House dust as an allergen
The most common cause of atopic asthma in adults is house dust. In our material, sensitization to house dust was detected in 100% of patients with this form of the disease. House dust is a natural product of human life, but its antigenic composition varies in different climatic zones and living spaces.
During the observation of patients, features in the clinical course were identified, which were associated with the spectrum of causally significant allergens.
Allergological examination of 408 patients included a full set of allergens up to 100 items. The examination was carried out using house dust allergens, dermatophagoid mites, feather allergens (pillow feathers), animal allergens (cat, dog, rabbit, sheep wool) 15 types of pollen, 32 types of food, fungal, bacterial allergens.
One patient could identify from 8 to 38 allergens. Depending on the spectrum of allergens, the combination of 2, 3 and 4 groups of allergens, the clinical course of asthma had its own characteristics. Strongly positive allergic reactions to regional household and epidermal allergens were noted.
For patients with bronchial asthma living in the Kabardino-Balkarian Republic, a regional house dust allergen was prepared, collected in the homes of 20 patients who had no effect of treatment during SIT with standard commercial allergens. The implementation of SIT with “regional” allergens has improved the therapeutic effect of immunotherapy.
In patients with bronchial asthma who were under our supervision, an allergological examination revealed household sensitization, i.e., an allergy to house dust and feather pillows in 100% of patients. In addition to the main form of sensitization, there was a concomitant allergy to pollen (25.9%) and food allergy (38.9%).
The antigenic properties of house dust depend on the presence in it of various species of microscopic mites, for which house dust is a favorable habitat, especially for mites of the genus Dermatophagoides pteronyssinus. Bedding, including feather pillows, is a favorable environment for ticks to breed. The ideal condition for the development and reproduction of ticks is also high air humidity (75 - 80%). In houses with increased dryness, there are no dust mites or only a small number. In damp, old rooms, mites of the genus D. pteronyssinus are found more often.
Some patients experience seasonality in the manifestation of the disease, i.e., an increase in asthma attacks during warm periods of the year. The seasonality of the appearance of symptoms of bronchial asthma is associated with the development and reproduction of ticks during this period.
The allergenic composition and antigenic activity of the allergen from house dust depend on climatic and geographical factors. The prevalence of ticks varies in different regions. In the Krasnodar region, mites were found in 51.2% of house dust samples, in Moscow, mites were found in 60% of samples, in the Rostov region in 73.5%, in the Republic of Kazakhstan - in 47.3%, in the Chuvash region - in 100%, in Lithuanian - 96%.
In foreign countries with a humid maritime climate, such as Holland, Japan, Yugoslavia, Bulgaria, sensitization to ticks among patients with bronchial asthma ranges from 70 to 100%.
According to our observations, in the clinical course of bronchial asthma, 51.4% of patients with household and epidermal allergies had pronounced sensitization to house dust mites, which was confirmed by the sharply positive results of skin allergy tests with the mite allergen and PACT data. More patients with severe sensitization to mites were identified among adults than among children.
Atopic bronchial asthma, associated with sensitization to mites, was caused by the living conditions of patients, usually located in old, damp, dark rooms, in houses with stove heating, more often in rural areas, with a large number of pillows and feather beds, where there were good conditions for development and mite reproduction. In these same patients, a predominant occurrence of asthma attacks was noted at night, usually 2-3 hours after the onset of sleep, a clear elimination effect, i.e., cessation of asthma attacks in the hospital or when changing place of residence.
A study of the seasonality of the manifestation of allergy to mites showed that in some patients, seasonality in the disease was found, i.e., a clear connection between periods of exacerbation of the disease and the season of the most active reproduction of the mite. Thus, 10.4% indicated an increase in asthma attacks in April-May, 20.8% - in June-July. Attacks of asthma became especially frequent in August-September-October, which often caused diagnostic errors: bronchial asthma was regarded as infectious-allergic, the exacerbation of which is associated with the onset of cold weather (Table 10).
According to our observations, the clinical course of bronchial asthma with a pronounced tick-borne component depended on the ecology of the home: in 54.3±5.1% of patients, attacks of suffocation occurred only in the house.
With seasonality associated with the tick-borne component of household allergies, patients noted that in the period August-September-October, attacks of suffocation at home at night, in bed, became more frequent. At the same time, there was little concern about rhinoconjunctival syndrome, in contrast to patients with pollen seasonality, when attacks of suffocation developed against the background of rhinoconjunctival syndrome.
Atopic bronchial asthma with a pronounced tick-borne component was mostly severe; asthma attacks occurred every night, with a sharp deterioration in the condition in the autumn.
