Bronchial asthma is an inflammatory disease of the respiratory tract, characterized by a chronic course associated with increased bronchial reactivity. The prevalence of this pathology today is approximately 5-6%, each year it causes 0.5% of deaths. The incidence of asthma is increasing annually throughout the world, especially among children. We will talk about what this disease is, for what reasons it occurs, and what the symptoms are, as well as about the features of diagnosis and treatment of bronchial asthma (in particular, physical therapy methods).
Why and how the disease develops
Increased reactivity (or hyperreactivity) of the bronchi, as a rule, occurs in response to the entry of a particular allergen into the body - a type I hypersensitivity reaction develops. The development of an attack of the disease can be provoked by:
- pollen of flowers and other plants;
- house dust (or rather, the mites found in it);
- mold, pet hair;
- Food;
- household chemicals and cosmetics;
- medications;
- industrial hazards;
- infections;
- active and passive smoking.
Undoubtedly, unfavorable environmental conditions, hereditary factors, and psychosocial conditions also play a role.
So, the allergen enters the body and causes a cascade of biochemical reactions in it, as a result of which the wall of the bronchi spasms, their mucous membrane swells and secretes a large amount of secretion, and the lumen significantly narrows. These changes cause a number of symptoms characteristic of bronchial asthma.
Symptoms
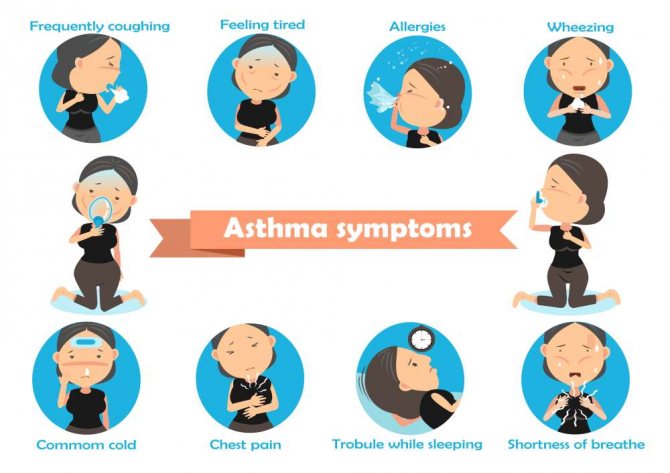
Bronchial asthma occurs in a paroxysmal manner - periodically, in the early stages of the disease. After direct contact with the allergen, characteristic attacks occur, accompanied by sudden shortness of breath, moist wheezing that can be heard at a distance, difficulty breathing, and a feeling of congestion in the chest. The attack ends with a cough with the discharge of thick viscous “glassy” sputum.
With a long course of the disease, inflammatory changes develop in the bronchi, and attacks occur more often even without connection with an allergen, but under the influence of any provoking factors - a strong odor, cold air, physical activity, inhalation of cigarette smoke, as well as against the background of viral infectious diseases.
During the period of remission, the symptoms of the disease are minimal or completely absent.
Depending on the frequency of asthma attacks, there are 4 stages of bronchial asthma:
- I – intermittent (asphyxiation attacks occur less than once every 7 days, exclusively after contact with an allergen; nightly – 2 times a month or less; exacerbations of the disease are short-term, easily stopped; respiratory function indicators are within normal limits (FEV1 ≥ 80% from the proper value, FEV1 variability < 20%));
- II – mild persistent (attacks of shortness of breath occur more often than once every 7 days, but less than once a day; night attacks - more often than 2 times a month; FEV1 is greater than or equal to 80% of the norm, its variability is less than or equal to thirty%);
- III – moderately severe persistent bronchial asthma (attacks occur every day, at night - more than once a week; exacerbations of the disease disrupt the patient’s activity and sleep, he needs daily bronchodilator drugs; FEV1 ranges from 60 to 80% of normal, FEV1 variability over 30%);
- IV – severe persistent (symptoms of the disease occur daily several times a day; night symptoms more often than once every 7 days; frequent exacerbations of the disease, during which the patient’s physical activity is significantly limited; FEV1 is 60% or less of normal values, its variability is more than thirty%).
