The health of the unborn child directly depends on the condition of the mother during pregnancy. Some diseases pose a real threat. One of these dangerous pathologies is asthma, which can worsen during pregnancy. Just a few years ago, doctors did not recommend giving birth to women with this disease. But medicine does not stand still, and today mothers with asthma give birth to healthy babies.
Asthma during pregnancy
Classification of the disease
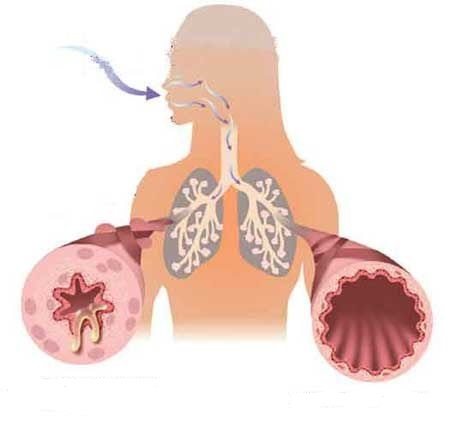
Asthma is a chronic respiratory disease. At the time of an attack, the lumens in the bronchi narrow, causing spasms and swelling of the mucous membranes of the larynx, which provokes suffocation. Cases of asthma diagnosis in pregnant women have recently become more frequent. This poses a threat as it has a direct effect on the fetus. An unborn child experiences oxygen starvation, which can provoke intrauterine hypoxia. Therefore, pregnant women with asthma should be constantly under medical supervision.
Pathology is classified based on etiology:
- endogenous;
- atopic;
- mixed;
- professional;
- aspirin
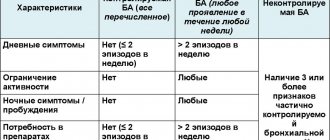
Diseases are also classified according to severity, where four stages are distinguished:
- Intermittent (episodic). Attacks are rare, often at night.
- Persistent (mild). Symptoms appear several times a week.
- Moderate weight. Frequent attacks that recur daily.
- Severe form. Daily attacks, most often occurring at night.
Women who want to give birth to a healthy child should independently monitor their condition. Professional treatment of bronchial asthma in pregnant women will help avoid severe symptoms and save the life of the unborn baby.
The course of asthma during pregnancy
Asthma behaves differently in different women during pregnancy. And it is very difficult to predict how it will progress for YOU. Especially if this is your first pregnancy. During pregnancy, asthma worsens in about one third of women, improves in one third, and remains stable in one third.
There are also a number of noted medical facts:
- Asthma worsens most often between 29 and 36 weeks of pregnancy. During this period, the symptoms of bronchial asthma may increase - suffocation, lack of air and cough;
- If asthma suddenly improves during pregnancy, toremission usually progresses gradually throughout pregnancy;
- The severity of asthma symptoms during the first pregnancy is often similar during subsequent pregnancies.
Manifestations
The disease often occurs in women of childbearing age, which increases the number of pregnant patients. The following can trigger an attack in asthmatics:

