recommendations of the doctor.
Immunotherapy
To improve the effect of medications prescribed for the treatment of allergic rhinitis and to strengthen the child’s body during the period when symptoms of the disease appear, immunotherapy is used. Its action is aimed at changing the immune system so that it does not react to allergens as a threat. The most common method is subcutaneous injections with an allergen. They allow you to gradually reduce the body's sensitivity to their effects and, over time, reduce the manifestation of symptoms of the disease.
Immunotherapy is effective for allergies to mold, animal dander, dust mites and cockroaches, pollen from trees, grasses, and ragweed. This type of treatment is carried out under the supervision of a doctor and only in adolescents.
Possible complications
The most severe and common complications of hay fever in children are stenosing laryngotracheitis, allergic bronchitis and bronchial asthma - they occur in 22.8-48.4% of children suffering from hay fever. All these diseases are accompanied by impaired airway patency and, accordingly, tissue hypoxia. The extreme degree of bronchial asthma—status asthmaticus—is an indication for hospitalization of a child in the intensive care unit. The most common result of treatment for pollen allergy is angioedema and recurrent urticaria.
Diagnostics
The examination consists of two main stages: the first is a preliminary diagnosis, the second is the identification of a causally significant allergen. The child was examined by a pediatrician, pediatric ophthalmologist, dermatologist and otolaryngologist. All examinations are carried out under the supervision of a pediatric allergist-immunologist. The time frame for performing manipulations and obtaining results varies within 3-14 days. • Consultative appointment.
During the consultation, signs of allergies and the duration of symptoms are indicated.
You can suspect hay fever in a child if there is a positive allergic history (pathology in one of the closest relatives), symptoms of the disease develop during the flowering of plants and disappear in winter or late autumn. • Allergy tests.
Blood sampling is included to study specific IgE antibodies and allergen panels, perform general analysis and eosinophil counts. The most informative are the skin allergens with the most common causative allergens. To diagnose hay fever in children, pollen from trees, cereals, weeds, flowers and cultivated plants is used. Based on the results of the examination, differential diagnosis of hay fever is carried out in acute respiratory viral infections, bacterial conjunctivitis, chronic rhinitis and other types of allergic reactions. The result is an objectively diagnosed and correctly selected therapy, taking into account the severity of the disease and the age of the child.
Treatment
To reduce the severity of symptoms, contact with the flowering plant should be avoided. In modern pediatrics and allergology, a three-stage treatment of hay fever is recommended: acute therapy, anti-relapse treatment, allergen-specific immunotherapy: At the first stage, antihistamines are prescribed that block H2-histamine receptors and prevent the further development of inflammation. New generation systemic drugs are preferable; they have a less sedative effect. You can also use sympathomimetics (to reduce tissue swelling); endocasic glucocorticosteroids (to quickly eliminate the symptoms of pollen allergy with severe symptoms of the disease); beta-2 agonists (to reduce the progression of bronchial asthma in the early stages). • Supportive care.
An antihistamine drug with a pronounced antiallergic effect was selected, and the timing of admission was established to coincide with the flowering period of plants whose pollen causes pathology in the child. Some experts recommend periodically switching medications to a different group of antihistamines of the same generation for more effective therapy. The most effective method of combating hay fever is allergen-specific immunotherapy. It involves the oral or injectable administration of small doses of an allergen to gradually reduce the body's sensitivity to a specific antigen. This treatment of hay fever is carried out exclusively under the supervision of a pediatric allergist in compliance with all the rules for taking the drug and increasing its dosage. ASIT begins when the child turns 5 years old.
Hay fever. What it is? Features of hay fever, its treatment, symptoms and signs
Hay fever is a classic allergic disease that occurs in people of any age and gender. The high level of prevalence of hay fever is associated with deteriorating environmental conditions on the planet. In adults, the disease occurs between the ages of 18 and 40, and is more common than in children; more women are affected.
Hay fever, definition
Hay fever is an allergic disease, the clinical symptoms of which - rhinitis and conjunctivitis - appear only during certain plant flowering seasons.
When pollen penetrates the body, the process of producing specific antibodies is activated, which, together with antigens, create immune complexes.
These complexes, attaching to receptors on the cytoplasmic membrane of tissue basophils (mast cells), destabilize them, which causes the activation and release of histamine, serotonin and other inflammatory mediators from the cells.