The course of asthma depends on the age at which it debuted. If the disease manifests itself in early childhood, then during puberty of most patients it enters the stage of spontaneous stable remission and does not bother the patient for many years or even his entire life. For people who fell ill while at a young or middle age, several options are possible: in a third of them spontaneous remission may occur, in another 30% the disease proceeds with constant alternating periods of exacerbation and remission, but is characterized by moderate severity, and in the last 30% In most cases, it is difficult, progresses steadily and leads to serious complications in a short time.
Breathing exercises
Physiotherapy for bronchial asthma may involve breathing exercises. It is carried out in the morning or evening. First you need to stand at the open window for 10 minutes. You need to correctly distribute inhalations and exhalations. They differ in duration. Inhale slowly, deeply. At the same time, the shoulders are raised. Exhale quickly. Shoulders drop sharply.
Next, take a deep breath, raising your arms above your head. Palms squeeze. In this case, the exhalation will be longer. Hands are gradually lowered. The exhalation should be 2 times longer than the inhalation.
Having considered the main methods and features of physiotherapy for bronchial asthma, we can draw conclusions about the high effectiveness of such procedures. They are indicated for almost all patients with a similar illness, if they have no contraindications.
Diagnostic principles

The doctor will suspect that the patient has bronchial asthma at the stage of collecting complaints, life history and disease data (if this pathology is suspected, it is collected in great detail in order to form a complete picture of it; special questionnaires have also been developed for these purposes).
The doctor’s fears will be confirmed by data from the objective status of the patient, namely auscultation (listening) of the lungs: whistling moist rales will be detected (directly during an attack they can be heard not only through a phonendoscope, but also at a distance from the patient), as well as an extended expiratory phase. During the period of remission, these signs may not be detected; in addition, the intensity of wheezing decreases or is completely absent in the case of severe blockage (obstruction) of the bronchial lumen.
In addition, signs of allergic dermatitis or other manifestations of allergies may be found on the patient's skin.
Additional research methods to confirm or refute the diagnosis of bronchial asthma are:
- spirometry (this is the main and most informative method for diagnosing this disease; it is this that allows you to register FEV1 indicators (and their variability) that characterize the stage of the pathological process; in addition, it is used to determine the reversibility of the process in the bronchi - first they simply do spirometry, record its results, and then they give the patient a drug that dilates the bronchi and repeat the study; if the results have improved by 20% or more, this indicates that the patient has bronchial asthma, and if they have remained virtually unchanged, this speaks in favor of another lung pathology called COPD) ;
- plethysmography (allows us to identify an increase in airway resistance that occurs with bronchial obstruction);
- peak flowmetry (a self-monitoring method that allows the patient to independently monitor indicators of respiratory function (namely, peak expiratory flow) and, based on the results, draw conclusions about the factors provoking an attack and the effectiveness of the therapy; a special device is used for this - a peak flow meter);
- examination of the level of blood gases (helps to detect disturbances in the gas balance of the blood associated with the disease - a decrease in the oxygen content in it (hypoxemia) and an increase in carbon dioxide (hypercapnia));
- study of bronchial reactivity (sensitivity of the bronchi to the effects of provoking factors; carried out in cases of characteristic complaints of the patient in combination with normal indicators of respiratory function);
- assessment of allergic status (as a rule, skin tests with allergens are performed or IgE is determined in the blood serum);
- examination of sputum under a microscope (it detects Kurshman spirals (sputum from the lower respiratory tract, which has taken their form) and Charcot-Leyden crystals, as well as casts of bronchioles, accumulations of epithelium, bacteria and an increased content of neutrophils and eosinophils);
- complete blood count (eosinophilia (more than 5% of these cells) may be detected).
