The nasal mucosa is an extremely important organ that performs the functions of cleaning, moisturizing and temperature regulating the inhaled air. It is a serious protective line that takes the first blow from pathogenic (disease-causing) microorganisms.
Even the strongest immune system, constantly exposed to the harmful effects of bacteria and viruses, fails from time to time.
In the case of the mucous membrane of the nasal cavity, we are most often talking about an inflammatory process.
In the accepted medical classification of diseases, inflammation of the nasal mucosa is called rhinitis. In common parlance, a runny nose.
On the one hand, symptoms of inflammation of the nasal mucosa are often observed during the cold autumn-winter period of the year. In such a situation, catarrhal runny nose can be an independent illness or accompany some kind of cold.
On the other hand, symptoms of inflammation of the nasal mucosa are often observed in the spring and summer. In this case we are talking about allergic rhinitis. Flowering time is the traditional time for the activation of allergic reactions.
These situations have only one thing in common - they both require timely and correct treatment.
Causes of inflammation of the nasal mucosa and types
Depending on the duration of the disease, acute and chronic rhinitis are distinguished, and often the second form develops in the absence of proper treatment in the acute phase.
A huge number of factors can provoke the occurrence of an inflammatory process in the nasal cavity.
It is on the basis of which of them caused the symptoms of pathology that different types of rhinitis are distinguished.
1
Catarrhal. Its appearance is caused by frequent acute respiratory viral infections, decreased immunity, serious pollution of the surrounding air with dust or combustion products, regular inhalation of tobacco smoke and an increased level of contamination of the internal surfaces of the nose with bacteria. The symptoms are moderate and do not cause significant discomfort to the patient.
2
Allergic. It develops against the background of allergens settling on the mucous membranes of the nasal cavity. Depending on its type, a runny nose can be present either exclusively in a certain season or throughout the whole year.
It is often accompanied by bronchial asthma, conjunctivitis or urticaria. A distinctive feature of this form of the disease is the presence of itching in the nose, increased lacrimation and frequent bouts of sneezing.
And sometimes white Vojacek spots are formed, which are the result of uneven spasm of blood vessels.
inflammation of the nasal mucosa: photo
3
Medication. The main reason for its appearance is addiction to nasal drops. It occurs much less frequently due to the use of antihypertensive drugs, tranquilizers or antipsychotics.
4
Atrophic. Develops when working in dusty, hot or excessively dry air. Sometimes it is a consequence of surgery or a genetic predisposition.
It is characterized by the formation of a large number of dry crusts, which are difficult to remove, and the mucous membrane bleeds.
5
Vasomotor. It is usually diagnosed in people with impaired vascular tone, that is, patients with hypotension, asthenovegetative syndrome, some endocrine pathologies, etc.
For this type of pathology, alternation of the sides on which congestion is observed is typical, but the distinguishing feature is inflammation of the nasal mucosa without a runny nose with crusts.
In the early stages of the development of the inflammatory process, only redness and swelling of the tissues are noticeable. As it progresses, crusts will form, causing irritation of the mucous membrane, and subsequently purulent discharge (during a bacterial infection).
If the nasal mucosa is burned: symptoms
Sometimes during steam inhalations, as well as in everyday life, if you accidentally inhale hot air or toxic substances, you can get a burn to the mucous membrane. This shows up:
- redness and swelling of tissues;
- dryness;
- the formation of bubbles filled with transparent contents;
- the appearance of erosions;
- the death of the outer layers of the mucous membrane, which is manifested by its graying.

