- Classification of the disease
- Causes of neurodermatitis
- Symptomatic manifestations
- Diagnostic measures
- Treatment of neurodermatitis
- Treatment of neurodermatitis with folk remedies
What is neurodermatitis: symptoms, treatment, prevention. The disease is an inflammation of the skin, manifesting itself in the form of allergic or chronic rashes. On the planet, approximately 40% of people suffer from neurodermatitis, in most cases this pathology occurs among children. The disease can last for a long period of time and disappear by the time of puberty.
Neurodermatitis on the head, face, arms and legs
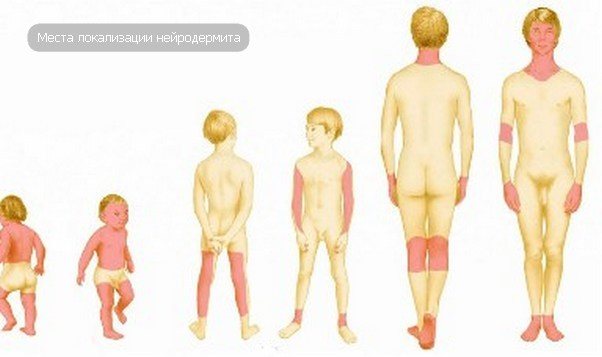
There is an extensive list of skin diseases that are characterized by this feature - severe itching, which is permanent, and it can also grow and increase over time. Remission of neurodermatitis usually lasts no more than a year. Foci of the inflammatory disease occur in various parts of the body: from the head to the feet. Neurodermatitis refers to diseases that combine allergic and nervous nature. It has been established that there is a close relationship between strong experiences and periods of exacerbation. Let us consider the main foci of the disease and methods of their treatment.
Types of disease in adults
Each adult will have different manifestations of this disease . There are several types of neurodermatitis, which differ from each other depending on the degree of damage to the skin and the development processes. The disease is divided into types:
- Limited neurodermatitis is the formation of rashes that are localized in one separate area of the body. The locations of such lesions are concentrated in the popliteal and elbow bends, the inner thighs, scrotum, legs, anus, and so on.
- Hypertrophic neurodermatitis or Ehrmann's neurodermatitis. The form is considered not common; it causes inflammatory processes that are localized in the inner femoral region. The inflammation is tumor-like in nature. Often the disease process is accompanied by the appearance of formations that look like warts.
- Linear neurodermatitis. This type of disease is accompanied by inflammation, which develops mainly on the extensor surfaces of the upper and lower extremities. Inflammations have the shape of stripes. Most often the surface is flaky or warty.
- Follicular neurodermatitis. This form of the disease is characterized by the location of the rashes, localized along the hair follicles. In this case, pointed-shaped papules are formed.
- Hyperemic neurodermatitis. This species is characterized by loss of skin pigmentation in areas of inflammation.
- Psoriasiform neurodermatitis. The disease spreads mainly to the neck and head. Externally, the rashes are compacted redness, which are covered with small scales.
- Diffuse neurodermatitis. This form of the disease is often called atopic neurodermatitis. After all, the disease is considered a more severe form. Diffuse neurodermatitis is characterized by the appearance of multiple lesions. Most often they are localized on the lower and upper extremities, torso and other areas of the body. After severe itching, highly pigmented thickenings and areas appear. At the same time, the skin acquires a brown tint and becomes dry.
With any type of disease, the patient experiences noticeable discomfort. But all forms of the disease will require timely treatment in order to avoid unpleasant consequences and complications in the future.
Neurodermatitis of the scalp
As a rule, neurodermatitis of the scalp is somewhat problematic to treat. This is explained by the fact that hair partially blocks access to inflammatory foci. It is worth clarifying that the patient’s hair does not fall out, which is why many people delay visiting the doctor. And delay in the case of neurodermatitis on the head can have quite serious consequences. Neurodermatitis on the neck often occurs due to the appearance of lesions on the head that were not noticed in time.
The main and characteristic symptom of neurodermatitis is, of course, constant and severe itching, which begins to intensify over time. Then flaking of the scalp appears, a pronounced rash that gradually spreads throughout the entire scalp as you scratch. Then small foci of inflammation begin to merge into one large spot, which becomes covered with a hard crust. Such a formation may crack over time and an ichor appears.
Treatment of neurodermatitis of the scalp begins with an accurate diagnosis and, if possible, identification of the underlying cause. If the attending physician notices the appearance of a rash after suffering an emotional shock, the patient will be prescribed sedatives. Anti-inflammatory and antihistamine drugs are also prescribed to counteract the allergic effect and reduce severe itching. External means are hormonal ointments and creams. Preventive measures to prevent exacerbation include maintaining a healthy lifestyle, minimal contact with the allergen and a minimum of stressful situations.