Exercises for exacerbations
Physiotherapy for bronchial asthma is carried out during an exacerbation in the hospital, but only after the patient’s condition becomes stable. A number of physical exercises can help relieve an attack in combination with drug treatment. They are carried out under the supervision of a doctor.
The patient lies on his back. I put a high pillow under my head. The air is inhaled through the mouth. At this time, the stomach is slightly inflated. They also exhale air through the mouth. At the same time, the stomach is pulled in.
Next, you need to sit on a chair, focusing on its back. As you inhale, raise your arms up. The elbows are bent. They put their hands on their shoulders. As you exhale, they are raised up again and lowered along the body.
Sitting on a chair, arms move in different directions. As you exhale, bend forward, reaching your hands to the floor. Exercises are repeated no more than 5 times. If signs of fatigue appear, stop gymnastics.
Principles of treatment
Unfortunately, it is impossible to completely get rid of bronchial asthma today. However, if the patient follows all the doctor’s recommendations and receives adequate therapy, his condition improves significantly and often stable remission occurs. That is, the purpose of treatment is to maintain a satisfactory quality of life for the patient.
Etiological treatment
Its essence comes down to eliminating the effects of all possible allergens on the body. These measures are especially effective at the early stage of the disease - stopping contact with substances that provoke an attack can even lead to stable remission.
The patient should take the following actions:
- limit possible contacts with plant pollen (probably even leave your permanent place of residence to another region for the period of flowering of the plant that causes an allergic reaction);
- remove carpets and soft toys from the home, keep books in closed cabinets, wash floors daily, wipe off dust;
- change bed linen regularly;
- do not have pets;
- exclude from the diet foods that are potential or previously identified allergens;
- change place of work (if you are allergic to any industrial substances).
Drug treatment
Which groups of drugs will be prescribed to a patient by a doctor depends directly on the stage and characteristics of the course of his disease. They can be introduced into the body in various ways - inhalation, by injection/infusion (popularly called droppers) or in the form of tablets by mouth.
Basic therapy
There is such a thing as basic therapy for asthma. The drugs that are used in this case have a direct effect on the bronchial mucosa, eliminating their pathological changes. They must be applied on an ongoing basis - not in courses, but constantly, long-term, often and for life. It is these drugs that allow you to control the course of asthma, preventing its progression.
Such medications are:
- drugs of choice are inhaled glucocorticoids (beclomethasone, fluticasone, budesonide and others);
- systemic glucocorticoids (methylprednisolone, prednisolone);
- long-acting bronchodilators (inhaled beta2-agonists (formoterol, salmeterol) and xanthines (theophylline, aminophylline and others));
- cromones (the main ones are sodium cromoglycate, nedocromil sodium);
- leukotriene modifiers (montelukast, zafirlukast).
Indications
Physiotherapy for bronchial asthma in children and adults gives good results. It is used in combination with other techniques. Physiotherapy has a special effect on internal organs and stimulates their proper functioning. This allows you to increase blood circulation, strengthen muscles and coordinate movements correctly.

Physiotherapy is carried out for patients with varying degrees of severity of the disease. In this case, the age of the patient and the type of his disease do not play a role. Physiotherapy for bronchial asthma in adults in a hospital is carried out under the supervision of doctors. If the disease is of mild severity, the procedures are carried out at home, as well as when visiting the hospital. During physiotherapy, special equipment is used.
Exercises, strength of influence and other aspects are prescribed by the doctor in accordance with the type and characteristics of the disease, as well as the characteristics of the patient’s body. The more advanced the stage of the disease, the worse the drainage function of the bronchi becomes. The mobility of the chest decreases. Physiotherapy helps normalize the ventilation process. As a result, gas exchange becomes correct.
The main objectives of physiotherapy are to restore the functionality of the respiratory organs and normalize metabolic processes in them. Also, special techniques and techniques increase the endurance of the body and strengthen it. With significant mucus production during the period of spasm, the drainage function of the bronchi improves. They remove phlegm faster, which significantly reduces the time of an attack and its negative consequences. Physiotherapy can improve the patient's quality of life.