The severity of the signs of a burn is directly dependent on its severity. In mild situations, usually only redness can be noticed, and only in the absence of attention to severe injuries does such a complication as epithelial necrosis occur. Source: nasmorkam.net
Causes
Inflammation of the nasal mucosa can be infectious or non-infectious. The infectious process is triggered by the following reasons:
- Viruses that often infect the nasopharynx and cause disease.
- Bacteria that enter the nasopharynx with inhaled air, as well as hematogenously from other sources of infection in the body.
- Fungi. Pathogenic fungi can also cause this disease. This may occur due to local or systemic infection of the body.
- The simplest. Sometimes mucosal irritation caused by mycoplasmas or chlamydia is diagnosed.
Inflammation in the nasal cavity can also be caused by a seasonal runny nose. In this case, the shells become inflamed for the period while the plants bloom en masse. This is most often observed in spring and summer.
In some systemic diseases, inflammation affects the nerve endings in the nose. In this case, neurovegetative rhinitis develops. In addition, the disease can be caused by nasal injuries, foreign bodies and operations.
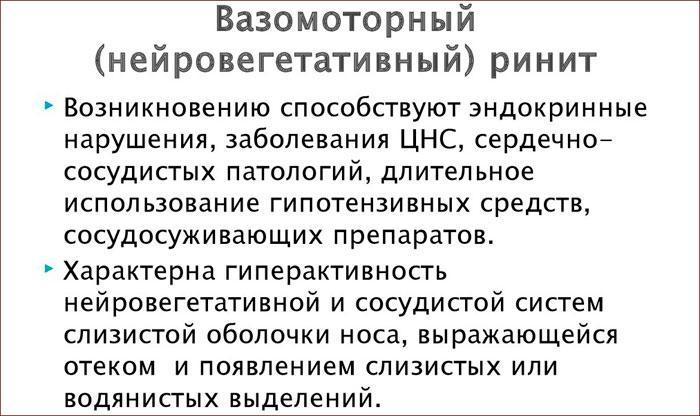
The cause of inflammation in the nose is often the uncontrolled use of certain medications. With prolonged use of vasoconstrictor drops, dryness of the mucous membrane occurs, as a result of which vasomotor rhinitis develops. This is why such medications cannot be used for more than 5 days in a row .
Inflammation of the nasal membranes can be caused by regular inhalation of too dry air and crying.
Diseases of the nasal mucosa
In addition to acute and chronic rhinitis, the inflammatory process in the nasal cavity can also be caused by:
1
Ozenoy. The disease is characterized by the formation of huge crusts and the presence of an unpleasant odor, which the patient himself does not feel.
2
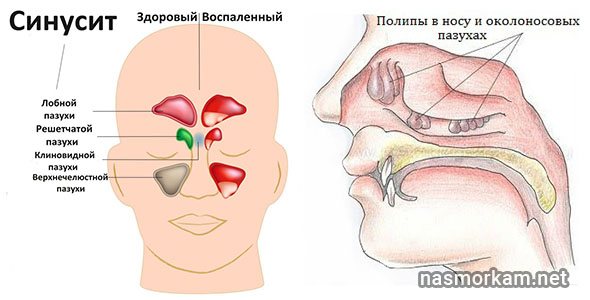
Sinusitis. This category includes sinusitis, frontal sinusitis, ethmoiditis and sphenoiditis, which are characterized by inflammation of the mucous membrane of the paranasal sinuses, and then the accumulation of pus in them. This leads to discomfort, headaches, severe nasal congestion, etc.
3
The presence of polyps. They are small neoplasms that develop against the background of the fact that the nasal mucosa is irritated for a long time by the action of any factors. The disease is characterized by difficulty breathing, headaches, hyposmia, stuffy ears and sleep disturbances.
Inflammation of the nasal cartilage, called perichondritis, is also sometimes diagnosed. It often develops due to injury, after which tissue infection occurs.
This sore in the nose manifests itself as pain, and upon rhinoscopy, a red tumor is found filling both nostrils. In such cases, the mucous membrane is usually damaged, since inflammation spreads to it.
How does the disease manifest itself?
Inflammation of this area can be acute or chronic. The acute process proceeds through a number of successive stages, which are accompanied by certain symptoms:
- At the first stage, the patient is bothered by itching and dry mucous membranes. This stage lasts from several hours to a day. At this stage, the infection begins to penetrate the mucosa.
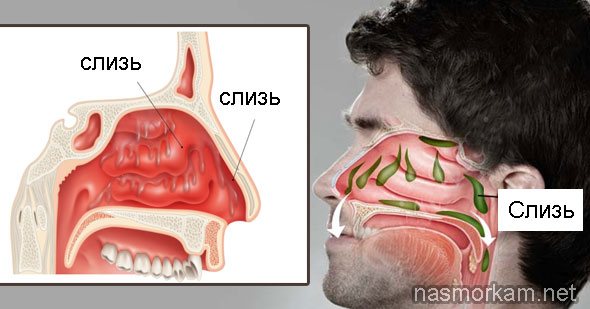
- At the second stage, the patient develops serous, profuse discharge, a stuffy nose, and a decreased sense of smell. In this case, symptoms of general intoxication of the body may occur: temperature rises, headache, aching bones.
- At the stage of purulent inflammation: the runny nose changes from clear to yellow or yellow-green. Purulent inflammation may indicate that the process has moved to the paranasal sinuses.
- During the recovery stage, the runny nose stops, the nose begins to breathe and the sense of smell gradually returns.
Important! With proper treatment, rhinitis can be abortive and end at stage 1 or 2. In the absence of treatment and reduced immunity, the process becomes chronic or is accompanied by complications, for example, inflammation of the sinuses.