Signs and causes of occurrence
The main symptoms of the disease are reddish rashes in the neck, gradually spreading to the face and scalp. The patient complains of incessant itching and pain when washing and combing his hair.
If the disease manifests itself not only on the scalp, but also on the face, then the following will be affected:
- cheeks,
- lips,
- area of the nasolabial triangle,
- chin,
- forehead,
- skin around the eyes.
On the head, as can be seen in the photo, scaly (psoriasiform) neurodermatitis most often occurs, which affects the back of the head.
If timely treatment is not started, papules will form on the surface of the dermis.
Their damage and scratching leads to the appearance of microtraumas, the spread of infection and an increase in the inflammatory process .
The main reason for the occurrence and development of neurodermatitis in children and adults is an allergic reaction, which can be caused by the following irritants:
- consumption of certain foods (citrus fruits, chicken eggs, strawberries, tomatoes),
- exposure to low temperatures on the skin,
- contact with pollen, household dust or pet hair.
Among the factors contributing to the appearance of neurodermatitis are:
- various types of intoxication,
- chronic diseases of internal organs,
- ENT diseases,
- abuse of diets,
- eating disorder,
- malfunction of the digestive tract,
- prolonged stress, depression, nervous breakdown.
Some patients are diagnosed with neurodermatitis, caused by hereditary diseases, hormonal imbalance, and a malfunction of the immune system.
Neurodermatitis on the face
Neurodermatitis on the face causes significant difficulties, since this is the most exposed area of the skin, which is constantly exposed to various environmental influences. The disease also tends to spread to other parts of the body. First of all, a person feels severe itching in the neck area, then the disease progresses and a localized rash appears on the cheeks, forehead, and around the eyes. Severe itching and reddened areas of the skin, called papules, can merge into one inflammatory focus. The most dangerous situation that can arise is the introduction of infection through dirty hands.

Treatment of neurodermatitis on the face is complex: it is necessary not only to select appropriate medications, but also to take care to provide your body with favorable conditions. And the first most important step is to avoid contact with allergenic substances, as well as to avoid physical and emotional stress. The specialist will prescribe how to treat neurodermatitis on the face; you should not solve this problem yourself. Drug therapy usually consists of the following drugs:
- Antihistamines.
It is recommended to pay attention only to modern products that have an effective effect and practically do not cause side effects. Modern antihistamines are approved for use by pregnant women, without any threat to the fetus.
- Sedatives.
Sedatives are prescribed to patients for two important purposes - normalizing the nervous system, as well as relieving patients from emotional turmoil or stress.
- Ointments and creams with glucocorticosteroids.
A fairly effective method of treatment, however, it has its negative sides. The positive qualities include a fairly rapid therapeutic effect, since the drug immediately reaches the affected area.
Treatment of neurodermatitis
So, a diagnosis of “neurodermatitis” has been made: the symptoms and their treatment should be carried out comprehensively exclusively by a dermatologist or infectious disease specialist; self-medication can end very badly. For an ailment such as neurodermatitis, treatment usually begins with the removal of painful symptoms with the use of external, restorative and highly targeted medications to eliminate associated health problems, plus the following measures:
- neutral antipruritic creams and ointments for exfoliation and resorption of skin lesions;
- drug therapy aimed at reducing aggravating factors;
- stopping contact with identified allergens;
- drawing up an individual daily regimen, including a full night's sleep, an individually selected diet, physical activity, sun and air baths, wearing clothes made from natural fabrics;
- special exercises to increase the tone and reserve forces of the body in the fight against the disease;
- prescription of vitamin and mineral complexes;
- inpatient treatment (if necessary);
- prescribing hormonal drugs for severe disease;
- physiotherapeutic procedures;
- combating depression by raising a positive attitude and thinking;
- antibacterial agents when adding secondary infection;
- sanatorium-resort treatment on the sea coast, water procedures with thermal waters and mud therapy during periods of remission.
When undergoing a course of treatment, it is necessary to give up emotional stress and all types of overwork, and patience and perseverance are needed to obtain positive results from complex therapy.
Neurodermatitis on hands
Atopic dermatitis has many characteristic signs, among which neurodermatitis on the palms is not the least important - as a rule, the knee and elbow bends, hands, and forearms are the first to suffer. However, severe rashes, redness, painful cracks or sores are not the only things that worry a patient with this disease. Secondary signs of neurodermatitis also appear: sleep disturbance, irritability, decreased blood pressure, apathy, depression, impaired secretion of gastric juice.

