Causes of reaction to cold
- Long-term chronic diseases: sinusitis, sinusitis, caries, tonsillitis;
- Disruptions in the endocrine system;
- Weakening of the immune system;
- The presence of helminths in the human body;
- Pathologies of the kidneys, diseases of the gastrointestinal tract, liver and other organs;
- Colds, stress and cancer;
- Hereditary predisposition;
- Infectious diseases: chickenpox, mumps and pneumonia;
- Allergy to dust, animal hair, pollen;
- Long-term use of antibiotics;
- Genetically programmed increased permeability of the skin and mucous membranes.
Getting rid of cold allergies on your own
Helpful Tips:
You can also read: Why does the skin on my face peel in winter?
- Half an hour before going outside, lubricate your hands and face with a nourishing cream that will help protect sensitive skin.
- Always wear protective lipstick. The best one is one that contains avocado oil or shea butter.
- Before leaving the house, as well as immediately after going outside, drink hot tea with lemon or cranberries.
- When going outside, try not to breathe too deeply so as not to injure your mucous membranes and lungs.
- Eat more nuts, fatty fish (salmon, salmon, mackerel), cheese, and dress salads with olive oil.
- Try to eat hypoallergenic food, since the occurrence of one type of allergy provokes the development of another.
- In summer, you can strengthen your body by hardening. Dousing yourself with cold water will help prepare your body for the cold.
- Before the start of winter, it is recommended to undergo a course of treatment with antihistamines to reduce the likelihood of allergic reactions.
- Avoid stress, as it weakens the body's defense reactions.
- Strengthen your immune system. Lead a healthy lifestyle, exercise and eat right.
Types of cold allergies
Allergy to cold is characterized by a variety of types and forms of manifestation.
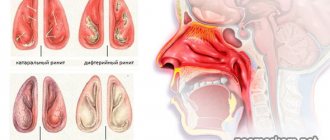
Cold dermatitis - the skin is very itchy and itchy. In severe cases of the disease, swelling of the entire body may occur.
Cold runny nose - accompanied by discharge of fluid from the nose, frequent sneezing, general weakness and headaches; nasal discharge is observed only in the cold, when a person enters a warm room, the runny nose stops;
Cold conjunctivitis – on frosty days the eyes can become very sore and watery;
Cold asthma is the most dangerous type of allergy, which is accompanied by attacks of suffocation and severe shortness of breath;
Cold erythema (urticaria) - characterized by severe redness of the skin and severe soreness in certain areas of the body.
Cold urticaria is divided into several types
Acute or chronic. With this type of allergy, severe irritation, rash and itching begins on the face and hands, and blisters appear. Certain areas of the body may turn red; in appearance it looks like insect bites. The rashes are often accompanied by lethargy, chills, and pain in the joints and muscles. Attacks of exacerbation can continue for several weeks and even months while it is cold outside.
Recurrent. It usually occurs at certain times of the year - autumn, winter and cold spring (most often it appears from early autumn to mid-spring). However, exacerbations can occur at different times of the year, depending on the air temperature. An exacerbation of an allergic reaction to cold water can begin at any season.
Reflex. It occurs exclusively when the entire body cools, but at the same time, rashes can appear only in one area of the body.
Hereditary . Passed on from generation to generation. The disease is expressed in the form of maculopapular rashes and burning. Sometimes allergies are accompanied by fever, chills, and joint pain.
Features of hereditary allergies: this is a genetically programmed gene mutation; occurs with slight hypothermia (draft, light wind); is not a lightning-fast response to an allergen; it can develop over several hours; inflammatory changes in laboratory parameters (leukocytes, CRP, ESR) are characteristic; occurs against the background of inflammatory diseases; negative ice challenge tests.