Allergens
- seafood;
- pollen;
- dust;
- household chemicals;
- cigarette smoke;
- animal fur.
Under the influence of these factors, a woman experiences shortness of breath, which turns into attacks of suffocation. Sometimes asthma appears after a traumatic brain injury or as a consequence of a disruption of the endocrine system.
Complications
In the absence of proper drug control, a pregnant woman with signs of bronchial asthma develops respiratory failure, arterial hypoxemia, and peripheral microcirculation is impaired. As a result, 37% of patients experience early toxicosis, 43% have gestosis, 26% have a threatened miscarriage, and 14.2% experience premature birth. The occurrence of hypoxia at a time when the formation of the child’s main organs and systems occurs leads to the formation of congenital developmental anomalies. According to research results, heart defects, developmental disorders of the gastrointestinal tract, spine, and nervous system are observed in almost 13% of children born by women with exacerbations and attacks of suffocation in the 1st trimester.
Immune complexes circulating in the blood damage the endothelium of the uteroplacental vessels, which leads to fetoplacental insufficiency in 29% of pregnancies with BA. Fetal growth retardation is found in 27% of patients, malnutrition - in 28%, hypoxia and asphyxia of newborns - in 33%. Every third child born to a woman with clinical symptoms of bronchial asthma is underweight. This figure is even higher in the steroid-dependent form of the disease. Constant interaction with the mother's antigens sensitizes the child to allergens. In the future, 45-58% of children have an increased risk of developing allergic diseases; they are more likely to suffer from acute respiratory viral infections, bronchitis, and pneumonia.
Diagnostics
The main method for diagnosing the disease is spirometry, which helps determine the amount of air exhaled. Diagnosis using the peak flowmetry method makes it possible to determine the exhalation rate. In addition, patients undergo standard laboratory and instrumental examination, which includes:
- blood test (general, biochemical);
- X-rays of light;
- allergy test;
- culture of sputum;
- computed tomography of the lungs (if necessary).
X-rays of light
Diagnosis and subsequent treatment occur under the supervision of a pulmonologist, allergist or therapist.
Features of treatment in pregnant women
Patients often complain that with the onset of pregnancy, asthma attacks become more frequent and more severe. Doctors explain this situation by a sharp change in hormonal levels and toxicosis.
Asthma during pregnancy leads to hypoxia, possible miscarriage or premature birth. There is a risk of defective development, congenital defects, and serious disorders of the nervous system. Lack of proper treatment poses a threat to the health and life of the mother and her unborn child.
Most medications are contraindicated in pregnant women. Therefore, it is most often recommended to use special inhalers (nebulizers), which asthmatics have long appreciated. Their help may be effective for asthmatic women during pregnancy and as a preventative measure.

Inhalation with a nebulizer
Inhalations give a local effect and affect only the bronchi and lungs, the concentration in the blood is minimal. Doctors do not recommend using inhalers containing freon.
A pregnant woman needs professional supervision. If before pregnancy she could control her condition herself, now this must be done together with a doctor. Any medications or vitamins that were not prescribed by a doctor must be excluded. Even if they were taken before pregnancy.
It is necessary that the expectant mother understands the severity of all complications that arise during pregnancy. If everything is done correctly, asthma attacks may not even bother you during the entire period of pregnancy. In order not to provoke a new attack, several recommendations from professional doctors will help:

Wet cleaning
- avoid stressful situations, control your emotional state;
- moisten the home daily and carry out wet cleaning;
- follow a diet, exclude seafood, exotic fruits, honey, coffee, eggs, chocolate from the diet;
- eliminate all bad habits;
- try not to have pets;
- stick to a daily routine, get more rest;
- use non-drug methods for treatment (climatotherapy, breathing exercises).
And then asthma will not be a contraindication for pregnancy.
Breathing exercises
There are several recommendations for performing breathing exercises for pregnant women. This helps not only relieve an attack, but also prevent its occurrence. Therefore, this practice must be used not only during an asthmatic attack, but also as a preventive method. A new attack causes panic. You need to learn to control this. Stress makes attacks worse.
Examples of exercises:

Breathing exercises
- If you cannot take a breath, you must continue to take deep exhalations.
- It is impossible to exhale and continue to inhale. Sit up straight, straighten your shoulders and breathe in as much air as possible.
- Take a deep breath, bend forward and exhale sharply.
- All exercises are performed while sitting, or even on the floor.
Several of these exercises quickly relieve spasms in the bronchi and reduce the risk of a possible attack.
What drugs are allowed
During pregnancy, a woman breathes and eats for two. Everything she takes will definitely go to the child. And if it is not possible to refuse the drugs, doctors prescribe them with extreme caution. Usually prescribed:
Beclomethasone
- Pulmicort;
- Beclomethasone;
- Theophylline;
- Salmeterol;
- Teopek;
- glucocorticoid agents.
Some components quickly pass through the placenta to the fetus and can provoke tachycardia.
Traditional medicine
Traditional medicine has many remedies in its arsenal that help in the fight against asthmatic attacks. Most often these are herbs that are used in the form of decoctions for inhalation. This is where nebulizers come in handy. There is no need to pour hot solutions into them, which eliminates the risk of possible burns. To prepare decoctions, herbs are used that help relieve swelling and spasms. This:
- yarrow;
- St. John's wort;
- chamomile;
- plantain;
- mint.
It is not advisable to use decoctions internally. Especially if the doctor did not advise it. Some can increase the tone of the uterus, lead to its prolapse and provoke involuntary abortion. This is especially dangerous in the first trimester of pregnancy.