Untreated acute form can become chronic or lead to complications
Manifestations of different forms of rhinitis can differ significantly from each other:
- With an allergic rhinitis, inflammation appears only upon contact with an allergen. A person’s nose becomes stuffy, and copious clear discharge begins to flow.
- With atrophic rhinitis and ozena, the main problem is dry nose and purulent crusts, which emit an unpleasant odor and greatly disturb the patient.
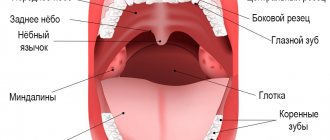
- With hypertrophic growth of the mucosa, in addition to discharge, the patient has serious problems with nasal breathing. He begins to breathe through his mouth due to swelling, which leads to inflammation of the pharyngeal mucosa and dry mouth.
In addition, there are special specific forms of runny nose associated with hormonal changes in the body. Thus, pregnant women develop vasomotor rhinitis, which is accompanied by swelling and discharge and goes away on its own after childbirth.
When to see a doctor
The reasons for visiting a doctor are:
- persistence of a runny nose and nasal discomfort for more than 2 weeks;
- sharp deterioration of condition after improvement;
- prolonged maintenance of high body temperature;
- severe deterioration in general health;
- presence of purulent discharge, etc.
In such cases, you should definitely contact an otolaryngologist and together with him choose the optimal treatment regimen.
In more detail: Otolaryngologist: what kind of doctor? What diseases does it treat?
Rhinoscopy of the nose (Endoscopy): what is it? Types, indications

In the absence of attention to your health and self-medication, life-threatening complications may develop, which include meningitis, damage to the trigeminal nerve, phlegmon, etc.
What diagnostics are needed to determine the causes?
In most cases, you can suspect the causes of a patient’s condition after communicating with him and performing rhinoscopy - a simple and fairly painless method of visually assessing the condition of the nasal mucosa. To confirm his assumptions, the doctor may refer him to:
- allergy tests to identify allergic reactions to various substances;
- laboratory analysis of nasal discharge;
- x-ray of the middle ear, paranasal sinuses, lungs, etc.

In rare cases, an additional CT or MRI is required to clarify the diagnosis. On the subject: MRI of the sinuses: what does it show and how is it done? Price
CT scan of the nasal sinuses: what does it show? Full description of the procedure. Price
Treatment of the nasal mucosa with medications
The nature of therapy is determined based on the detected causes of the inflammatory process. However, there are general recommendations:
- compliance with bed rest if there is a pronounced violation of the general condition;
- plenty of warm drinks;
- softening dry crusts with oil and carefully removing them, which is especially important if the mucous membrane is irritated;
- rinsing the nasal passages with saline solutions.
But in any case, the treatment of inflammatory processes of the nasal mucosa cannot be done without prescribing medications.
For patients whose mucous membranes are inflamed due to the activity of viruses or bacteria, it is recommended to use:
- antipyretics for fever, which also have an anti-inflammatory effect (Panadol, Nurofen, Imet, Rapimig, Efferalgan, etc.);
- colloidal silver preparations that effectively fight pathogenic microflora (Protargol, Deflu-Silver);
- vasoconstrictor drops and sprays to eliminate swelling and a feeling of congestion (Nazik, Noxprey, Otrivin, Xylo-Mefa, Xylen, Nazivin, Galazolin, Naphthyzin), but you should be careful with them and take only as prescribed by a doctor in recommended doses, since with them if exceeded, reactive hyperemia of the mucous membrane is possible;
- antibiotics (Augmentin, Hemomycin, Flemoxin-Solutab, Ospamox, Sumamed, etc.) necessary in the presence of a bacterial infection.