Safety regulations
To minimize the manifestations of cold urticaria, it is recommended:
- avoid hypothermia;
- take a warm shower, rinse your face with warm water;
- clothing should be made of cotton or soft wool, not synthetic!;
- in winter, be sure to wear a hat and scarf;
- exclude cold foods/drinks from the diet;
- exclude outdoor sports during the cold season;
- use protective creams and balms for the face, lips and hands (preferably from the pharmacy cosmetics segment);
- use antihistamines during exacerbation of urticaria according to the regimen prescribed by the attending physician.
Symptoms of cold allergy
Characteristic symptoms that can be observed on any areas of the skin that react to cold.
- Swelling, redness of the skin on the face and rashes on the hands;
- Dryness, peeling that occurs later;
- Burning and itching of the skin on the cheeks and forehead - as a reaction to the wind and hypothermia;
- Rash in the form of pimples and small blisters on closed areas - thighs, ankles or all over the body;
- Signs of respiratory diseases (sneezing, runny nose), which appear in the cold, but disappear in a warm room;
- Weakness and headaches;
- It is not uncommon for bruises to appear on the areas of the rash after 24-48 hours;
What may cause the reaction
- Freezing weather: Exposure to low air temperatures for several minutes or longer.
- Sweating: A reaction can occur even on a warm day. The breeze quickly cools damp skin, causing rashes.
- Visit to the swimming pool. You have to be especially careful when swimming. An accelerated heartbeat combined with an allergic reaction can cause a sharp drop in blood pressure.
- Cold solution for intravenous administration. Refrigerated IV solution may cause an allergic reaction and pain in the limb through which it is administered if the person is allergic to cold.
- Chilled foods and drinks: Consuming cold foods (ice cream, ice water) can cause the tongue and surrounding tissues to swell.
- Cool and cold surfaces: Contact with cold surfaces (if sitting on a cold stone) can result in the development of an allergic rash on the contact area.
- Cold indoor air: Walking into a heavily air-conditioned room on a summer day can lead to an allergic reaction to exposed skin, nasal congestion from breathing in cool air, and possibly a feeling of fatigue.
- Impaired blood flow: Activities that strain muscles and impair blood flow can cool the affected parts of the body, causing itching and rashes.
If you find yourself with one of the above symptoms, contact an allergist or dermatologist to clarify the diagnosis.
Don’t make a diagnosis yourself and don’t start the disease!
PRO HEALTH
03/20/2011 ALLERGY TO MELTS SNOW
Just a few years ago, the peak of allergic reactions occurred in the month of May. The flowering of the first plants and the opening of buds contributed to the seasonal exacerbation of allergies. However, over the past few years, the picture has changed dramatically; the growth curve of allergic reactions begins to creep up sharply in early March, when the drifts of uncollected snow on the streets of our city are just beginning to sag under the rays of the sun, and spring is timidly trying to come into its own.
Why do attacks of rhinitis and other manifestations associated with allergies attack us so early? Why do people who previously did not know what an allergic reaction is go into a coughing fit and are sincerely perplexed when their eyes begin to water and their throats feel sore?
As allergists note, there are several reasons for the early onset of the allergy period. The main one is reagents that are used in winter to treat sidewalks and roadways. If in past snowless winters they were covered and poured in smaller quantities, then in recent years their use has increased significantly. In addition, a small number of thaws contributes to the accumulation of reagents in the snow and their massive leaching during the melting process, the peak of which occurs precisely in the month of March. Snow on city streets, like a sponge, perfectly accumulates harmful substances produced by vehicles and industrial enterprises. The new phenomenon even has an unofficial name - “melting snow allergy”!
Now think about what chemical elements are contained in this snow mass in a preserved form? These are lead oxides, soot, heavy metal salts, etc. In a word, the entire periodic table in the process of melting is absorbed into the soil and spread by the wind throughout our city, i.e. enters the atmosphere and our lungs, provoking various types of allergic reactions.
