Currently, there is practically no area of medicine where glucocorticosteroid medications . They have become widespread in all areas of medical practice. One of the most important of these substances is prednisolone.
Prednisolone is a glucocorticoid drug. It is a hormonal substance, an artificial analogue of the hormone hydrocortisone , produced by the adrenal cortex and, accordingly, has similar actions to it.
The drug has been very well studied and has been used in medical practice for quite a long time. It is active against many diseases.
The main functions of this substance:
- Anti-inflammatory. Associated with inhibition of the secretion of inflammatory mediators from mast cells - cytokines and histamine.
- Suppresses the immune system, as it interferes with the movement of immune cells, suppresses the functions of leukocytes, macrophages and the formation of antibodies.
- Antiallergic.
- Anti-shock.
It is worth noting that the number of cases in which patients would exhibit negative reactions is a small percentage . But, nevertheless, such a situation is possible, and it does occur. Therefore, you need to be prepared for it.
How to take Prednisolone correctly | How to reduce the dose and stop Prednisolone tablets
Prednisolone is a glucocorticosteroid drug with antiallergic and anti-inflammatory properties. Prednisolone is prescribed for use for diseases of all kinds of severity and origin. We suggest that you read the instructions - how to take Prednisolone correctly?
Hormonal treatment should be carried out only according to strict indications.
During treatment, it is necessary to remember that inhibition of the hypothalamic-pituitary-adrenal axis persists in patients receiving Prednisolone, even in a small dose (10 mg/day for 3 weeks or more), for a long time (up to 1 year) after discontinuation of the drug.
There is evidence that there is no significant inhibition of the hypothalamic-pituitary-adrenal axis if the dose of Prednisolone does not exceed 5 mg/day (1 tablet).
The development of side effects during treatment with prednisolone most often occurs in patients receiving more than 10 mg (2 tablets) per day.
In order to reduce side effects, the doctor may prescribe anabolic steroids and also increase the intake of potassium in the body (diet, potassium supplements), calcium and vitamin D.
Since Prednisolone promotes the formation of blood clots, it is necessary, together with the hormone, to regularly take blood-thinning drugs, such as Curantil, Thrombo-ACC, Aspirin-Cardio.
During treatment with Prednisolone (especially long-term) you need to:
- see an ophthalmologist;
- control blood pressure and water-electrolyte balance;
- regularly donate blood for analysis (glucose, ESR, C-reactive protein).
How to take Prednisolone correctly - dosage and time of day
In the acute period of the disease, Prednisolone is prescribed at a dose of 1-2 mg/kg body weight. Standard: 4-6 tablets of prednisolone (20-30 mg) per day. After stabilization of the condition, the dosage is reduced according to the scheme (see below).
In the most severe cases, the doctor may prescribe up to 100 mg (20 tablets) of prednisolone per day. In this case, distribute the daily dose into 2-4 doses.
The maintenance dose (after stabilization of the condition) is 3 times lower than initially prescribed.
How to take Prednisolone for uncomplicated diseases
At the beginning, the daily dosage of prednisolone is divided into 3 doses, then switched to a single dose of the drug in the morning.
Take prednisolone from 6 to 10 am in accordance with the rhythm of the adrenal glands.
Take hormonal tablets during or immediately after meals.
It is correct to take prednisolone with milk so as not to injure the stomach. Milk reduces acidity and is a source of calcium.
Do not stop prednisolone quickly, reduce the dosage evenly. Abruptly stopping taking the pills can lead to an exacerbation of the existing disease, as well as a failure of the adrenal glands.
How to reduce the dose of Prednisolone correctly without consequences
The daily dose of prednisolone is gradually reduced, taking into account the results of clinical and laboratory tests of the patient’s blood, including determination of ESR and C-reactive protein.
In medical studies, prednisolone at a dose of 15 mg/day was gradually reduced to 8 mg/day (2.5 mg per month) and then by 1 mg every 2 months until discontinuation. The results of these studies indicated optimal control of disease activity during the study period. In contrast, faster dose reductions resulted in less favorable results.
Thus, after reducing the dose of prednisolone to 10 mg/day, it should subsequently be reduced by less than 1 mg per month (for example, 1 mg every 2 months).
The dose reduction scheme to 10 mg/day provides for its reduction by no more than 2.5 mg per month, no more than once a month (for example, once every 2 months). The initial volume of prednisolone is reduced by 2.5 mg monthly or every 2 weeks to 10 mg/day, and then by 1 mg every 6–8 weeks until treatment is discontinued.
