The persistent form of bronchial asthma is a rather serious disease that haunts the patient for a very long time. For years, the patient exhibits symptoms of the disease: a constant cough, difficulty breathing and heaviness in the chest. Such symptoms limit a person’s life activity, but sometimes there are periods when the disease recedes, there are no signs, and complete relief occurs.
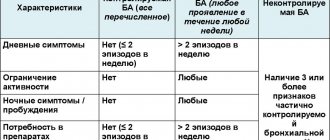
Degrees of development of persistent asthma
- The first degree includes a mild form of intermittent asthma. It is accompanied by shortness of breath, hoarseness and cough. These symptoms appear once a week. At night, an attack occurs no more than 4 times a quarter. The interictal period is characterized by the absence of symptoms. Indicators of the pulmonary system are normal.

- In the second degree of bronchial asthma with a persistent course, symptoms of the disease may appear 2 times within a month. At night, attacks almost never occur. At this stage of asthma development, the patient’s natural activity is disrupted. There is a gradual increase in pulmonary insufficiency.
- The third degree of the disease includes moderate asthma. Symptoms of the disease appear almost daily, accompanied by severe attacks. During this period of time, the patient is forced to take short-acting beta g-adrenergic agonists daily. Seizures disrupt the patient’s usual lifestyle, disrupting nighttime sleep and impeding recovery.
- The fourth place is occupied by the most complicated form of bronchial asthma. At this stage, there is constant pain, repeated attacks of suffocation and a painful non-productive cough. The patient suffers from insomnia, and therefore the biological rhythm of life is disrupted. This form of the disease requires mandatory hospitalization with further treatment in a hospital setting.
It should be noted that the severity of asthmatic disease can be determined based on symptoms before the start of the first treatment procedures. Otherwise, it is necessary to take into account the intensity of the therapy.
Prevention
In order to prevent bronchial asthma, you must follow several important recommendations.
Allergy sufferers are not recommended to keep pets, since their fur is one of the main allergens that provoke the development and exacerbation of persistent bronchial asthma. Quitting smoking, both active and passive, is also considered necessary.
It is very useful to regularly take walks in the fresh air, away from noisy roads and hazardous industries. Performing breathing exercises helps improve the functioning of the bronchi and lungs, as well as prevent the onset of a suffocating attack.
Persistent bronchial asthma is one of the most severe diseases of the respiratory system, which is accompanied by attacks of suffocation, severe coughing, and sleep disturbances. Treatment of mild to moderate illness can be carried out at home.
The pathology, which occurs in a severe form, is treated only in a hospital setting, as it poses a serious danger to the patient’s life.
source
Clinical manifestations
Persistent bronchial asthma, as a rule, has an episodic course and is characterized by short-term attacks, as well as their absence in the interval between exacerbations.
Asthma is characterized by an increasing exacerbation of symptoms and a decrease in the activity of bronchodilators used. Severe bronchial asthma can sometimes lead to hypoxia.
Unstable development of the disease is observed in patients with typical treatment measures. However, even among such patients, an inadequate course of bronchial asthma is possible, accompanied by the development of acute attacks with possible complications. An example of this is aspirin-induced asthma, which develops in response to NSAIDs.
Bronchial asthma becomes chronic in cases where the disease cannot be controlled with inhalation and there is an urgent need for the use of systemic steroid drugs.
Treatment methods
Pharmacotherapy for persistent asthma is divided into 2 types:
- continuous maintenance therapy;
- drugs used for exacerbation.
Maintenance (basic) therapy is aimed at reducing the frequency of attacks, up to their complete absence. For this purpose, drugs with anti-inflammatory activity (inhaled and systemic corticosteroids), long-acting beta-2 agonists are prescribed.

Salbutamol
In case of exacerbation, drugs with the fastest possible development time of effects are used: Salbutamol, Fenoterol.
Symptoms of the disease
The presence of bronchial symptoms in mild or moderate disease may be associated with a number of provoking factors, which may include physical activity and direct contact with the allergen.
Most often, bronchial asthma is accompanied by the following manifestations:
- bubbling in the chest area and wheezing;
- painful cough with minimal sputum;
- impossibility of normal respiratory function;
- the presence of compression in the chest area.

As symptoms increase, the course of the disease becomes more complicated and requires emergency medical measures.
Causes of persistent asthma
The risk of persistent asthma is due to the following reasons:
- genetic predisposition;
- excess of immunoglobulin bodies in the body;
- smoking of any form;
- ARVI;
- activities related to hazardous industries;
- excess body weight.