Treatment of neurodermatitis on the hands is a rather problematic and lengthy process. Before making a diagnosis and prescribing treatment, an accurate diagnosis must be carried out, since many of the symptoms are similar to other skin diseases. It is necessary to treat neurodermatitis on the hands comprehensively, eliminating not only external manifestations, but also internal disorders. Then a whole list of necessary medications is prescribed: sedatives, antihistamines, vitamins, ointments and creams.
The psychosomatics of neurodermatitis on the hands implies the psycho-emotional nature of the progression of the disease. There are common cases when, during periods of severe shocks or stressful situations, people’s hands begin to itch very much. Also, periods of exacerbation can be directly related to previously suffered mental turmoil.
Treatment of patients with limited neurodermatitis
Guided by the clinical picture of the disease and the results of immunological and biochemical studies, the doctor can easily establish a diagnosis. After assessing the symptoms, treatment is prescribed. The recovery process in adults is divided into two areas:
- getting rid of existing violations;
- the use of therapeutic methods aimed at preventing relapses.

Treatment of the disease is carried out comprehensively, taking into account the individual characteristics of the body.
To combat the disease, drugs of different action groups are prescribed:
- antihistamines (relieve itching, prevent plaques from spreading to healthy skin).
- Enzymes (normalize the functioning of the gastrointestinal tract).
- Corticosteroid drugs (hormone therapy). The drugs contain substances with strong antiallergic properties. They bring particular relief during the period of exacerbation of the disease. The disadvantage of this treatment is that the patient’s body quickly becomes accustomed to the hormones. An overdose of hormonal drugs can lead to various side effects. Such treatment is not prescribed for children, and short courses for adults.
- Multivitamins.
- Local treatment of disease foci (cream or ointment). The choice of drug is made taking into account the causes of the disease, its severity, the patient’s age and concomitant diseases.
General strengthening of the body is achieved by long stays in the fresh air and a balanced diet.
Various physiotherapeutic procedures (phonophoresis, electrophoresis of antipruritic and absorbable drugs) give good results.
Neurodermatitis on the legs
There are two main causes of neurodermatitis on the legs: neurogenic and allergenic. However, in addition to the reasons, there is a wide range of factors that contribute to the development of the mechanism of inflammatory disease. The characteristic localization is determined by the characteristics of the progression of neurodermatitis. Experts name several types of this disease, but the pathology on the legs is often linear or limited. From this it follows that the rash has a large affected area. Often the main lesions appear on the folds, the inner side of the thigh, and sometimes the foot.
Neurodermatitis on the legs will need to be treated with many medications. For external use, zinc or dermatol ointment or cream with menthol are suitable - they significantly alleviate the patient’s condition, reduce itching and have a disinfecting effect. We must also not forget about sorbents that help remove toxins from the body. Antihistamines and sedatives form the basis of the treatment of neurodermatitis.
Symptoms of neurodermatitis
Before treating neurodermatitis in adults, you need to understand what neurodermatitis looks like. The main symptoms of dermatitis:
- intense itching,
- rash,
- redness,
- peeling of the skin,
- darkening of the skin,
- nervous disorders,
- low blood pressure.
The patient's skin begins to itch before rashes and redness appear. Constant scratching leads to the formation of shiny knotty surfaces. Over time, the nodules acquire a pink-brown color, they merge into a single lesion with smeared contours. The affected area begins to peel, become crusty, and turn purple or blue.
Doctors associate the darkening of the skin with hypofunction of the adrenal glands, which is provoked by the disease. Less corticosteroids enter the blood, and accordingly more ACTH (adrenocorticotropic hormone) is secreted; it contains sections of melanocyte-stimulating hormone. This substance stimulates the production of pigments by skin cells. Blood tests in patients with neurodermatitis often show low glucose levels; this is also associated with hypofunction of the adrenal glands and a lack of glucocorticoids. The patient's body weight decreases. Due to constant itching, fatigue and irritability increase, and sleep disturbances may occur.
The disease neurodermatitis is chronic and worsens in the cold season. The health status of patients improves in summer and spring. The symptoms of the disease appear most acutely if the foci of inflammation are localized on the hands. Hands more often interact with the external environment and moisture.

Neurodermatitis is accompanied by hypofunction of the adrenal glands
How to properly treat neurodermatitis: the best medicines and folk recipes
Neurodermatitis in medical practice has a second name - atopic dermatitis. This skin disease is one of the hereditary diseases that can develop asymptomatically over a long period of time. Exacerbation of neurodermatitis occurs when exposed to unfavorable external factors or a significant deviation in the functioning of important body systems.
The disease can be treated in several ways, but the main goal of any therapy is to maximize the period of remission.