Yarrow decoction
Causes
The occurrence of the disease in a pregnant woman is provoked by the same factors as in non-pregnant patients. Atopy, a hereditary predisposition to allergic diseases due to hypersensitization of the body with increased synthesis of immunoglobulin (IgE), plays a significant role in the development of bronchial asthma. The triggering point of bronchospastic conditions in these cases is the action of external triggers - household allergens (dust, paint vapors, building materials), plant pollen, animal hair, food products, pharmaceuticals, tobacco smoke, occupational hazards, etc. The appearance of symptoms in predisposed pregnant women can be provoked by respiratory viral infections, chlamydia, mycobacterium tuberculosis, intestinal and other parasites.
The topic of the influence of changes during gestation on the occurrence and course of asthma is still considered insufficiently studied. According to various authors in the field of obstetrics, in some cases the onset of the disease is associated with pregnancy, and its symptoms may persist or completely disappear after childbirth. A number of neuroendocrine, immune and mechanical factors have been identified that contribute to the development of bronchospasm during gestation. They also cause exacerbation of the disease and aggravation of its symptoms in pregnant women with bronchial asthma:
- Increased secretion of endogenous bronchoconstrictors
. The maternal part of the placenta and uterine tissue synthesize prostaglandin F2α, which stimulates smooth muscle contraction. Its concentration increases towards the end of gestation, ensuring the timely onset of labor. The substance also provokes respiratory obstruction due to spasm of bronchial smooth muscle fibers. - Increased concentration of immunoglobulin
E. A high level of IgE is an important link in the pathogenesis of atopic reaction to the action of sensitizing factors. Immune restructuring in response to constant exposure to fetal antigens leads to an increase in the content of this immunoglobulin in the blood of a pregnant woman and increases the likelihood of developing bronchospasm and asthma. - Increase in the number of α-adrenergic receptors
. Hormonal changes that occur towards the end of pregnancy are aimed at ensuring adequate labor activity. Stimulation of α-adrenergic receptors is accompanied by increased contractile activity of the myometrium. The number of such receptors also increases in the bronchi, which facilitates and accelerates the occurrence of bronchospasm. - Reduced sensitivity to cortisol
. Glucocorticoids have a complex anti-asthmatic effect, affecting different parts of the pathogenesis of the disease. During pregnancy, due to competition with other hormones, pulmonary receptors become less sensitive to cortisol. As a result, the likelihood of bronchospasm increases. - Changes in breathing mechanics
. The stimulating effect of progesterone contributes to the occurrence of hyperventilation and an increase in the partial pressure of carbon dioxide in the first trimester. The pressure of the growing uterus in the II-III trimesters and increased resistance of the vessels of the pulmonary circulation potentiate the appearance of shortness of breath. In such conditions, bronchospasm develops more easily.
An additional factor that increases the likelihood of asthma during gestation is progesterone-induced swelling of the mucous membranes, including those lining the respiratory tract. In addition, due to the relaxation of the smooth muscles of the esophagogastric sphincter in pregnant women, gastroesophageal reflux is more likely to form, which serves as a trigger for the development of bronchospasm. An exacerbation of the disease in a patient with manifestations of bronchial asthma can also occur if maintenance treatment with glucocorticoid drugs is refused for fear of harming the child.
Preventive measures
During pregnancy, a woman should control her lifestyle, avoid stress, eat well and rest. As preventive measures for asthma, doctors recommend:

Rinse the nose with saline solution
- Rinse your nose regularly with saline solution;
- use eye drops for conjunctivitis before walking during active flowering;
- avoid places where there are smokers (passive smoking);
- maintain optimal air humidity in the bedroom;
- limit or completely eliminate contact with allergens.
These simple rules will help you avoid new attacks.
Prognosis and prevention
Adequate treatment of bronchial asthma during pregnancy can completely eliminate the danger to the fetus and minimize threats to the mother. Perinatal prognosis with controlled treatment does not differ from the prognosis for children born by healthy women. For preventive purposes, patients at risk who are prone to allergic reactions or suffering from atopic diseases are recommended to quit smoking and limit contact with household, industrial, food, plant, and animal exoallergens. To reduce the frequency of exacerbations, pregnant women with asthma are advised to take exercise therapy, therapeutic massage, special sets of breathing exercises, and speleotherapy.
source