Mediators enhance the secretion of exudate, increase the porosity of capillaries, and cause contraction of smooth muscle fibers of the bronchi, which is clinically manifested by: lacrimation, sneezing, secretion of watery nasal discharge, bronchospasm.
Symptoms of hay fever
Symptoms of hay fever are strictly seasonal. The severity of the course and severity of symptoms of hay fever are directly determined by the intensity of plant flowering and weather conditions.
In dry weather with wind, the saturation of air with pollen increases, and the symptoms of the disease also increase. When it is humid, the density of pollen particles in the air is minimal, and the patient’s condition improves.
Characteristic clinical symptoms are caused by synchronous damage to the mucous membranes of the nasal cavity and organs of vision. Eye symptoms:
- Feeling of “sand”, the presence of foreign particles in the eyes.
- Itching, burning in the area of the eyeballs.
- Constant lacrimation.
- Photophobia.
- Periorbital edema.
- Hyperemia of the conjunctival membrane.
- Dilated capillaries of the sclera.
- Narrowing of the palpebral fissure.
- Swelling of the eyelids.
Respiratory tract symptoms:
- Severe itching in the nasopharynx.
- Impaired nasal breathing.
- Paroxysmal sneezing.
Nasal discharge is copious and mucous.
If allergic inflammation affects the paranasal sinuses, sinusitis is formed.
Sometimes contact allergic dermatitis, urticaria, pathologies of the genitourinary tract (cystitis, vulvovaginitis), nervous system (arachnoencephalitis) are added. With a high degree of sensitization of the body, the development of pollen intoxication is possible, which is clinically manifested by weakness, fatigue, increased sweating, tachycardia. fever, headaches, insomnia or daytime sleepiness.
The most dangerous manifestation of hay fever is bronchospastic syndrome (pollen bronchial asthma) in the form of a dry paroxysmal cough, with episodes of suffocation and shortness of breath. Bronchial asthma as the only clinical manifestation of hay fever occurs in 11% of cases. In winter, no exacerbations are observed. With the end of the dusting season, the signs of rhino-conjunctivitis gradually end.
Causes of hay fever
The cause of hay fever is an immediate allergic reaction as a response of the immune system to the penetration of pollen from flowering plants into the body, which was previously sensitized with a certain antigen.
Research in the field of molecular allergology has shown that the source of allergic reactions in hay fever is not only pollen, but also other parts of plants (leaves, seeds, fruits, stems).
This serves as the basis for the occurrence of cross food allergies and intolerance to plant-based medications in patients.
Factors provoking hay fever
Hereditary predisposition: a person’s allergies manifest themselves in 50% of cases if both parents have symptoms of any allergic pathologies; if one is sick - 25%.
- Antenatal pathologies: prematurity, low birth weight babies.
- Lack of breastfeeding.
- Place of residence: urban residents suffer from hay fever 4–6 times more often than rural residents.
- Time of birth – children born during the dusting season have a greater risk of developing hay fever.
- Frequent ARVI.
- Smoking.
- Poor nutrition, presence of allergens in food.
- Geographical factors - the existence in the region of plants that spray allergic pollen.
- Atmospheric air pollution from industrial waste and vehicle exhaust gases.
Diagnosis of hay fever
Diagnosis of hay fever takes place in 2 stages.
- The first stage of the examination is performed by a general practitioner or family doctor
- A detailed study of the disease history (seasonal manifestations of the disease in spring and summer).
- Identification of family heredity for various types of allergic pathologies.
- Conducting a physical examination (rhinoscopy and ophthalmoscopy, x-ray of the sinuses).
- Laboratory tests of blood, nasal secretions, and sputum, in which, in case of hay fever, a large number of eosinophils are detected.
The second stage of the examination is carried out by an allergist.
- Skin tests with pollen allergens are performed outside the exacerbation season. The method consists of intradermal injection of suspected purified allergens. The result is assessed after 20 minutes - if hyperemia or swelling of the skin occurs at the injection site, the test is considered positive.