Manifestation of diffuse form

Diffuse neurodermatitis
Diffuse (common) neurodermatitis has another name - Darier's prurigo vulgaris. This form refers to a severe type of the disease, in which the lesions are numerous, tend to grow peripherally, sometimes the process becomes so widespread that it takes the form of erythroderma (generalized inflammation of the skin with significant swelling, hyperemia and the appearance of blisters with further detachment of the epidermis and the formation of erosive lesions). surfaces).
The disease begins in children in infancy or early age with the appearance of diathesis, which over time develops into eczema and at the age of 6–8 years transforms into neurodermatitis.
With this form of the disease, the first sign is intense itching, and then skin manifestations appear in the form of pink, swollen and thickened lesions on the skin that are confluent in nature. Small flat nodules with a shiny surface appear in certain areas of the skin. In the affected area there is peeling and hemorrhagic crusts appear. Most often, the face is affected first, then the inflammation spreads to other parts of the body. It becomes swollen, hyperemic, a pronounced skin pattern and fine-plate peeling appear. In many patients, the red border of the lips and the surrounding skin are involved in the process (atonic cheilitis). When a secondary infection attaches to the lesions, pyoderma develops - purulent inflammation of the skin.
As the itching intensifies, neurological disorders in patients progress more and more - insomnia becomes more severe, patients become very irritable, and sometimes become depressed.
Diffuse neurodermatitis has a chronic course, which is characterized by exacerbations in the autumn-winter period, and spontaneous remission occurs in the summer.
What it is?
Neurodermatitis is an inflammatory process that develops on the skin. The disease has a chronic form and can be inherited. Atopic dermatitis manifests itself in the form of rashes on the epidermis, accompanied by severe itching. The origin of the disease is always due to its neuro-allergic nature.
In medical practice, neurodermatitis is divided into three forms of development:
- infant type (the second name of the disease is diathesis, the disease is widespread in newborns and children under two years of age);
- children's type (children from 2 to 12 years old are at risk of the disease; the occurrence of a skin rash may be accompanied by abundant pigmentation of the skin);
- adolescent-adult type (in adulthood, neurodermatitis in most cases acquires a chronic form, and its exacerbation occurs only in the presence of certain factors).
Clinical picture

Limited neurodermatitis usually produces no more than two foci of inflammation. They are dry, but after scratching they become wet, crusty and can bleed if it is severe.
Typical localization of focal dermatosis:
- back of the head;
- inner surface of forearms, thighs;
- popliteal, elbow bend;
- shin;
- scrotum;
- perianal zone;
- crotch.
The defining symptom of the disease is severe, painful itching and redness. Afterwards, flat papules form. They merge into oval plaques and then unite into one purple lesion.
A limited form of neurodermatitis of the external genitalia and perianal area can manifest itself only as itching, without typical signs on the skin.
Rashes with limited neurodermatitis are symmetrical and have a clear, demarcated structure.
What does the hearth look like:
- The internal (central) part is subject to infiltration (inflammation) and lichenification (thickening, strengthening of the skin pattern).
- From the middle, closer to the edges, shiny, isolated papules are visible.
- Specific pigmentation is observed along the periphery.
If treatment is not prescribed in time and the symptoms worsen, a secondary infection joins the scratching and this leads to a pustular lesion.
The nervous system suffers from severe, debilitating itching. External, cutaneous symptoms are accompanied by emotional instability, insomnia, mood swings and extreme irritability.
Reasons for development
The main factors contributing to the development of neurodermatitis at any age are considered to be disruption of the internal systems of the body and a decrease in the level of immunity. In some cases, the disease can be transmitted at the genetic level, especially if there are allergies in the family. Numerous external factors can provoke an exacerbation of neurodermatitis, including excessive air pollution, unfavorable atmospheric conditions or harmful working conditions.
The causes of neurodermatitis can be the following factors:
- constant stressful situations or increased mental sensitivity;
- development of chronic infectious diseases;
- diseases of the digestive system;
- lack of vitamins in the body and poor nutrition;
- long-term use of potent drugs;
- deviations in the performance of the central nervous system;
- diseases of the gastrointestinal tract;
- intoxication of the body;
- constant mental stress;
- physical exhaustion of the body.
Symptoms and diagnosis
The manifestation of neurodermatitis occurs gradually. First, rashes appear on the neck and face, spreading to the folds of the skin. When the disease becomes more complicated, the rash covers all parts of the body. The symptoms of neurodermatitis are accompanied by general lethargy of the body, fatigue, decreased blood pressure and lack of appetite.