The scale of the epidemic
In its scope, the allergy epidemic can already be compared to the flu epidemic. It threatens an equally large part of the population and has a pronounced seasonal nature. Approximately 20% of St. Petersburg residents suffer from allergic diseases to one degree or another, and among children this percentage reaches 30! Every year the situation only gets worse. Statistics eloquently demonstrate the trend in the spread of allergies and the steady increase in the number of people suffering from it.
Today, the list of external manifestations of allergies looks something like this: pain or burning in the eyes, tearing, sneezing, swelling, runny nose, wheezing, shortness of breath, hearing loss, various skin rashes, nausea and the same headache. The most dangerous form of allergy is known - anaphylactic shock. It can occur either a few seconds after the allergen enters the body or within a period of up to five hours. And then - loss of consciousness, sudden shortness of breath, convulsions, rash all over the body, vomiting - you need to urgently call an ambulance.
Has the snow melted? Get out of the park!
Of course, anaphylactic shock is an extreme. However, allergies are an insidious, unpleasant and, alas, difficult to treat disease. There are quite a few varieties of it (in particular, food, cold, household chemicals, melting snow, etc.).
In the spring, especially in March and early April, in addition to the danger contained in melting snow, it is necessary to pay attention to another invisible enemy - mold spores. Molds are especially dangerous: with the onset of warm weather, they begin to multiply and grow. But even at home, this particular allergen is the second most common after house dust mites!
The street version of the appearance of allergy symptoms is simple: you go out to a park or square to take a walk and breathe some air, and spores of mold fungi that live in damp soil, thawed last year’s leaves, grass and pine needles immediately begin to enter the respiratory tract. There is an even greater risk when working in the garden or vegetable garden in the spring. In addition to respiratory problems (runny nose, cough, sore throat, shortness of breath) and allergic conjunctivitis (“melting snow syndrome”), there may also be skin problems - atopic dermatitis (eczema). Therefore, such walks should be excluded.
By the way, if there is a reaction to rotten leaves and grass, then most likely there is a reaction to household mold (the risk zone in an apartment is the bathroom), and, possibly, to the soil in pots with indoor flowers. Therefore, these sources of mold must be excluded.
Insidious hay fever
Hay fever is caused by pollen from flowering plants, and urban residents suffer from it 6 times more often than rural residents. You should not believe rumors about the harmlessness of hay fever; they are greatly exaggerated. Indeed, as it progresses, already 2-4 years after the onset of the disease, the lower respiratory tract is affected, which leads to the development of pollen bronchial asthma.
However, not only the respiratory system, but also the nervous system suffers from hay fever: the patient develops irritability, fatigue, depression and migraine attacks are possible. In some cases, damage to the optic and auditory nerves and even damage to the blood vessels of the brain are observed; cases of pollen epilepsy are described. When pollen enters the gastrointestinal tract with food, some patients experience nausea, vomiting, diarrhea, and severe abdominal pain in combination with urticaria. Once pollen particles enter the bloodstream, they can also cause a rheumatic-type reaction in the joints.
Why are residents of cities, including St. Petersburg, mostly susceptible to hay fever? The fact is that due to an unfavorable environment (car exhaust gases - their quantity has increased significantly, emissions from enterprises, etc.) the mucous membranes of the nose and eyes are in a state of chronic inflammatory or degenerative process. Therefore, an active reaction to each new stimulus immediately appears. Moreover, there is no need to talk about any lifelong immunity to allergies: even the body of a mature person can reach a critical point and give in to the same pollen. Again, it is enough to react only once, and the next time you encounter a minimal amount of allergen, the symptoms will be obvious.
There is no doubt that such a meeting is very likely: pollen is carried by the wind over a distance of 300-400 kilometers. Therefore, if the same birch tree is not yet blooming in your St. Petersburg microdistrict, then its “relatives” can send greetings from the neighboring Novgorod or other southern region. In general, you can feel relatively calm only at an altitude of 5000 meters above sea level and in permafrost areas: pollen does not reach there...
