Allergy shots are commonly called immunotherapy. They are made so that the human body can better fight infections and bacteria that cause an allergic reaction. Indicated for people who experience severe allergic reactions, and this happens for at least three months a year. Allergy vaccinations as such do not completely protect against it; they only strengthen a person’s immune system, helping the body cope with allergens.

How is it administered?
The medicine is administered by subcutaneous injection, as well as by instilling a solution into the nasal passage or mouth. The most reliable method is injections, because this way the patient will definitely receive all the necessary dosage of the drug.
At the beginning of therapy, the most minimal doses of the drug are used, which are subsequently increased. The highest concentration of allergens of the administered product occurs during the last injection. A maintenance dose of the drug is administered at regular intervals. It is worth noting that the maintenance course is quite long and ranges from three to five years.
Many people are interested in whether it is possible to get an allergy vaccine.

Allergen-specific immunotherapy and prevention of expansion of the list of allergens
ASIT is a method of antiallergic therapy and consists of introducing increasing dosages of an allergen to which increased sensitivity is established. Only such immunotherapy acts on any significant links in allergic processes and has a long-lasting preventive effect after completion of the treatment course.
The purpose of this technique is to reduce sensitivity to causative significant allergens, which is manifested in a decrease or absolute absence of clinical symptoms during natural exposure to pathogenic pathogens. The clinical effectiveness of this method is confirmed by controlled trials using placebo. In the course of such studies, the obvious advantages of specific immunotherapy over other treatment methods are determined:
- Long-term remission is maintained after completion of a successful ASIT course.
- The expansion of the range of allergens to which hypersensitivity is established is prevented.
- The aggravation of the disease is prevented. It also becomes impossible to transform a milder clinical manifestation of allergy (for example, rhinitis) into a more severe one (bronchial asthma).
- Reduced need for the use of antiallergic drugs.
Next, we will find out how often you will have to visit a doctor and what is the dosage of the injectable drug if you undergo a course of vaccinations against a particular allergic reaction.

Treatment process. How many times will you have to come to the Clinic?
1. It all starts with a visit to an allergist-immunologist. Be sure to take all available medical documentation with you: we need to fully understand your health picture. The doctor will examine you and, if necessary, conduct or repeat tests for sensitivity to various allergens.
2. Based on the results of the examination or examination + examination, the doctor will draw up a treatment plan. The treatment plan may include not only ASIT, but also other measures to restore normal immune function. This could be the treatment of concomitant infections, immunodeficiency, dysbiosis: we need to increase the chances of success of antiallergic vaccination.
3. Allergen-specific immunotherapy. You will take allergen medications yourself under the tongue. Typically this process lasts from several months to a year. Repeated treatment cycles are possible. As we get used to it, we will increase the dose of the allergen. The first doses of the ASIT drug and its new doses are under the supervision of a doctor in the clinic (in case of an excessive response to the allergen, we will immediately provide assistance), then at home. In total, there may be 5-7 such control visits to the clinic. More - only in very rare cases.
4. In case of any undesirable reactions or difficulties during administration, an unscheduled examination by your attending physician. This rarely happens.
How to prepare for vaccinations?
It is forbidden to engage in physical activity for two hours before an allergy shot, as well as for the same amount of time after it, and in general it is necessary to limit physical activity. When engaged in physical activity, blood rushes to the tissues, and antigens, in turn, are very quickly released into the bloodstream.
Vaccinations are generally incompatible with certain medications, for example they should not be combined with beta blockers. These drugs, when combined with allergy shots, may increase the risk of side effects. Therefore, immediately before undergoing such a course of therapy, you should tell your doctor about all the medications that the person is taking. You need to pay no less attention to the course of vaccinations if you are pregnant or if a woman is planning to conceive.
Recommendations for patients with hay fever
Every year during the flowering period, if possible, leave the area; reduce your stay in places where there are a lot of flowering plants (in a field, in a country house, in the foothills, etc.); wear long sleeves; when you come home, take a shower and change clothes; in clear sunny weather, especially in the morning, wear glasses; Indoors need to be wet cleaned more often; It is better to ventilate the premises in the evening; special nets should be placed over windows, vents, and transoms; if possible, during the flowering period do not take medications other than those prescribed by an allergist; Do not plan surgical interventions during the flowering period (except in emergency situations).
What to expect after vaccinations?
Thirty minutes after vaccination, you must undergo an examination by a doctor in order to identify possible adverse reactions such as runny nose, sore throat, itching and general malaise. Such symptoms may also occur after the patient leaves the doctor. If this happens, you need to return to the medical facility where the vaccination was performed.
The occurrence of local irritation at the injection site, along with swelling and redness, is considered normal if these symptoms subside within a maximum of eight hours after the injection.
Is there a flower allergy vaccine?