The main symptoms of neurodermatitis are the following conditions:
- severe skin itching (at night the symptom becomes especially painful);
- rashes are accompanied by peeling of the skin;
- the lesion consists of three zones (an enhanced pattern in the center of the lesion, replaced by shiny papules, and a border in the form of pigmentation);
- the first signs of neurodermatitis appear on the neck, face and folds of the skin;
- rashes may appear as fluid-filled blisters.
In most cases, neurodermatitis can be diagnosed based on the characteristic external signs of the disease. To clarify the diagnosis, the doctor may prescribe additional examinations. The patient will need to undergo an immunogram, general blood and urine tests, cultures and consult with an allergist. Additionally, examinations by specialized specialists may be scheduled.
- hypertrophic type (the disease affects the groin area);
- diffuse type (symptoms of neurodermatitis appear on the face, neck and folds);
- follicular type (atopic dermatitis affects only the scalp);
- limited type (the disease affects specific areas of the skin and has clearly defined boundaries);
- psoriasiform type (a rash appears on the head and face, characteristic scales appear on the affected areas of the epidermis);
- linear type (rash appears exclusively on the skin of the extremities).
Why does neurodermatitis develop?
Experts believe that common causes of neurodermatitis are:
- weakened immunity;
- intoxication of the body;
- inflammatory processes;
- metabolic disease;
- gastrointestinal diseases;
- hereditary predisposition;
- mental or physical exhaustion;
- poor nutrition and irregular daily routine;
- neuropsychological disorders, neuroses, stress, depression.
Despite the variety of factors that provoke the development of neurodermatitis, dermatologists believe that the disease triggers an allergic mechanism. At the first meeting with an allergen, the body produces antibodies to a new compound, but the second time the antibodies combine with the body and are carried through the bloodstream to all tissues and organs and destroy the membranes of their cells.
During the process of degranulation, active substances are released, among which is histamine. This substance causes redness and thickening of the skin, an increase in local temperature and a feeling of itching or burning. In case of secondary infection, body temperature rises.
Scientists explain damage to the nervous system as the cause of neurodermatitis by dysfunction of peripheral nerve fibers. Therefore, the patient begins to experience severe itching, and rashes appear on the body. The desire to scratch the skin leads to injury, increased intensity of itching and swelling of the tissue.
Neurodermatitis is not a contagious disease. Often its root cause is a genetic predisposition to allergies. The human body can react with illness to any irritant - from the fur of a pet to your favorite cosmetic product.
Neurodermatitis - types and symptoms
Neurodermatitis is divided into several varieties. The classification was developed according to the criteria of “location of rash localization” and “degree of prevalence of the process.”

Based on this, the disease is diagnosed by type:
- Limited. The most common form of neurodermatitis, affecting small areas of the skin.
- Diffuse. Pathological elements appear multiple and occupy large areas of the body. Usually the rash is localized on the face, neck, knee-elbow cavities, and arms. Neurodermatitis on the hands is a subtype of diffuse neurodermatitis, its symptoms can be seen in the photo (above), and the principles of treating the disease will be described below.
- Linear – affects the upper and lower extremities.
- Follicular – affects the scalp.
- Psoriasiform - appears on the neck and head.
- Hypertrophic - localized in the groin area.
- Decalvating - a rash forms on the hairy areas, subsequently the affected hairs fall out.
The main symptom of the acute stage of the disease is unbearable itching, which intensifies at night. Other signs appear later. At first, the rash resembles red spots, papules and plaques that tend to merge. Due to scratching, the body is affected by a secondary infection, which turns the elements into pustules - vesicles with contents. The skin tissues swell and appear puffy.
External signs of neurodermatitis in adults are shown in the photo.

Doctors see 3 zones on a patient’s body:
In chronic patients in remission, a zone of lichenification appears due to irritation of the skin, because it is difficult for a person to resist scratching. Multiple papules form on the scalp of the body. The skin of the fingers, palms and soles cracks.
If neurodermatitis develops on the face, the patient notices increased eyebrow loss and an abnormal shade of the eyelids. Skin color changes due to constant scratching. Pale pink papules form on the forehead and cheeks. Itching at the site of their localization intensifies periodically. If bright spots appear on the cheeks, they do not have clear boundaries, but constantly itch and begin to peel off.
The photo clearly demonstrates what neurodermatitis looks like on the face.

Scratching the skin of the face is dangerous due to the addition of pyococcal infection. Infection with pyococcus is recognized by a pronounced gray tint to the face. The skin becomes dry and flaky. It itches in both problem and healthy areas.
Features of neurodermatitis in children
Neurodermatitis most often affects children with allergies. The disease develops not only due to allergies to food, wool or pollen. In some babies, a predisposing factor is congenital intolerance to certain substances. Children with an unstable psycho-emotional background and problems with the nervous system are also susceptible to the disease.