In patients with severe asthma, asthma lost its atopic features, since manifestations of pulmonary insufficiency and associated bronchitis came to the fore in the clinical picture. In all these patients, in local clinics, asthma was interpreted as infectious-allergic and in some it was already hormone-dependent.
Determination of the total revealed fluctuations in its level from 153 to 2000 IU/ml, and the average value was 653.7 ± 33.2 IU/ml. When performing skin allergy tests with a mite allergen, the majority showed sharply positive reactions.
Here is an extract from the medical history
Patient K. X., born in 1959 (case history No. 1172) went to the allergology office. He has been suffering from bronchial asthma for several years. Notes attacks of suffocation at home at night. Lives in the village. The house is one-story, damp, dark. He sleeps on a feather bed. Attacks of suffocation occur at home at night, as soon as one goes to bed. The patient has especially severe attacks of suffocation in August-September. This period is difficult not only because of the flowering of ragweed, but also because it coincides with the period of active tick reproduction. The patient received two courses of specific treatment with house dust and pillow feather allergen. The treatment had no effect. In the third year, the patient was examined with a mite allergen. The reaction was sharply positive, and the patient was given a course of specific immunotherapy with household and epidermal allergens, including the mite allergen. The effect was good. The patient changed his place of residence. A few months later, his wife brought his old feather bed, on which he had slept before. On the same night, an attack of suffocation developed. The patient correctly assessed this fact: he took out the mattress and his condition improved.
This example confirms the presence of bronchial asthma with a pronounced tick-borne component.
In 48.6% of patients, it was not possible to identify a clearly expressed tick-borne component, since most of them (55.6%) lived in modern apartments with good living conditions. Attacks of suffocation also occurred at home at night, but did not have a pronounced elimination character and did not depend on changes in living conditions. The atopic form of the disease in this group of patients was confirmed by positive results of skin allergy tests with household and epidermal allergens. They were not allergic to ticks.
Fungal tonsillitis
Have you been trying to cure FUNGUS for many years?
Head of the Institute: “You will be amazed at how easy it is to cure fungus by taking the product every day for 147 rubles ...
Read more "
Fungal or candidal tonsillitis photo
The body of a healthy person constantly contains various fungi and microorganisms. They practically do not manifest themselves, being an integral part of the opportunistic microflora. When immunity decreases or there are health problems, fungi can begin to actively reproduce, causing serious internal diseases and inflammation. One of these is fungal tonsillitis - a special type of infection of the throat mucosa, which requires specific treatment.
Causes of the disease
Candidal tonsillitis or fungal tonsillitis
Despite infection and inflammation in the throat, you should not call this type of mycosis fungal tonsillitis. The second name of the disease is tonsillomycosis. The disease visually resembles the more common streptococcal sore throat and is a fungal infection of the tonsils.
The main pathogens that cause tonsillomycosis are yeast or putrefactive fungi from the genus Candida. Therefore, doctors sometimes call the disease candidal tonsillitis. In rare cases, mycoses such as Saccharomycetes are isolated. It always develops without a pronounced acute period, but can be complicated by interaction with pathogenic streptococci.
Almost always, fungal tonsillitis occurs against the background of severe weakening of the body after any colds or viral diseases.
Other common causes and predisposing factors are:
- weakening after a diet or vitamin deficiency;
- chronic diseases of the nasopharynx or tonsils;
- hidden inflammatory processes of internal organs;
- poor nutrition;
- smoking;
- endocrine disorders;
- prolonged and uncontrolled use of strong antidepressants;
- oncological diseases.
Candidiasis tonsillitis or fungal tonsillitis
Due to the characteristics of age and immunity, candidal tonsillitis is more common in young children. Cases of the disease in the first year of life are directly related to the familiarity of the child’s body with pathogenic microflora. The main reason in this case is complications after thrush or dysbacteriosis.
More often than others, fungal tonsillomycosis is diagnosed in patients with certain problems:
- those suffering from HIV;
- having chronic candidiasis;
- leading an antisocial lifestyle;
- using dentures;
- who have undergone radiation or chemotherapy.
Experts emphasize that this type of mycosis always occurs against the background of a combination of two factors:
- the body's defenses cannot restrain the development of pathogenic fungi;
- the number of beneficial bifidobacteria, which inhibit the growth of candida, decreases.
Fungal tonsillitis symptoms
Fungal sore throat photo
Most experienced otolaryngologists can distinguish fungal tonsillitis in children and adults by the appearance of the throat mucosa. A large number of small white spots appear simultaneously on the palate and tonsils. They can cover almost the entire inner surface of the pharynx, tonsils and posterior wall. When the candida pathogen predominates, this plaque has a white, milky tint. If the fungi are moldy, it takes on a greenish color.