Allergic rhinitis is eliminated primarily by stopping contact with the substance to which there is increased sensitivity. And to eliminate the unpleasant manifestations of allergies, you can use antihistamines: Loratadine, Suprastin, Erius, Eden, Telfast, Claritin, etc.
Physiotherapy is often prescribed in addition to drug treatment. The most commonly recommended courses are:
- UHF;
- ultraviolet irradiation;
- microwave exposure.
Attention
In rare cases, surgery may be required. It is indicated in the presence of chronic rhinitis, caused by polyps, deviated septum, adenoiditis, or congenital anomalies in the anatomical structures of the nasal cavity.
How to relieve inflammation?
Medicines based on corticosteroids can quickly eliminate severe inflammation. But they can be used only if there are compelling indications; it is not recommended to start taking them on your own, since with prolonged use they provoke a decrease in local immunity.
These drugs include:
- Nasonex;
- Baconase;
- Flixonase;
- Avamis;
- Flunisolide, etc.

The effect after their use occurs within 2–4 hours and lasts throughout the day. Thanks to corticosteroids, you can quickly remove swelling, itching, sneezing attacks, as well as restore normal nasal breathing and reduce the amount of discharge.
They help when the inside of the nasal mucosa hurts, to treat allergic rhinitis, with adenoiditis and other pathologies.
The gradual elimination of inflammation is facilitated by antibiotics, which are used exclusively for bacterial infections. By destroying pathogenic microflora, they eliminate the causes of the production of inflammatory mediators, and it disappears. [ads-pc-1][ads-mob-1]
Features of treatment in children
In children, especially young children, chronic inflammation of the nasal passages practically does not occur. In most cases, the reason that the inside of the nose is red is ARVI.
But for infants, any hyperemia (overflow of blood vessels) is dangerous, since swelling and accumulation of mucus significantly complicate breathing. As a result, the baby cannot eat and sleep properly.
To ease your baby's condition:
- regularly remove snot using a special aspirator or a bulb with a soft tip;
- saline solutions are instilled up to 6 times a day;
- if necessary, use vasoconstrictor drops (before feeding, at night).

Older children are treated in the same way as adults, but the dosage of prescribed drugs is changed.
Since the main cause of the inflammatory process in children is mechanical damage to the internal membranes, the question often arises: how can a child heal small wounds?
In such situations, you should use sea buckthorn oil and antibiotic-based ointments, for example, Levomekol, tetracycline and others.
How to treat the nasal mucosa with folk remedies?
People often call for help from all kinds of traditional medicine in how to cure the nasal mucosa. In many cases, they can really help a person cope with the disease that has arisen, but sometimes they can also cause harm.
Therefore, before using them, it is recommended to consult a specialist, especially if a serious pathology is suspected. The most effective and safe methods include:
1
Steam inhalations. Peeled potatoes are boiled in water, which is then drained. Then the patient bends over the contents of the pan, covers himself with a towel and inhales the hot vapors through his nose. This procedure produces a warming and moisturizing effect, due to which not only dry crusts begin to come off more easily, but also accelerate tissue regeneration processes.

2
Rinsing with herbal decoctions (chamomile flowers, calendula, linden, string grass, yarrow, etc.). To prepare them, just pour a tablespoon of the selected plant material into a small container, pour a glass of boiling water and close the lid. After the infusion has cooled, it is filtered and the nasal passages are washed. Such procedures will moisturize the mucous membranes, improve blood circulation in them, help eliminate pathogenic microflora and allow tissues to recover faster.
3
Hot foot baths. They are carried out for a quarter of an hour, and to enhance the effect, mustard powder can be added to the water. This will help activate blood flow and shorten the duration of illness. But at elevated temperatures this method is contraindicated.
4
Decoction of pine buds. 50 g of raw material is poured with cold water, brought to a boil under the lid and cooked over low heat for 10 minutes. After cooling, the broth is filtered and taken together with honey or natural raspberry jam 5-6 times a day.
Thus, folk remedies can help with mild forms of inflammation. But for serious diseases they are used exclusively in addition to drug and physiotherapeutic therapy.
Comments (2)
Karina
07/28/2017 at 00:58 |
I try not to procrastinate with a runny nose. At the first sniffle, I wash it with an inexpensive morenasal spray. Cope with a runny nose in no time.Answer
Ira
03/14/2018 at 18:23 |
And I mix folk methods with traditional ones. A hot tea with raspberries or honey and lemon. Aquamaster spray, penetrates quickly. At night, you can smear the star on your forehead. You can steam your feet. But I don’t like washing.
Answer