Pollen until autumn...
As Olga Dzyuba, a St. Petersburg pollen specialist and candidate of geographical sciences, said, each climate zone has its own pollen allergens. In the North-West of Russia, these are mainly wind-pollinated tree and shrub plants (elm, hazel, alder, willow, birch), as well as meadow grasses (foxtail, bluegrass, timothy).
However, hay fever has three periods of activity: spring, summer and summer-autumn. The first lasts from mid-April to the end of May and is associated with the flowering of trees, primarily alder and birch. The proportion of patients during this period is about 10%. The summer period is the most dangerous, because it accounts for 70-80%. In time, this is from the beginning of June to the end of July, when meadow cereal grasses bloom: timothy, bluegrass, wheatgrass, and zoster. From the end of July to October, the time comes for asteraceae (wormwood) and goosefoot (quinoa), which threatens trouble for approximately 6% of allergy sufferers - these are victims of the summer-autumn period. In addition, allergists highlight the October outbreak of hay fever: active leaf fall, especially in dry, warm weather, releases pollen contained in the leaves.
How to protect yourself from hay fever? Potential victims during the flowering period of “their” plants (this is determined using an allergy test) should, if possible, protect themselves from contact with pollen. After all, the more often the contacts and the higher the concentration of the allergen, the more severe the disease.
It is clear that during this period you need to stay away from fields and forests and not bring flowers into the house. When you come from the street, you should immediately change clothes and wash your hair, because pollen may remain on your clothes and hair. It is especially intense in the early morning hours. Hence the advice - do not sleep with windows open at night.
When it rains, the concentration of pollen in the air is much lower than on a dry, sunny day. For allergy sufferers, the opposite is true: the better the weather, the worse it is for them. If the disease is traditionally very severe, then in the most unfavorable period it is best to take a vacation and go to the sea or to an area where coniferous forests predominate.
We take measures in advance
During an exacerbation, the doctor usually prescribes antihistamines to the allergy sufferer. It is important to change the medication periodically to prevent addiction from developing. If the medication is ineffective, the doctor may prescribe hormonal drugs according to an individual regimen, depending on the severity of the patient’s condition. Hyposensitization methods are also used in treatment: the patient is given an allergen in microdoses in advance in order to gradually accustom the body to the upcoming contact with it.
Unfortunately, treatment is usually long-term. In addition, over time, the disease can progress, the range of allergens expands: they are often joined by house dust, animal hair, or, for example, odors. The same low-quality cosmetics and deodorants irritate the mucous membrane and serve as a kind of gateway for the development of various forms of allergies. The most allergenic components of cosmetics are dyes, fragrances, and animal fats. Therefore, the best option is to buy it in pharmacies or specialized stores. In addition, you need to take into account the fact that a quality product, by definition, cannot be cheap. When purchasing a product that is new to you, you should conduct a test: apply a little product to the crook of your elbow or to the skin behind your earlobe and wait at least 12 hours (ideally, at least 36 hours should pass). If there are no consequences, these cosmetics or other perfume products can be purchased.
The basic concept of adequate treatment of allergies and asthma is based on an integrated approach, including a combination of drug therapy with osteopathic methods, reflexology, homeopathy, and sometimes psychotherapy. Only then can a positive effect be achieved.
At the first symptoms, you should not delay a visit to an allergist. In St. Petersburg, over ten allergy clinics for adults provide free assistance, and there are a number of paid clinics. Today in St. Petersburg a system of preclinical diagnostics has been developed, i.e. Doctors have the opportunity to predict the risk of developing the disease when there are no manifestations of allergies yet. The essence of the technique is simple: a person answers 12 questions in a questionnaire. After this, the answers are analyzed, and the forecast accuracy reaches 80%. If there is a predisposition to the disease, additional research is performed.