Pensioners! Don't cut fungal nails! They are derived simply: take 9 grams...
Military doctor: So that the soldiers do not have fungus, they 2 times a day...
Other characteristic symptoms are:
- unpleasant sourish odor from the mouth;
- painful sensations when swallowing;
- feeling of a lump in the throat, soreness;
- weakness of the body;
- violation of taste perception;
- enlarged lymph nodes in the neck.
Fungal tonsillitis in advanced form
The acute period for mycosis lasts from 7 to 10 days. It is characterized by an increase in temperature, loss of appetite and a general deterioration in well-being. If the patient self-medicates or the therapy is incorrectly selected, tonsillomycosis develops into a chronic form. It is characterized by a constant alternation of complete rest and a sharp relapse, especially after a cold.
If the disease affects the baby's body against the background of thrush, the child becomes restless, refuses to drink or bottle, and sleeps restlessly. It is difficult for parents to understand the reason for the sudden change. And when breastfeeding, the fungus is constantly transmitted from mother to baby. A hint may be flaking on the mammary gland, itching or redness.
Possible complications
With a severely weakened body and low level of immunity, the disease becomes chronic. The fungus spreads through the lymphatic system and multiplies in soft tissues and internal organs. In an advanced state, fungal tonsillitis can cause inflammation of the heart muscle and kidneys, disrupt the functioning of the liver and intestines, and provoke rheumatic changes in the joints.
The absence of complex antimycotics in therapy leads to inflammation of the appendix, otitis media with complications, abscesses and cervical lymphadenitis. Therefore, the disease requires careful systemic diagnosis and compliance with all instructions of the attending physician.
Diagnostic methods
Any sore throat can lead to complications, so at the first symptoms you should consult an otolaryngologist. He determines the necessary studies and tests that will help identify the main pathogen and select an antifungal agent.
After a preliminary examination, a scraping of plaque on the tonsils and larynx is taken through a laryngoscope. Additionally carried out:
- sowing material to determine mycosis;
- microscopic examination.
The main difference from ordinary sore throat is the rapid spread of whitish plaque throughout the entire oral cavity, including the tonsils and pharynx, which is not typical for the bacterial form.
Fungal tonsillitis treatment
Candide solution for thrush
An integrated approach to the treatment of fungal tonsillitis is aimed at restoring the balance of healthy microflora and strengthening the immune system. The basis is the use of special antimycotics: Fluconazole or Nystatin. In case of severe allergies, they can be replaced with Orungal or Pimafucin, which are effective in the presence of candida fungi.
The treatment plan must include the following procedures:
- taking immunostimulants;
- treatment of the infected throat mucosa with anti-inflammatory sprays (Hexoral or Chlorphillipt);
- removing plaque using antifungal solutions of Candida, Livaron or Clotrimazole;
- irradiation of the zone of formation of fungal tonsillitis with ultraviolet light;
- additional antibiotics (if necessary).
The patient is recommended to take a complex vitamin composition, balance his diet and give up his bad habits. When treating infants, an examination of the mother is required.
For candidal tonsillitis, experts recommend supplementing therapy with some folk recipes:
- gargling with the addition of fir, tea tree or sage oil;
- treatment with decoctions of chamomile or calendula;
- use propolis tincture, honey with the addition of a few drops of lemon juice.
A simple soda solution removes plaque well and helps reduce fungal activity. Rinsing with such an alkaline composition kills the pathogen and reduces unpleasant symptoms, especially in the presence of candida.
To prevent relapse, you need to pay more attention to your immunity and treat any inflammation in a timely manner. The condition of the intestines and the absence of dysbiosis are of great importance, so regular nutrition with fermented milk products should become a pleasant and tasty habit.
Features of bronchial asthma. Combined sensitization
Combined sensitization is the result of polyvalent sensitization to 3–4 groups of allergens.
Combined allergies create difficulties both in the process of diagnosing the disease - determining the spectrum of allergens, and in the correct choice of treatment tactics and the sequence of treatment with allergens when carrying out specific immunotherapy.
Manifestations of combined allergies can occur through delayed, immediate, and mixed types of allergic reactions and include sensitization to diverse allergens.
Combined sensitization of pollen etiology is observed in widespread diseases: atopic bronchial asthma, hay fever, allergic rhinitis, food and drug allergies.