How to take Prednisolone according to a scientific scheme and reduce it from 8 tablets to complete withdrawal (treatment period is 2.5 years):
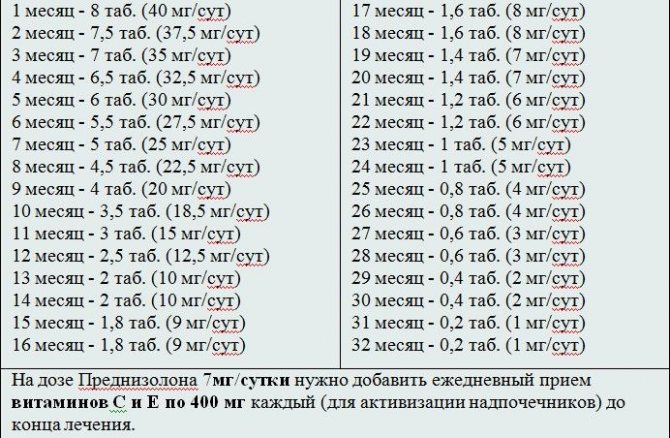
Standard regimen for taking prednisolone (course of treatment for 1 year):
0.8-1 mg/kg for 8 weeks, followed by a slow dose reduction for another 8 weeks and switching to a maintenance dose (10-15 mg/day) for 6 months.
How to take Prednisolone according to the schedule and reduce it from 12 tablets to complete withdrawal:
If you subtract 1/2 or even a full tablet (5 mg) from a daily dose of 60 mg, this is less significant for the body than subtracting the same amount of a hormonal drug from a dose of 10 - 15 mg/day. In other words, the higher the exogenously administered dose of the hormone, the less significant the initial dose reduction is for the patient’s body.
Having started reducing the dose from 60 mg, you can reduce it by 1/2 table. in 3 - 4 days, that is, in one week for 1 tablet. Having reduced the amount of prednisolone in the proposed rhythm to 40 mg/day, a further reduction in the daily dose is carried out by 1/2 table. in Week.
With a daily dose of 30 mg, you can continue to reduce by 1/2 table. per week (this is more convenient for the patient), but after each subsequent dose reduction they take a week-long pause. During this period, the body “gets used” to the available daily dose of glucocorticosteroid hormones. A week later, the volume of prednisolone is again reduced by 1/2 tablet. In fact, each subsequent reduction in the dose of the drug occurs once every 2 weeks.
With a daily dose of 10–15 mg or 8–12 mg, the rate of reduction of prednisolone remains the same, but the dose is reduced not by 1/2, but by 1/4 of the table. in Week.
We hope that our instructions will help answer the pressing question: “How to take Prednisolone correctly.”
“Assault” therapy drug
Prednisolone is a hormonal drug
Prescriptions of the drug are made exclusively in emergency cases, when the main therapy does not lead to an adequate result, or the treatment begins to take a protracted nature. If the clinical picture is unsuccessful, the prescription is carried out in a short course using high doses of the drug. Long-term use of large amounts of Prednisolone can cause protein deficiency in the blood plasma, which threatens a toxic release of free progesterone. Reasons why Prednisolone is classified as a hormonal drug:
- Deficiency of progesterone in plasma protein, as a rule, leads to dysfunctions of growth and sexual development of adolescents during maturation, or during adolescence.
- Prednisolone causes an increase in blood sugar levels in patients with diabetes. In addition, the drug is capable of simultaneous actions to enhance the breakdown and new formation of fat cells deposited in tissues, which leads to a transient process of obesity.
- Excess Prednisolone leads to disruption of mineral metabolism, since the drug is able to remove potassium from the body, thereby reducing myocardial contractility. This leads to myocardia and the risk of heart attack.
- Prednisolone removes calcium from the body, which leads to osteoporosis, or thinning of the bones. Bones become brittle and can break from a slight bruise.
- The action of the drug causes water and sodium to be retained in the cells of the body, causing serious swelling.
The drug Prednisolone is produced in various forms, according to the recipe: powder, injection solution, injection suspension, oral liquid, oral suspension, oral syrup, oral tablets, dissolving tablets for oral use.
How to avoid side effects when taking corticosteroids?