Another way is to work with newborns, which makes it possible to identify a risk group and carry out primary prevention of allergic diseases in children using non-medicinal means. With age, even recommendations on choosing a profession are possible: a potential allergy sufferer cannot be a pharmacist, hairdresser, or pastry chef. Caring for the quality of life of an allergic person should begin from the first years of life.
Prepared by Peter Berestov
We also thank Pyotr Vasilievich Ivchenkov for his help in preparing this material.
Title: Allergy to melting snow Number of hits: 1474 Author: Pyotr Berestov
Diagnosis of cold allergies
Diagnosis of an allergy to cold, like any other allergy test, must be carried out in a medical center, where there are all the means and capabilities to provide immediate assistance.
List of laboratory tests for diagnosis
- General blood analysis;
- General urine analysis;
- Blood chemistry;
- Identification of lymphocytes sensitive to cryoglobulin;
- Skin tests (to exclude concomitant allergies).
- Provocative test with an ice cube;
- TempTest.
What do these tests show?
General blood analysis. The results of a complete blood count will help detect an increased number of white blood cells, eosinophils and ESR (erythrocyte sedimentation rate). These changes indicate that an allergic process is occurring in the body. However, it is not correct to draw conclusions only on the basis of a blood test, since the same results are characteristic of helminthic infestation.
General urine analysis. An increased protein content in the urine indicates a possible inflammatory process of the urinary system, for example, glomerulonephritis, which develops as a complication of allergies.
Blood chemistry. This analysis will show increased amounts of circulating immune complexes, acute-phase inflammatory proteins, and an increase in total immunoglobulin E levels.
Such changes confirm an allergic reaction in the active phase, but do not provide accurate information about the allergen.
Identification of cryoglobulin-sensitive lymphocytes. If the test results are positive, this means that the cold is the cause of the allergy.
Skin tests. Skin tests are performed if there is doubt that the cold caused the allergic reaction. Quite often, lymphocytes sensitive to cryoglobulin cannot be detected in the blood.
And if there is no important evidence of the body’s reaction to cold, then doubts are understandable. Therefore, it is necessary to make sure that the allergy is triggered by cold and is not a cross-reaction to some other allergen.
Duncan test or ice cube test. Cold sensitivity testing is usually done by placing an ice cube on the skin for a few minutes. If the reaction to the cold is positive, the area where the skin comes into contact with the ice will become red, swollen, and may develop a rash.
TempTest Helps determine the body's overall sensitivity to low temperatures. TempTest differs from the ice cube test in that it can not only detect cold urticaria, but also determine what temperature range causes symptoms.
The patient places his hand on the device panel, equipped with thermal film, for 5 minutes. Thermal film continuously generates the entire range of specified temperatures. Using this procedure, the threshold temperatures for the formation of cold urticaria are determined.
How to get rid of allergies to cold?
Firstly, before starting treatment, a person should exclude the presence of those diseases that provoke the development of cold allergies.
Secondly, symptomatic treatment can be used. If you have skin rashes, use antihistamine ointments, which will speed up the healing of the skin and reduce swelling. If the main manifestations of the disease are lacrimation and runny nose, antihistamine drops will help.
Thirdly, before going outside, you need to cover your skin as much as possible: do not forget to wear a hat and hood, a voluminous scarf, mittens or gloves. Doctors recommend especially protecting your legs from frost, even though they are not exposed areas of the body. Wear warm tights and socks, and high boots. Clothing in contact with the body should not be made of wool or synthetics. It is better to choose linen or cotton items.
If the measures you take on your own do not help, you should consult a doctor who will select the necessary treatment based on your symptoms and your test data. You should contact either your primary care physician or an allergist directly.
Depending on the symptoms, doctors use medication
Signs of allergic cough in adults and its treatment
A cough can signal the development of various diseases. People often confuse a cough of an allergic nature with a manifestation of an acute respiratory disease (pharyngitis, laryngitis, bronchitis) and begin to treat it with cold medications or antibiotics.