How neurodermatitis in children will be treated depends on the specific symptoms. The traditional variant of the pathology is one inflamed focus (a larger number of zones are observed less frequently).
In the acute period, an erythematous area is detected on the skin, which subsequently transforms into a bizarre papule with a diameter of up to 3 mm. Several papules merge into a single lesion of any shape. As the pathology progresses, weeping begins.
Treatment options
Treatment of neurodermatitis at home includes several methods. Therapy with medicinal herbs and folk remedies has good indicators of effectiveness, but if complications occur, it is recommended to use medications. Before using them, it is important to consult with a specialist and carefully study the lists of contraindications specified in the instructions.
Pharmacy medicines
Neurodermatitis requires complex therapy. The list of medications used includes drugs from different groups, including potent drugs. A qualified specialist must draw up a course of treatment. Only a doctor can objectively assess the clinical picture of the patient’s health condition and identify the factors that provoked an exacerbation of atopic dermatitis.
Drugs used to treat neurodermatitis:
- antihistamines (Claritin, Tavegil, Diazolin);
- hyposensitizing drugs (sodium thiosulfate);
- neuroleptics (Thioridazine);
- sedatives (tinctures of valerian and motherwort);
- tranquilizers (Mebikar, Amizil).
Folk remedies
Alternative medicine recipes can be used not only to treat neurodermatitis, but also as a preventive measure. Natural components eliminate the inflammatory process well, accelerate cell regeneration and eliminate the consequences of skin rashes. Thanks to folk remedies, the period of remission of the disease can be significantly extended.
You can cure neurodermatitis using the following recipes:
- treatment with blue clay (mix sea salt and diluted blue clay in equal proportions, apply the preparation to the affected area of the skin and wait for it to dry, repeat the procedure daily for two weeks);
- ointment with herbs (mix valerian root, lily of the valley, calendula and eucalyptus in equal proportions, mix two tablespoons of lanolin or any fat with a teaspoon of the resulting preparation, use a skin treatment product);
- ointment with beeswax (mix any bird fat, tar and beeswax in equal proportions, place the preparation in a clay pot and leave to infuse for 4 hours in a preheated oven or on hot bricks, strain the mixture, cool and use to treat affected areas of the skin);
- lard, aloe juice and fir oil (mix 50 g of aloe juice with 5 ml of fir oil, add melted lard to obtain a homogeneous consistency, use a skin treatment product);
- infusion of Sophora japonica (pour two tablespoons of the fruits of the plant with a glass of boiling water; after infusion, the preparation can be used to treat affected areas of the skin or ingested).
Neurodermatitis on the face and head: photos, symptoms, causes, types and treatment in adults
Neurodermatitis is an allergic disease that manifests itself in the form of pronounced redness and thickening of the skin.
The disease is inflammatory in nature and affects patients of any age. Neurodermatitis on the head appears most often in young children and goes away by the end of puberty.
In adults, itchy red rashes appear not only on the face, but also on the neck, causing the patient a lot of discomfort.
Description and types
Pathology is one of the widespread diseases that require systematic long-term treatment under the guidance and supervision of an experienced allergist and dermatologist.
Depending on the extent of the affected areas, the following forms are distinguished:
- limited (Broca's neurodermatitis) - the rash is localized in separate areas, 1-2 oval-shaped foci are observed,
- diffuse - several foci of inflammation appear throughout the body.
There are the following types of neurodermatitis that affects the head and face:
- White, or depigmented. Its distinctive feature is the lightening of the skin in the affected areas.
- Exudative. Accompanied by the formation of small blisters filled with serous fluid. As a result of scratching, the papules burst and become covered with a rough crust, which cracks and causes microtraumas. This form is dangerous due to infection of wounds and the development of an inflammatory process.
- Hypertrophic. It is characterized by the appearance of large lumps that look like warts.
- Psoriasiform or scaly. Red spots, covered with a large number of small scales, form on the surface of the skin. Red itchy plaques appear in the affected area. Gradually merging, they form a compaction of considerable size.
In the photo below you can see a rash on the face, characteristic of neurodermatitis in adults. The disease worsens appearance and disrupts sleep. The spots itch very much and the skin feels like it’s on fire. Some forms of the disease cause pain at the slightest touch to the inflamed areas .
Signs and causes of occurrence
The main symptoms of the disease are reddish rashes in the neck, gradually spreading to the face and scalp. The patient complains of incessant itching and pain when washing and combing his hair.