In addition, it is corticosteroids taken in the afternoon that cause side effects more quickly. Therefore, by setting the correct hours for yourself to take your medication, you can reduce your dose and reduce harmful side effects.
If you have to take large doses of the drug, it is better to take them at once, say, at three-minute intervals, with plenty of water, but at exactly the right time.
If the disease is not acute, then we advise you to take prednisolone not daily, but every other day, but in a double dose. In many cases, this also helps reduce side effects.
A very important rule. It is safe to stop taking corticosteroids only if the patient has been using them for no more than 10 days. If longer, then you need to stop taking it very slowly, over the course of months, gradually reducing the dose. Otherwise, there is a high risk of exacerbation of the underlying disease and the occurrence of side effects.
Rheumatology patients should not take polcortolone (also known as triamcinalone). Polcortolone will only worsen the disease, causing damage to the musculoskeletal system.
With long-term use of prednisolone, the adrenal glands often atrophy, resulting in adrenal insufficiency. This is a dangerous disease, but it can be avoided. Medicines should be taken only in the early morning, because prednisolone taken during the day suppresses the activity of the adrenal glands. Medicines should be taken every other day, but in double doses. It is better to reduce the dose to the minimum possible, if the course of the disease allows.
Dexamethasone should not be prescribed unnecessarily and for a long period of time. It affects the adrenal glands tens of times stronger than prednisolone.
When taking corticosteroids for a long time, it is necessary to warn doctors if any other disease occurs, or during an upcoming operation.
Another complication is steroid diabetes. To avoid it, you need to completely eliminate sweets and baked goods from your diet.
Another possible complication is osteoporosis. If prednisolone is prescribed for a period of more than a month, it is mandatory to take calcium supplements along with vitamin D. For example, Calcium-D/3 nikomed, Complivit calcium D/3, etc.
How not to get sick? Who and where should you turn if you are already sick? What to do before meeting with a doctor? How to navigate the world of analyzes and examinations? Which ones are informative and which ones are useless? How to say thank you to the doctor without breaking the law? You will learn about this and much more from the blog materials.
What is better: taking prednisolone for a long time or stopping it quickly?
And the involvement of the kidneys and central nervous system in the inflammatory process, suppression of hematopoiesis, and the addition of an infectious disease creates a huge number of new problems, and in order to “jump out” of such an exacerbation, the dose will need to be increased not by 2 times, but sometimes by 20-30 times! In such a situation, even the most advanced medicine will not have time to help; the money may simply run out or not be enough to provide adequate treatment!
We must not forget that a “rheumatological” patient needs to constantly invest money in medications for the rest of his life to maintain his health.
Landmark: A) – consultation with a doctor! B) - again, do the above tests, which need to be checked before each dose reduction, and study them in detail, comparing them with the norm. C) listen to yourself carefully. (I don’t mean listening to every twitch of a muscle, movement of an intestine full of gas, “crawling goosebumps” - this path leads to a neurologist/psychologist at a minimum, and most often to a psychiatrist). D) - if reducing the daily dose of hormonal drugs leads to a worsening of the condition, go back to the previous dose, where you felt normal.
Prednisolone is a glucocorticosteroid product with antiallergic and anti-inflammatory properties. The drug is prescribed for several diseases of varying severity and origin. “How to take Prednisolone correctly?”
Prednisolone is prescribed for allergic, rheumatoid arthritis, autoimmune diseases (scleroderma, systemic lupus erythematosus and dermatomyositis), skin diseases (eczema, psoriasis, joints, various types of dermatitis, etc.), for any diseases of the eyes, mild, kidneys, cerebral edema, gastrointestinal tract. During organ transplantation, the drug is indicated to treat graft rejection. In oncology, prednisolone is taken during chemotherapy to eliminate nausea and vomiting. Each tablet contains 5 mg of the active drug. During the acute period of illness, take 4-6 tablets per day. After the condition has stabilized, reduce the daily dose to 1-2 tablets. Take medication 1 daily, preferably at 6-8 am. In the most difficult situations, the doctor can prescribe up to 100 mg (20 tablets) of prednisolone per day. Then distribute the daily dose of medication into 2-4 doses. In the acute period of the disease, children are prescribed prednisolone at a dose of 1-2 mg/kg body weight. Distribute the medication into 4-6 ways. The maintenance dose (after stabilization of the condition) is three times lower than the medical dose. Take the tablets while eating or immediately after eating. Take the medication with a small amount of water. Do not cancel the product quickly, as usual, since the healing took a long time. Reduce the dose evenly.