Allergen-specific immunotherapy (ASIT) allows you to reduce a person’s sensitivity to a specific allergen, and thus reduces the severity of external manifestations, and also reduces the risk of “severification” of allergies - the development of bronchial asthma.
Its essence lies in the subcutaneous injection of increasing doses of a causally significant allergen. ASIT is carried out before the beginning of the flowering season. This treatment is recommended for three to five years.
What types of allergies does ASIT help with?
We use high-quality drugs for allergen-specific therapy produced by SEVAFARMA, Czech Republic (SEVAPHARMA, www.sevapharma.cz). This is not the cheapest option for ASIT, but in this case we recommend paying a little extra for quality, safety and the ability to take it independently and sublingually, rather than through injections and in the clinic.
Indications for ASIT
- Hay fever. Allergy to pollen from flowering trees, shrubs, and grasses.
- Allergy to household allergens (house dust mites, molds);
- Allergic rhinitis, conjunctivitis, bronchial asthma, atopic dermatitis, allergens caused by the listed household and pollen and cross allergens.
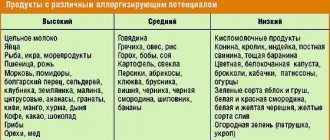
Cross allergy options
Vaccination effectiveness
Immunotherapy is quite effective in combating allergies to insect stings. But to date, there is no data on how effective this method is if a person has food allergies.
What is important to know about vaccinations for egg allergies?
If a baby is intolerant to chicken protein, then all vaccines that are made on the basis of a chicken embryo are contraindicated for such a patient.
You should call your doctor if symptoms develop after vaccination that are caused by side effects of the medication.
Diet
Hypoallergenic diet for allergies to tree pollen - in the period from April (mid-March) to May (mid-June) exclude (or greatly limit): stone fruits (cherries, cherries, peaches, apricots, plums, black olives), pome fruits ( apples, pears, kiwi), honey and bee products, nuts (walnuts, pistachios, peanuts, almonds, especially hazelnuts) and products containing them, raw carrots, potatoes, raw tomatoes, cucumbers, parsley, dill, celery, spices (curry, anise, cumin and others), birch sap, cognac. The use of herbal remedies is strictly prohibited: birch buds, birch leaves, alder cones, buckthorn bark, oak, ramnil.
Hypoallergenic diet for allergies to pollen of cereal (meadow) grasses - in the period from June (mid-May) to July (mid-August) exclude (or greatly limit): bread kvass, beer, wheat vodka, schnitzels, puddings, dumplings, pancakes, cutlets , gravies, sauces (contain flour), bread, bakery products and cereal products (oats, wheat, rye, barley, rice), rolled oats, bran, oatmeal cookies, cereal porridges, pasta, peanuts, all types of smoked sausages, coffee , cocoa, ice cream, sherbet, sesame, sorghum, honey and bee products, strawberries, wild strawberries, citrus fruits, legumes, soybeans, corn, sorrel. It is not recommended to take B vitamins, herbal teas, herbal remedies containing cereal herbs and the use of cosmetics containing herbal ingredients.
Hypoallergenic diet for allergies to pollen-bearing herbs - in the period from mid-July to September, exclude (or severely limit): sunflower seeds and sunflower oil, halva, mustard mayonnaise, honey and bee products, drinks prepared using wormwood (vermouths, balms, absinthe , tarragon and others), carrots, garlic, celery, parsley, dill, spices (cumin, pepper, anise, coriander, curry, chicory, nutmeg, cinnamon and others), ginger, watermelon, melons, zucchini, eggplant, tomatoes, tobacco, potatoes, carrots, cabbage, beets, turnips, spinach, lettuce, Jerusalem artichoke, rutabaga, bananas, kiwi, citrus fruits, Corvalol, Valocordin. The use of herbal remedies is strictly prohibited: those based on wormwood, chamomile, calendula, coltsfoot, string, elecampane, yarrow, tansy, plantain, dandelion, St. John's wort, immortelle.
Vaccination schedule for children
You can get an allergy vaccination in all medical institutions in the country that have an allergy department.
The vaccination schedule must be individualized. The child is vaccinated only against the background of absolute health with additional insurance protection with antiallergic medications. As a rule, antihistamines are prescribed three days before the vaccination and for twelve days after it.