- Provocative biotests are used when skin tests are insufficiently clear. When performing the study, allergic reactions of varying severity occur, so they are performed exclusively in specialized hospitals, where doctors are familiar with emergency care techniques for the development of conditions that are dangerous to the health and life of the patient (Quincke's edema, anaphylactic shock), and also so that the patient is under 24-hour medical supervision. A diagnostic sample (a component of pollen) is administered into the nose, into the eyes, or in the form of inhalation. The appearance of an allergic reaction to a certain type of pollen is evidence of a precisely identified etiological antigen that provokes hay fever. Determination of specific reagins in the blood - Ig E
Hay fever code (ICD-10)
The code for hay fever according to the International Classification of Diseases, 10th revision is J30.1. Hay fever is included in class X - “Diseases of the respiratory system”, and is defined as “Allergic rhinitis caused by pollen”
Seasonal hay fever
Hay fever is called seasonal allergy, since the disease is closely related to the flowering season of plants that disperse allergenic pollen. There are 3 known categories of plants whose pollen has allergenic properties:
- wind-pollinated trees;
- cereals;
- weeds.
- Each type of plant has its own season of activity:
- Spring: from April to the end of May, flowering of wind-pollinated trees.
- Summer: from June to mid-July, pollen spread by cereal crops.
- Summer-autumn: end of July – September, weed flowering season.
- Pollen is released by flowering plants in the morning, but the maximum concentration is determined in the afternoon or evening. Fine pollen can be scattered for many kilometers around, and its allergenic properties persist for several hours. After rain, the air is practically free of pollen allergens.
Treatment of hay fever is determined by the phase of the disease: season of exacerbation or inter-relapse period.
Therapy during the exacerbation season
Elimination of etiological allergens.
- Antihistamines of the 2nd or 3rd generation. Histamine is recognized as the leading pathogenetic link involved in the development of hay fever.
- Antihistamines only work in the early stages of an allergic reaction (sneezing, watery eyes, mucus from the nose). Later, when other mediators (prostaglandins, leukotrienes) are added, when swelling of the mucous membranes of the nasal cavity and nasal congestion occurs, vasoconstrictors are prescribed.
- Cromoglynic acid derivatives (cromoglycates) are mast cell stabilizers. They act on the outer membrane of basophils and prevent the release of mediators from them.
Topical glucocorticoids have high anti-inflammatory effectiveness and reduce nasal and bronchial secretions. Systemic steroids are rarely prescribed for a short course, as they have numerous negative side effects on the body.
Symptomatic remedies: vasoconstrictor nasal drops (decongents) cause a narrowing of blood vessels, remove swelling of the mucous membranes, improve nasal breathing, relieve nasal congestion, but long-term use (more than 7 days) can provoke the appearance of drug-induced rhinitis.
A stepwise approach is used in treating the disease:
Stage 1, mild course: use antihistamines, cromoglycate. Stage 2, intermediate course, topical (local) glucocorticoids are used.
Stage 3, severe course - local glucocorticoids, antihistamines.
Inter-relapse period
- Elimination of risk factors: treatment of foci of chronic infection (carious teeth, pharyngitis, tonsillitis), getting rid of helminths and protozoa, treatment of concomitant diseases.
- Allergen-specific immunotherapy (ASIT) in various ways: oral, subcutaneous, aerosol, combined. The method allows to reduce the sensitivity of tissues to a specific antigen. This effect is achieved by introducing into the patient’s body specially selected minimum doses of the allergen with a slow gradual increase. ASIT reduces the symptoms of allergic inflammation by reducing tissue sensitivity to the allergen and mediators.
- ASIT is the only method of therapy that allows you to achieve long-term remission, delay further progression of the disease and prevent complications.
- Nonspecific immunotherapy.
Medicines for hay fever
generations: Suprastin, Tavegil, Fenkarol act quickly, but do not last long, so they are prescribed several times a day. Because of their ability to penetrate the blood-brain barrier and have a restraining effect on the functioning of the central nervous system (drowsiness, lethargy), they are not used in people whose occupation requires a quick reaction.
generations: Cetrin, Cetirizine, Erius act within 24 hours, do not depress the nervous system and can be used for a long time without developing negative side effects.
- Antihistamines of the second generation and cromoglycates begin to be taken 2 weeks before the expected start of flowering and continue to be taken until the end of the season.
- Cromoglycates are available in eye drops, nasal sprays, and inhalation aerosols: Intal, Cromohexal, Lecrolin.
- Vasoconstrictor nasal drops: Sanorin, Naphthyzin, Otrivin.
- Systemic glucocorticoids (tablets, intramuscular injections) are used for severe disease with episodes of bronchospasm and suffocation.