If the disease manifests itself not only on the scalp, but also on the face, then the following will be affected:
- cheeks,
- lips,
- area of the nasolabial triangle,
- chin,
- forehead,
- skin around the eyes.
On the head, as can be seen in the photo, scaly (psoriasiform) neurodermatitis most often occurs, which affects the back of the head.
If timely treatment is not started, papules will form on the surface of the dermis. Their damage and scratching leads to the appearance of microtraumas, the spread of infection and an increase in the inflammatory process .
The cause of the occurrence and development of neurodermatitis in children and adults is an allergic reaction that can be caused by the following irritants:
- consumption of certain foods (citrus fruits, chicken eggs, strawberries, tomatoes),
- exposure to low temperatures on the skin,
- contact with pollen, household dust or pet hair.
Among the factors contributing to the appearance of neurodermatitis are:
- various types of intoxication,
- chronic diseases of internal organs,
- ENT diseases,
- abuse of diets,
- eating disorder,
- malfunction of the digestive tract,
- prolonged stress, depression, nervous breakdown.
Some patients are diagnosed with neurodermatitis, caused by hereditary diseases, hormonal imbalance, and a malfunction of the immune system.
Traditional medicine therapy
A dermatologist prescribes treatment for neurodermatitis on the face and head after a visual examination and laboratory examination. Drugs are selected taking into account the individual characteristics of the body, the nuances of the course of the disease and the presence of concomitant pathologies.
First of all, therapy is aimed at getting rid of unbearable itching and pain, the second stage is eliminating the cause of the disease . Then measures should be taken to restore the normal state of the epidermis.
Ointments
Dermatologists recommend using medications for external use - creams and ointments that are applied in a thin layer to the inflamed dermis. They are chosen based on the degree of development of the disease, the severity of skin damage and the cause of the disease. All prescribed drugs are divided into non-hormonal and corticosteroid.
These preparations are made on the basis of tar and dermatol, naphthalan oil and salicylic acid, ichthyol and corticosteroids. Some ointments (Celestoderm, Fluorocort, Dermovate) are approved for use strictly as prescribed by a doctor.
Self-medication with hormonal drugs can cause side effects and the development of withdrawal syndrome.
Corticosteroids are extremely rarely used in the treatment of neurodermatitis in young children (Prednisolone ointment, Hydrocortisone). Sinaflan, Dermovate are strictly prohibited for therapy in teenage girls.
The most effective ointments include:
- Trimistin. Promotes rapid healing of microtraumas, stops the development of the inflammatory process, softens the rough crust on the affected areas of the skin. Allows you to achieve a positive result in the treatment of neurodermatitis aggravated by infection.
- Prednicarb. Relieves itching, eliminates inflammation, stops the development of an allergic reaction. Prescribed in the presence of severe peeling, it helps soften keratinized particles and cleanse the upper layers of the epidermis.
- Bepanten. Fights itching, cleanses and restores damaged tissue.
- Eplan. Has an antiseptic and regenerating effect.
- Gistan. Recommended to combat flaking and itching.
- Fluorocort. Effective in exudative forms, stops inflammatory processes and relieves discomfort.
Before applying the ointment, the affected surface should be cleaned of any scales that have formed. For this purpose, special shampoos are used. They contain tar or antifungal substances (Nizoral, Sebozol, Perhotal).
Pills
Sometimes treating neurodermatitis with external means alone is ineffective. In such cases, the doctor selects systemic drugs depending on the cause of the disease.
- For stress or nervousness, sedatives are prescribed. They have a calming effect, helping to get rid of problems arising from nervousness (Sedasen, valerian extract, Novo-Passit).
- In case of an allergic reaction, antihistamines will be required: Tavegil, Cetrin, Pheniramine.
- Immunomodulators (Methyluracil, Sodium Nucleinate) help strengthen the body's defense system.
- In case of bacterial infection, antibiotics from the group of penicillins or cephalosporins are prescribed.
- To restore the normal functioning of the digestive tract, it is recommended to take enzymatic agents and sorbents (Panzinorm, Bifidumbacterin, Linex).
Folk recipes
Folk remedies prepared from medicinal plants will help soothe inflamed facial skin and get rid of discomfort, itching, burning and pain.
- Mix chopped thyme, plantain, elecampane, celandine, and string in equal parts. Pour boiling water over the finished mixture at the rate of 2 tablespoons of the mixture per glass of water. Leave in a water bath for 15 minutes. Cool, strain through cheesecloth folded in half. Use the decoction as a lotion to wipe your face in the morning and evening. The procedure is repeated until the signs of neurodermatitis disappear.