Such therapy will not only be ineffective, but can also seriously aggravate the situation. Therefore, it is important to be able to recognize the symptoms of an allergic cough and also know how to deal with them. In this article we will look at this topic in detail and answer all the important questions.
Causes of allergic cough development
An allergy cough occurs in response to an element (substance) entering the body, to which the immune system responds with hyperactivation. In most cases, coughing attacks are caused by aeroallergens - substances in the air.
The following factors can cause cough due to allergies:
- pollen of weeds and medicinal herbs, trees, various flowers (garden, field, vegetable flowers, etc.);
- household allergens. This category includes household products in the form of aerosols (sprays, fresheners, powder, blush), powder and other detergents, book or house dust, tobacco smoke;
- molds;
- epidermal particles: feathers, fluff, fur or dander of pets, birds;
- vaccines and medicines;
- bee or wasp stings;
- some food products.
The mechanism of cough development due to allergies
A cough occurs when the bronchi are irritated due to allergens entering the body. A substance that acts as an allergen enters into chemical reactions with immunoglobulins - blood proteins responsible for the immune system.
During this process, histamine is released from these cells, causing the development of an allergic reaction in humans.
Once in the blood, this substance has a negative effect on the functioning of the body, causing such deviations as:
- muscle spasms of the respiratory and digestive systems;
- swelling of the vascular walls;
- adrenaline rush;
- increase in blood pressure.
It is spasms and irritation of the bronchi that provoke the development of an allergic cough.
Symptoms of an allergic cough and its differences from a cold
Despite the fact that an allergic cough is similar to a cold, it can be distinguished by a number of specific signs. Treatment can begin only after making sure of the allergic nature of its origin! A person should also try to remember what preceded the manifestation of such a condition - infection, hypothermia, or contact with an allergen.
There are 2 cardinal differences between an allergic cough and an inflammatory or bacterial one:
- color of sputum. With allergies, sputum is always clear;
- mechanism of cough development. Allergic cough in an adult at the first stage is always paroxysmal and can last from 2-3 hours to 3-4 days. Then its second stage begins, characterized by the release of a small amount of sputum of transparent color and medium viscosity.
This development of events during an allergic reaction is associated with the occurrence of spasms and severe swelling of the respiratory tract mucosa. At first, a person suffers from severe bronchospasm and cannot control coughing attacks. To prevent possible suffocation, the body relieves bronchial irritation by secreting mucus.
In addition, the distinctive symptoms of cough due to allergies are:
- it appears unexpectedly, most often at night;
- can be dry. Only after a prolonged coughing attack can a person cough up a small amount of clear mucus;
- accompanied by severe itching in the larynx and difficulty breathing;
- there is no increase in body temperature;
- a rash and dermatitis may be observed on the skin;
- the throat does not turn red, there is no discomfort when swallowing;
- there is no transition from a dry cough to a wet cough;
- most often occurs in the spring.
An allergic cough is dry and barking in nature; a person is unable to control it. This condition is accompanied by the inability to breathe normally, wheezing and whistling in the chest. And with a respiratory disease, it is still controllable, quickly turns into wet, bringing relief.
Diagnostic measures
If a dry cough due to allergies does not go away for a long time, it is worth visiting an allergist, therapist or pulmonologist. They will conduct the necessary examination and send you for laboratory testing.
To identify the irritant and cause of an allergic cough, the following types of differential diagnosis can be prescribed:
- detailed blood test;
- swab from the throat and nasal cavity;
- sputum examination;
- fluorography;
- skin tests;
- bronchoscopy;
- electrocardiogram;
- radiography;
- spirometry;
- biopsy;
- Mantoux test;
- PCR diagnostics.
Detection of eosinophil cells in an amount of 5% and an increase in the level of immunoglobulin E in the blood will indicate the development of an allergy.
What to do first?