Persistent asthma can develop as a result of many factors. Of no small importance is the level of hormones in the body and the presence of chronic infectious foci. Therefore, timely treatment of concomitant diseases is necessary to avoid exacerbations of bronchial asthma.
Etiology and pathogenesis
According to GINA-2011, bronchial asthma (BA) is a chronic inflammatory disease of the airways, which involves a number of cells and inflammatory mediators, which leads to characteristic pathophysiological changes.
4. Narrowing of the airways is a universal final stage in the pathogenesis of asthma, which leads to the onset of symptoms of the disease and typical physiological changes.
Factors that cause narrowing of the airways:
Features of the pathogenesis are described for the following forms of asthma: - exacerbation of asthma; — night asthma; - irreversible bronchial obstruction; — BA, difficult to treat; — asthma in smokers; - aspirin triad.
Features of the course of the disease in childhood
As a rule, atopic bronchial asthma develops in children under 10 years of age. In children under 5 years of age, diagnosis is performed using bronchography.
The most likely causes of the disease in children are:
- genetic inheritance, especially on the mother’s side;
- allergic reaction to medications, food;
- the child has a history of diathesis;

- mild manifestation of obstructive syndrome during ARVI, since in children respiratory viral infections can most often provoke bronchial asthma with unproductive paroxysmal cough;
- In children, asthmatic syndrome can often occur during physical activity (physical exertion asthma), so the appearance of severe shortness of breath after exercise should alert parents.
Regardless of the severity of the disease, patients may experience complications ranging from mild to life-threatening. At the initial stage of the disease, they may be asymptomatic. This development of bronchial asthma in young children is most dangerous.
It is important to note that in most children, by the time of puberty, bronchial symptoms may disappear. However, in 205 cases of children suffering from persistent asthma at an early age, relapses are possible in adulthood. Children suffering from “aspirin asthma” have much less chance of recovery.
It is important to note that in most children, by the time of puberty, bronchial symptoms may disappear. However, in 205 cases of children suffering from persistent asthma at an early age, relapses are possible in adulthood. Children suffering from “aspirin asthma” have much less chance of recovery.
It is important to note that in most children, by the time of puberty, bronchial symptoms may disappear. However, in 205 cases of children suffering from persistent asthma at an early age, relapses are possible in adulthood. Children suffering from “aspirin asthma” have much less chance of recovery.
Carrying out diagnostics
With the severity of bronchial asthma, a detailed medical history is obtained from the patient for the presence of symptoms such as wheezing and noisy breathing, night cough, etc.
Visual diagnosis with short-term improvements does not reveal symptoms characteristic of asthma. Auscultation during the development of an attack determines the duration of exhalation and wheezing. In a severe asthma attack, cyanosis and involvement of additional pectoral muscles in respiratory activity are observed. Asthmatic disease must be distinguished from heart failure, which is characterized by a heart murmur.
The main diagnostic method for determining the disease is spirometry, which reveals respiratory functionality. In addition, in the absence of obvious symptoms, it is recommended to challenge with histamine, as well as check the response during physical activity.
Therapeutic measures
All types of asthmatic diseases, including atopic asthma, require five-step therapy:
- 1 - short-term attacks of the disease require the use of a leukotriene modifier;
- 2 – in mild persistent form, it is recommended to add inhaled corticosteroid therapy;
- 3 – moderate persistent stage of the disease requires additional administration of long-acting agonists;
- Stages 4 and 5 of severe bronchial asthma require oral use of corticosteroids.