A significant increase in the number of patients with simultaneous combined hypersensitivity to various allergens of non-microbial origin (household, epidermal, pollen and food), causing the formation of immediate-type hypersensitivity in the body with long periods of exacerbation and a severe course of the allergic process, poses the problem of developing methods for correcting these conditions. The problem of polysensitization to pollen and food allergens is presented in detail in the studies of S. X. Khutueva.
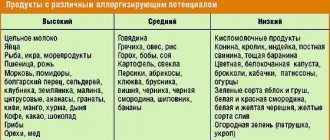
Fungal and food sensitization
What it is? This is the body’s reaction to a fungus, which can be both in the air and on the mucous membranes and horny integuments of a person; most often it manifests itself after a skin fungus has been transferred. Fungal sensitization is also a cause of asthma. Since the fungus is widespread in nature, it is often an unnoticed cohabitant with a person in any, even the cleanest house. Fungi can live not only in dust and walls, but also in the refrigerator, pantry, on food or any cotton products.
The phenomenon of food sensitization occurs as a result of many factors: poor heredity, mother’s refusal to breastfeed, helminthiasis, hypovitaminosis, and any problems with the gastrointestinal tract, which weakens the immune system. There is a concept of cross allergy. For example, if you are allergic to goat's or cow's milk, you may be sensitive to beef or goat meat. And also to the meat of other animals.
Household sensitization develops in several stages:
- Eating food causes rejection or any negative reactions. If you notice something like this, be sure to immediately consult a doctor, take the medications prescribed to you and follow a diet.
- Chronic sensitization. At this stage, neither diet nor antihistamines no longer have any effect on the sensitized organism.
Sensitization should not be allowed to develop until the last phase. Since at this stage of development of the disease it is already very difficult to cure the disease, and even if the irritants are completely excluded, the chances of healing will be low. The patient is treated through diet, medications and a course of special antibiotics, under the strict supervision of specialists.
Criteria
Allergies to pollen include allergies to fruits and vegetables. In patients with hypersensitivity to birch pollen, apples, cherries, peaches, apricots, pears, carrots, and celery act as food allergens. Our studies describe an acute allergic reaction in the form of anaphylactic shock that developed when drinking grape juice in a patient with sensitization to Asteraceae pollen and ragweed pollen.
Despite individual studies conducted to study combined sensitization to non-infectious allergens, the features of the clinical course of bronchial asthma with combined allergies depending on the allergen spectrum remain unstudied at present. The relationship between clinical and immunological diagnostic criteria has not been developed.
We observed 213 patients with combined sensitization to 3 and 4 different groups of non-infectious allergens. Of these, 50.2% of patients had a combined allergy to household epidermal and food allergens; 25.3% were found to be sensitized to household, epidermal and pollen allergens, and 24.5% to 4 groups of allergens (household, epidermal, food and pollen) (Table 13).
Combined sensitization to household, epidermal and pollen allergens was determined in 25% of patients with bronchial asthma.
Features of the clinical course of bronchial asthma depended on the allergen spectrum and clinical manifestations of pollen sensitization.
With combined household and epidermal allergies with concomitant sensitization to meadow grass pollen, as a rule, asthma had a benign course, since pollen allergy was accompanied only by rhinoconjunctival syndrome.
When household and epidermal allergies were combined with sensitization to weed pollen, namely ragweed pollen, asthma acquired a recurrent malignant course, since in most patients the allergy to ragweed pollen was accompanied by pollen asthma.
If household asthma was combined with an allergy to the pollen of meadow grasses and weeds, then during the flowering of meadow grasses, rhinoconjunctival syndrome was observed, and during the flowering of weeds, severe attacks of suffocation were added due to an allergy to ragweed.
Pollen sensitization in most cases was accompanied by pollen asthma: during the flowering period of ragweed, patients had severe asthma attacks that were difficult to stop due to the high concentration of ragweed in the air. Attacks of suffocation continued in winter due to existing household allergies, but were easier and were not accompanied by severe rhinoconjunctival syndrome. In patients, pollen asthma corresponded to the flowering period of meadow grasses.
The occurrence of pollen allergy was confirmed by the presence of a positive nasal challenge test with ragweed allergen, positive results in PACT and a positive basophil test. In those patients in whom the summer seasonality of the disease was also due to sensitization to ticks, there were differences in the clinical manifestations of the disease. If asthma attacks developed with an allergy to ragweed against the background of rhinoconjunctival syndrome, the condition of the patients sharply worsened during the day, especially in sunny weather.