To alleviate the condition and stop severe coughing attacks, you can take the following measures:
- if the allergen is known, it is necessary to completely avoid contact with it;
- gargle and rinse nasal passages with salt solution or water;
- take an antihistamine;
- carry out wet cleaning and remove dust from all surfaces, including upper cabinets and hard-to-reach places;
- ventilate the room;
- remove from the room all things and objects that can accumulate dust: carpets, rugs, blankets. Or you can replace them with hypoallergenic ones with padding polyester filling;
- remove pets from the premises and exclude contact with them;
- wash things only with laundry or baby soap.
Having taken such measures, it is necessary to look at the body’s reaction. If the cough does not subside, be sure to consult an allergist.
Treatment of allergic cough
Treatment of allergic cough in a hospital is carried out according to the following scheme:
- Prescribing antihistamines. This group of medications lowers histamine levels. Among them are older generation drugs, for example, Tavegil, Suprastin and Diazolin. But they cause side effects such as drowsiness and lethargy, so they are contraindicated for people driving vehicles or working in jobs that require quick reactions. In addition, they are quickly addictive and stop helping over time. Therefore, it is worth giving preference to new generation products, such as Zyrtec, Zaditen or Claritin. They differ in the duration of action and do not affect well-being. But they should be taken only after doctor's approval. You should also know that if the allergen is pollen or plant flowers, use Ketotifen.
- Use of bronchodilators. Such medications are designed to relax the muscles of the bronchi and eliminate spasms, which will greatly facilitate coughing. For example, they may prescribe Salbutamol, Beclamethasone or Eufillin. They can be bought in the form of inhalers or in tablets.
- Use of mucolytics or expectorants. Such remedies are used in cases where a cough is accompanied by difficult-to-discharge transparent sputum. They help thin the mucus in the bronchi and improve the coughing process. Bromhexine, Ambroxol and Mucaltin are considered the most effective.
- Purpose of enterosorbents. It is advisable to take them only in cases where the cough is caused by an allergen entering the body with food. Products with a sorbing effect can quickly remove toxins from the body and neutralize them, thereby cleansing the body. Such sorbents as Smecta, Polypefan, Enterosgel, Polysorb are recognized as effective.
In addition, in a hospital setting, certain procedures may be prescribed to combat a specific allergen. Eg:
- desensitization . This procedure is similar to vaccination. A small dose of the allergen is injected under the person's skin. The dosage of the administered substance is gradually increased, while reducing the time intervals between injections. This will allow the body to get used to the allergen, reducing its sensitivity. But such treatment is lengthy and takes time. In this case, the allergen must be precisely known. For example, it could be pet fur, plant pollen, or insect bites;
- blood purification (hemosorption, immunosorption, plasmapheresis, lymphocytopheresis) . Such methods are used only in the most severe cases, when it is necessary to cleanse the body of antibodies and allergens. With immunosorption and hemosorption, the blood is purified from harmful elements by passing it through absorbers (special sorbents). With lymphocytopheresis and plasmapheresis, the blood is divided into parts and treated with cleansing substances.
Inhalations
Dry, barking cough and its accompanying symptoms in adults are also treated with the help of a nebulizer - a device designed for inhalation for bronchitis, tracheitis, colds and pharyngitis. It is filled with saline solution or mineral water. The device turns all liquid into steam, which helps clear the airways of irritants (allergens) and moisturizes their mucous membranes.
Mineral water can be replaced with special solutions:
- "Pulmicort";
- "Berodual";
- "Eufillin";
- "Ventolin";
- "Berotek".
Such drugs help expand the lumen of the bronchi, thereby facilitating breathing and reducing spasms. Such solutions for inhalation must be used and diluted strictly according to the instructions or prescription of a doctor.
Instead of pharmaceutical solutions for inhalation, you can also use herbal tinctures prepared from plants such as:
- Datura leaves;
- sage;
- rye;
- chamomile;
- thyme.