In the case when the course of bronchial asthma is treatable, all measures return to the previous level.
Classification according to general rules
All diseases known to modern medicine are divided according to a special international classification; they are distributed according to the ICD. This is a single classification accepted throughout the world. All diseases without exception can be classified, but not bronchial asthma. The reason is that it tends to be accompanied by a variety of pathological processes. Asthma is classified according to other important factors, according to certain physiological manifestations:
- The severity of the manifestation of pathology at the very beginning of treatment;
- Signs of pathology that a person suffers from when starting therapy;
- Main phases of the course;
- The presence or absence of complications.
Based on this classification, the attending physician has the opportunity to determine the general condition of the patient. This is necessary in order to prescribe the most effective drug therapy.
Medications
Inhaled corticosteroids are most often prescribed to treat asthma. These include Tafen Novolizer, Flixotide, Bekotide, Klenil, etc. The inhaler relieves symptoms depending on the severity of the disease, improving the functioning of the pulmonary system, eliminating bronchospasms. In addition, inhalers help prevent the development of an attack during physical activity, improving the patient’s overall well-being.
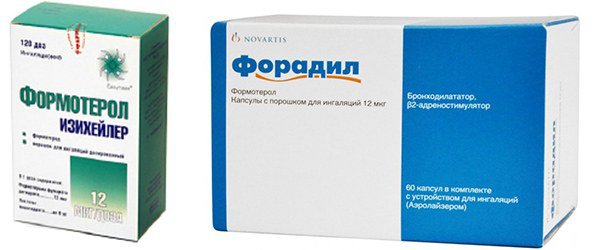
Antidepressants include antileukotrienes (Zafirlukast, Montelukast). These drugs allow you to reduce inhaled doses of glucocorticosteroids, which allows you to avoid side effects. In addition, it is possible to reduce the frequency of doses and dosage with the help of Formoterol, Foradil, etc.
For moderate severity of the disease, theophylline, which has a slow release, can be prescribed. It is used 4 hours after the use of corticosteroids, which had the desired effect in monotherapy.
Cromones (corticosteroids) are rarely used in self-treatment. They can cause a number of side effects. In especially severe cases, recombinant antigens (Xolair, Omalizumar, etc.) are sometimes prescribed. The pharmacological effect of these drugs has not been sufficiently studied, however, numerous studies indicate a decrease in bronchial symptoms with their use.
It must be remembered that any therapeutic measures can only be prescribed by a highly qualified specialist on an individual basis. Treatment tactics are chosen especially carefully for children.
Possible negative consequences
Asthma, including atopic asthma, worsens breathing and increases the load on the bronchial system.
- The result of a long-term disease can be emphysema, chronic development of bronchitis and an increase in connective tissue;
- in addition, the resulting congestive processes in the pulmonary system can worsen the functioning of the cardiovascular system, and the infectious route of development of bronchial asthma increases the risk of developing serious complications;
- a prolonged attack can manifest itself as pneumothorax, as well as air entering the pulmonary area during its rupture, which requires immediate hospitalization of the patient;
- Improperly performed treatment provokes severe asthma and the occurrence of status asthmaticus. It occurs with maximum narrowing of the bronchial region and the appearance of mucus plugs that interfere with normal air exchange.
It must be taken into account that emergency hospitalization is required when some symptoms of moderate severity develop, which are expressed by the following manifestations:
increased heart rate (more than 100 beats per minute);
- arrhythmias;
- the appearance of a respiratory rate of 25 beats per minute;
- the occurrence of an expiratory form of shortness of breath;
- noisy breathing and wheezing.
In addition, any deterioration in the patient’s condition with uncharacteristic symptoms also requires urgent medical intervention.
Classification by symptoms
Signs of bronchial asthma
It is quite difficult to miss the onset of the disease, since development occurs in certain stages. Based on them, experienced doctors classify the disease and develop a treatment regimen. The pathology has the following stages of development:
- Harbingers. A similar condition can be observed several days before the main attack. Usually such unpleasant phenomena as vasomotor rhinitis, difficult sputum discharge, dryness in the nasal cavity and periodic shortness of breath are observed.
- The height of the disease. As soon as the attack flares up, the person begins to experience a severe lack of air. At this time, the patient is forced to take a special position, for example, it becomes easier for him to sit on a chair with his hands resting on his knees. In this position, breathing becomes more difficult, as additional muscles begin to work. Inhalation is carried out with retraction of the intercostal spaces, and exhalation becomes longer and is performed with some effort. If the condition is serious enough, the patient may experience such an unpleasant phenomenon as hypoxia.
- Reverse development of the disease. This stage is accompanied by a gradual decrease in the severity of wheezing and shortness of breath. Gradually breathing is completely restored.
- Formation of status asthmaticus. This is a fairly severe attack, which is characterized by a more long-term and severe development of the disease. As symptoms worsen, the person becomes more acutely deprived of oxygen.
The last stage of the development of the disease is quite dangerous. If no treatment measures are taken, there is a risk of death.
Preventive actions
Preventive measures to prevent persistent bronchial asthma include the following:
- first of all, it is necessary to eliminate contact with the allergen that provoked the attack;
- it is necessary to carefully choose a profession - while limiting the negative impact of external factors;
- it is important to carry out all necessary vaccinations in accordance with the vaccination calendar;
- it is necessary to follow a special diet, avoiding fatty, salty, sweet and high-calorie foods.
It is important to note that regular and timely treatment, depending on the severity of the inflammatory process, can prevent serious complications and lead to a rapid recovery.
general information
Short description
Bronchial hyperreactivity is an increased sensitivity of the lower respiratory tract to various irritating stimuli, which are usually contained in the inhaled air. These stimuli are indifferent to healthy people. Clinically, bronchial hyperreactivity most often manifests itself as episodes of wheezing, difficult breathing in response to an irritating stimulus in individuals with a hereditary predisposition. There is also a hidden hyperreactivity of the bronchi, which is detected only by provocative functional tests with histamine and methacholine. Bronchial hyperreactivity can be specific and nonspecific.
Specific hyperreactivity occurs in response to exposure to certain allergens, mainly contained in the air (plant pollen, house dust, fur and epidermis of domestic animals, down and feathers of poultry, spores and other elements of fungi).
Nonspecific hyperreactivity is formed under the influence of various stimuli of non-allergenic origin (air pollutants, industrial gases and dust, endocrine disorders, physical activity, neuropsychic factors, respiratory infections, etc.).
Note. Excluded from this subcategory:
— Asthmatic status — J46; - Other chronic obstructive pulmonary disease - J44; — Lung diseases caused by external agents — J60-J70; - Pulmonary eosinophilia, not elsewhere classified - J82.
* Definition according to GINA (Global Initiative for Asthma) - 2011 revision.
— Professional medical reference books. Standards of treatment
— Communication with patients: questions, feedback, making an appointment
Download the application for ANDROID