With a pronounced tick-borne component, attacks of suffocation prevailed at home at night, in bed. During the day, patients noted constant, sometimes increasing, difficulty breathing. The condition of the patients sharply worsened due to exposure to the “culprit” allergens: during the day there was a high concentration of ragweed pollen in the air, at night there was close contact with the tick-borne allergen. The presence of a “tick-borne” component in pollen-induced bronchial asthma made it difficult to differentiate between atopic and infection-related forms of the disease.
We give an example of severe bronchial asthma with combined household, epidermal and pollen sensitization.
Extract from the medical history No. 5812
Patient B.A. was sent to the allergy center by a local doctor with a diagnosis of bronchial asthma of the infectious-allergic form.
The patient complains of asthma attacks in winter and summer, runny nose, nasal congestion, shortness of breath, cough with mucous sputum.
He first fell ill at the age of 7, when in the summer he began to worry about runny noses, sneezing, itchy eyes, and then attacks of suffocation appeared. Until the age of 15, I was sick only in the summer. He was treated by a local doctor on an outpatient and inpatient basis. From the age of 23, the disease began to bother me in winter, and the disease became year-round. In winter, attacks of suffocation occurred more often at home at night. In the summer, August-September-October was considered a particularly difficult period. Unreasonable runny nose, sneezing, and periodic nasal congestion bothered me both in winter and summer.
The patient's condition especially worsened at the age of 37, when frequent asthmatic conditions were the basis for prescribing prednisolone (30 mg per day according to the regimen) at the local clinic. The attacks of suffocation were severe and difficult to stop. The patient lost his ability to work, and at the age of 40 the patient was assigned disability group 2. Despite the fact that the maintenance dose of hormonal drugs was 4 tablets of prednisolone per day, attacks of suffocation continued to bother me. He used inhaled sympathomimetics and theophedrine.
Prevention of sensitization
The general principles of S. prevention boil down to reducing the intake of various allergens into the body and eliminating conditions conducive to S. This requires constant improvement of vaccination regimens and improving the quality of the drugs used, rational limitation of the use of heterologous antitoxic serums, especially antitetanus, and their replacement where necessary. perhaps, on homologous gamma globulins, limiting the uncontrolled use of medications, carrying out sanitation of foci hron. infections, compliance with household hygiene rules that limit the entry of dust and other allergens into the body, improvement of technological processes in order to limit the effect of industrial allergens on the body. Particular attention should be paid to identifying children with secretory IgA deficiency and other immunodeficiency conditions that contribute to the development of S. (see Immunological deficiency), and corrective therapy.
Bibliography:
Ado A. D. Antigens as extreme irritants of the nervous system, M., 1952, bibliogr.; aka, General Allergology, M., 1978; Beklemishev N. D. Infectious allergy, Alma-Ata, 1968; Beklemishev N. D. and Sukhodoeva G. S. Allergy to microbes in the clinic and experiment, M., 1979, bibliogr.; Gushchin I.S. On the elements of the biological expediency of allergic reactivity, Pat. physiol. and experiment. ter., v. 4, p. 3, 1979, bibliogr.; Pytsky V. I. Corticosteroids and allergic processes, M., 1976; Coombs RR A. a. Gell R. G. N. Classification of allergic reactions responsible for clinical hypersensitivity and disease, in the book: Clin, aspects immunol., ed. by PGH Gellj ao, p. 761, Oxford ao, 1975.
Sensitization phenomena are observed in biology, medicine, psychology, chemistry and physics, as well as several other fields of science. However, the term means completely different things. What are we talking about?
Table of contents of the dissertation Kotov, Vladimir Sergeevich :: 2002 :: Moscow
Chapter 1. THE PROBLEM OF ALLERGIC LUNG DISEASES DUE TO FUNGAL SENSIBILIZATION IN CHILDREN (Literature Review).8.
Chapter 2. CHARACTERISTICS OF THE SICK CHILDREN OBSERVED AND RESEARCH METHODS USED.26.
Chapter 3. ALLERGIC BRONCHITIS IN CHILDREN WITH SENSITIZATION TO FUNGAL ALLERGENS.33.
Chapter 4. BRONCHIAL ASTHMA IN CHILDREN WITH THEIR SENSIBILIZATION TO FUNGAL ALLERGENS.51.
Chapter 5. EXOGENOUS ALLERGIC ALVEOLITIS IN CHILDREN WITH SENSITIZATION TO FUNGAL ALLERGENS.71.
Chapter 6. ALLERGIC BRONCHOPULMONARY ASPERGILLOSIS IN CHILDREN.93.
Chapter 7. DISCUSSION OF RESULTS AND CONCLUSION.116.