On the topic, prednisolone itself is considered a systemic product; its effects affect the entire body. Its use can have both a beneficial and negative effect on almost all organs. This product has a great influence on the metabolism of major drugs in the body. With all this, sodium ions and water accumulate in the body, nitrogen deficiency, potassium ions are excreted, high sugar content, weight gain due to fat accumulation. Prednisolone also affects the functioning of the endocrine glands. The function of the adrenal glands suffers, in children the hormone is inhibited, in women the menstrual cycle is disrupted, the metabolism of sugars is disrupted, and a lack of insulin is sometimes noticed. The functioning of the heart and blood vessels is disrupted. Blood pressure increases, heart failure may appear, blood clots form, blood clotting becomes more difficult, electrocardiogram abnormalities indicate a lack of potassium. Since the patient has previously suffered a heart attack, the dead portion of the heart muscle increases in size. The number of muscle sizes decreases quickly. Muscle inclination, poor bone texture, possible fractures of bones and vertebrae. All this will help you answer the question: “How to take Prednisolone correctly.”
Post Views: 420
Consequences of using prednisolone
- Increases the risk of developing osteoporosis by suppressing bone growth (slows down its mineralization). Frequent fractures, aseptic necrosis of bones.
- Muscle hypotonia or atony.
- Calcium and potassium deficiency, excess sodium accumulation. Slows down the absorption of potassium and calcium from the gastrointestinal tract.
- “Steroid dementia” or degeneration of memory, mental activity, and behavior.
- Fluid homeostasis disorder , water retention in the body. Occurs due to a decrease in the permeability of the vascular walls and subsequent vasoconstriction. Edema syndrome. Increase in body weight.
- Impaired memory and attention.
- Increased blood pressure . Risk of cerebral stroke.
- Reduces the rate of protein synthesis in muscle tissue, resulting in muscle pain and muscle atrophy.
- Promotes the development of hyperglycemia , as it enhances the absorption of glucose from the digestive tract and stimulates the flow of sugar from liver cells into the blood. Steroid diabetes mellitus develops.
- Inhibits the synthesis of its own steroid hormones (endogenous). Inhibits the functionality of the adrenal glands.
- Itsenko-Cushing syndrome.
- From the digestive system : nausea, vomiting, peptic ulcer, hiccups, dyspeptic symptoms (heartburn), pancreatitis, esophagitis, increased appetite, bloating.
- From the heart : rhythm and conduction disturbances (bradycardia, arrhythmia), arterial hypertension, changes in electrocardiogram parameters, chronic heart failure, obliterating endarteritis.
- Mental and nervous disorders : hallucinations, headache, dizziness, irritability, nervousness, depressive syndrome, spatial orientation disorder, euphoria, vertigo, paranoia, cerebellar pseudotumor, increased intracranial pressure, seizures.
- From the organs of vision : infectious and inflammatory diseases, glaucoma, increased intraocular pressure, damage to the optic nerve, loss of vision, trophic disorders in the cornea, steroid exophthalmos, double vision, cataracts, thinning and perforation of the cornea, myopathy.
- Slow wound healing, that is, regeneration processes.
- Loss of consciousness.
- Hirsutism or increased hair growth throughout the body.
- Virilization . The appearance of male traits: low timbre of voice, body type.
- Increased sweating.
- On the skin : the appearance of acne, skin rash, itching, burning, atrophic changes in the skin and subcutaneous tissue, abscesses, secondary infectious skin lesions.
- Fungal infections (candidiasis) of the eyes, skin and nails, vagina.
- Increased blood clotting , often the development of thrombotic complications, thromboembolism. Result: infarction of various organs (heart, kidneys, liver, lung, brain).
- When instilled into the eyes, increased secretion of tear fluid is possible.
- Frequent exacerbation of infectious pathologies.
- Allergic reactions are possible . Anaphylactic shock up to the death of the patient is not excluded.
- Acute adrenal insufficiency.
- Menstrual irregularities : dysmenorrhea, amenorrhea. Associated with suppression of the secretion of sex hormones (estrogens, follicle-stimulating hormone, luteinizing hormone).
- Withdrawal syndrome . It manifests itself as an exacerbation of the underlying disease.
- Numbness, paresthesia, pain, necrotic lesions, and cicatricial changes may appear at the injection site.