If a child gets sick with something, you need to be very careful in choosing medications for him. It is not recommended to use popular and well-known remedies in the form of honey, mustard plasters, propolis, mumiyo, collecting pollen, rubbing with turpentine and other irritating liquids. Penicillin is not recommended for antibiotics.
Allergy treatment with vaccinations is becoming more popular every day.
Provided that the listed preventive procedures are consistently followed, the clinical symptoms of an allergic disease can be prevented and, at the same time, significantly weakened or postponed to a later age. In addition, the prevention of food allergies is also a way to prevent other forms of reactions. In some patients, this may also serve as a preventive measure against excessive respiratory morbidity.

What do experts think about allergy shots? More on this later.
COVID-19 vaccine will not be offered to people with allergies
Over the past 24 hours, 4,892 new cases of coronavirus have been identified in Russia – this is another recent minimum; 3,133 people have recovered. The second stage of clinical trials of the vaccine started today in Novosibirsk - volunteers from 18 to 60 years old are participating in it. Well, the world’s first registered Russian vaccine against COVID-19, the Gamaleya Center, has already rolled off the assembly line - 15 and a half thousand doses have been produced. As Rospotrebnadzor emphasized, the country needs to have several vaccine options.
Before getting the coveted vaccination, their heart is listened to, their lungs are scanned, their blood pressure and temperature are measured every day. For the purity of the experiment, the new vaccine is tested on young and healthy people.
“Exclude any pathology that is not visible to the eye, which the patient may not even know,” explains the specialist.
Scientific launches the second stage of clinical trials. That's another 86 volunteers who will be given the vaccine candidate. The first group of 14 people has already received their dose of protection.
“All volunteers feel good. Those who have already received the vaccine do not have any side effects, there are not even the slightest redness at the injection site,” says Anna Popova, head of Rospotrebnadzor, chief state sanitary doctor of the Russian Federation.
Novosibirsk is creating several vaccines on different platforms. Among these options is protein, when viral peptides are injected directly into the human body. And synthetic - there is no live virus in it.
“Initially, six different vaccine prototypes were developed, built on independent vaccine platforms. At the first stage, only three of them were selected. At the moment, the best option is the Epivac-Corona peptide vaccine, which has entered the stage of clinical trials on volunteers,” explained Rinat Maksyutov, General Director of the State Scientific Center for Virology and Biotechnology “Vector” of Rospotrebnadzor.
It took three weeks to develop the vaccine design, that is, the theoretical basis. On one platform alone, Vector scientists created 15 combinations. And safety and effectiveness were already tested on model animals.
“From the entire range of studies, we selected the most critical ones. If there were serious disturbances in the functioning of the immune system, the vaccine would not have been included in clinical trials,” said Elena Danilenko, director of the Institute of Medical Biotechnology, a branch of the State Research Center of Virology and Biotechnology “Vector” of Rospotrebnadzor.
To find the best option, different platforms were taken as a basis. Stop the rapid spread of infection and prevent a second wave. The time factor in developing the vaccine was extremely important.
The president spoke about this back in April, at the height of the pandemic.
“I understand well and am aware of what a complex, painstaking scientific search is being carried out in this direction. It’s difficult to make a guess here, it’s impossible. Not only must the vaccine be obtained, its effectiveness and safety must be proven. In this regard, I understand what a colossal responsibility for the result lies with the developers,” said Vladimir Putin.
The first vaccine registered in the world is Sputnik-V. It was developed by scientists from the Gamaleya Institute. Full information on the research results will be published this week.
“The approach we took makes it possible to specifically create the necessary antigenic product that causes us the desired immune response. We do not form antibodies to the entire virus, but to strictly specific structures that we create before the vaccine enters our body,” Alexander Gintsburg, Academician of the Russian Academy of Sciences, Director of the National Research Center for Epidemiology and Microbiology named after N.F., informed the public. Gamaleya.
Vaccine developers are still quite strictly limiting the range of its use. The injection can only be given to people aged 18 to 60 years. Vaccination will also be denied to those for whom any vaccination is contraindicated.
“These are people who have exacerbations of serious chronic diseases - these are oncological diseases, and unstable autoimmune diseases, these are any processes in the phase of active inflammation - be it allergic processes. Such people, of course, are not vaccinated,” said Irina Manina, an allergist-immunologist.
But there is much more evidence. The vaccine creates immunity. When a person encounters a live virus, he is already protected. The more people who are immune, the easier it is to stop the spread of the disease.
“Vaccination, we know, is a very powerful weapon against infectious diseases. And we are confident that the vaccine will be effective and will increase immunity,” said Tatyana Ruzhentsova, head of the clinical research department of the Central Research Institute of Epidemiology of Rospotrebnadzor.
The Pasteur Institute, where they are studying collective immunity to SARS Cov-2, came to the conclusion: at the moment, only every fifth Russian has antibodies to the coronavirus.
“If we reach a level where the immune layer reaches 60-70%, then we will have an increased incidence, but there will not be an epidemic. If the level of the immune layer reaches 90%, then there will not even be a high incidence. Until collective immunity is formed, we will not be able to sleep peacefully,” said Areg Totolyan, academician of the Russian Academy of Sciences, director of the St. Petersburg Research Institute of Epidemiology and Microbiology named after Pasteur.
Doctors and teachers will be the first to receive the coronavirus vaccine. Vaccination will begin in September this year. By this time, the second stage of clinical trials of another Russian vaccine is planned to be completed by scientists.
A double protective barrier that will be more difficult for the virus to overcome.
Reviews from allergy sufferers and specialists
Many patients complain that absolutely nothing helps them from an allergic reaction. Doctors, in turn, emphasize that people, after completing a course of vaccinations, often expect an immediate effect and result. But, as experts note, this simply does not happen, and everything takes time, along with the body developing appropriate protective reactions. Vaccination does not relieve a person from it, but encourages the body to respond more effectively to the pathogenic pathogen, due to which, in most situations, acute symptoms are noticeably reduced.

In reviews of allergy vaccinations, patients write that allergen-specific immunotherapy itself implies long-term treatment. Someone reports an improvement that occurs after just one year of treatment. But, as most patients say, they needed to undergo at least three, or even four courses, that is, they had to take injections for several years in order to ultimately get a lasting result. And some, judging by the reviews, have to visit a doctor for five years.
Doctors in their comments emphasize that if a person has an allergic reaction at least once, this already indicates that the patient has sensitization (that is, hypersensitivity) to a particular allergen. And this already means that an allergy that occurs once will not go away on its own. And when it will appear again is simply unknown. Thus, in such a situation, it is necessary to consult a doctor and undergo a course of appropriate vaccinations.
Cost of allergy treatment with ASIT, contacts, where to buy drugs
The cost of allergy treatment consists of the price of medications and our services.
Our services usually include 2 appointments with an allergist-immunologist and 5-7 control visits to the clinic per course of treatment. Some tests for infections, sensitivity to allergens, and an immunogram may be needed.
We recommend a drug that is suitable for treatment specifically in your case. You choose where to purchase the drug for allergen-specific immunotherapy. There are few pharmacies specializing in allergens. You can find out the cost of drugs and purchase them, for example, here:
- TD "Allergen" is a large supplier of immunobiological drugs, contacts here;
- Pharmacy “Balsam No. 158” (Partner of the Trade House “Allergen”), Moscow, Universitetsky Prospekt, 9, metro University , Tel.;
- Pharmacy point, st. Pogodinskaya 1/1, clinic of propaedeutics of internal diseases of the Moscow Medical Academy named after. THEM. Sechenova, m. Frunzenskaya, +7 (499) 248-71-81;
- Pharmacy point, New Zykovsky pr. 4A, Hematological Research Center of the Russian Academy of Medical Sciences, Dynamo metro station.
If you have difficulties purchasing medications, immediately contact your doctor, we will do everything to solve this problem.