- Mix a tablespoon of string and thyme, pour 250-300 ml of boiling water, place in a thermos. Leave for 10-12 hours. The finished infusion is poured into an ice tray and left in the freezer. The resulting cubes are used to wipe the face in the morning. You can use this remedy after the signs of acute neurodermatitis disappear. Before use, it is advisable to consult your doctor.
- To prepare the ointment, you will need to take heated pork (internal) fat (50-60 g), fir oil (2 ml), aloe juice (60-70 g). Mix thoroughly until smooth and store in a cool place. Apply a thin layer to damaged skin areas in the morning and before bedtime for a week.
- You will need 10 ml of fir, eucalyptus, calendula, and valerian oil. The mixture is added to 50 g of goose fat and mixed thoroughly. Apply the ointment to the skin before going to bed. Therapy lasts at least 14 days.
Neurodermatitis can be treated with infusions and decoctions for oral administration with the permission of a specialist and in the absence of contraindications and negative reactions from the stomach and intestines:
- Dry herbs of elecampane, calendula, coltsfoot, yarrow and blueberries are mixed in equal proportions. The collection is poured with boiling water: 450 ml of water for 2 tablespoons of raw materials. Leave in the thermos for 2 hours. Strain and drink 50-70 ml in the morning and before bedtime.
- Pour crushed dry grass of plantain, coltsfoot, and elecampane into a thermos, taking 30 g of each component. Pour 1 liter of boiling water and leave to steep overnight. You should drink 1 tablespoon three times a day for one week.
Before using any drug formulation, you should consult an experienced dermatologist. Inadequate treatment can cause a severe allergic reaction.
Diet
When creating a menu for every day, it is important to first remove from the diet foods that can cause an allergic reaction and introduce dishes rich in vitamins and minerals. Doctors strongly recommend that you stop consuming animal fats and replace them with vegetable fats . The most useful products are recognized:
- poultry and rabbit meat,
- lean beef and veal,
- skim cheese,
- fresh vegetables,
- fruits (green apples, bananas, pears),
- fermented milk products, provided that the patient is not allergic to milk.
It is necessary to give up berries, eggs, honey, citrus fruits, seafood, eliminating all possible allergens from the diet. An important condition is compliance with the diet. Each meal should be taken at the same time.
A full menu will help restore energy balance, activate the digestive tract, and provide the required amount of vitamins.
This guarantees the rapid restoration of damaged tissues and the full functioning of the body’s defense system.
Prevention
A number of preventive measures will help to avoid the re-development of neurodermatitis, including:
- regular walks in the fresh air,
- proper nutrition,
- giving up bad habits and a healthy lifestyle,
- you should avoid stressful situations, exercise regularly,
- take care of your skin, following hygiene standards and the recommendations of a dermatologist.
It is important to completely eliminate all possible contacts with identified allergens.
Attention!
The site administration advises you not to self-medicate, and in any controversial situations, consult a doctor.
Source: https://fr-dc.ru/kozhnye-zabolevaniya/simptomy-prichiny-i-lechenie-nejrodermita-na-golove-i-licze
What is not recommended to do?
Neurodermatitis is a chronic disease that can be triggered by numerous factors.
Patients with this diagnosis need to constantly monitor their lifestyle and diet. Ignoring the symptoms of the disease or self-medicating for complications is unacceptable. Any wrong actions can cause negative consequences, which will be difficult to get rid of.
For neurodermatitis it is not recommended:
- use questionable traditional medicine recipes;
- self-medicate for complications of the disease;
- violate the diet;
- allow contact with allergens;
- neglect preventive measures.
Drug therapy for neurodermatitis
If signs of neurodermatitis appear, treatment should be started immediately. It is carried out comprehensively using the following drugs:
- Antiallergic drugs. There are drugs of the first generation (Chlopyramine, Chlorpheniramine, Promethazine), second (Claritin, Zirtec) and third generation (Fexadin, Xizal, Aleron). The safest are third-generation antihistamines; they have a longer effect and are not addictive.
- Glucocorticoids. Used in severe cases.
- Vitamin complexes. The composition must include vitamins A, C, B.
- Enzyme preparations. Used if the patient has digestive disorders. The most commonly prescribed drugs are Festal, Pancreatin, and Mezim.
- Probiotics. Helps get rid of intestinal dysbiosis.
- Hepatoprotectors. Prescribed if long-term treatment has led to disturbances in the liver. The most popular hepatoprotectors are “Karsil”, “Essentiale”.
Therapy at all stages is controlled by a dermatologist. In acute cases, the patient is given intravenous calcium gluconate and sodium thiosulfate.
To speed up recovery, you need to use boron, tannin lotions, ichthyol pastes, and long-acting corticosteroid ointments.

Karsil effectively restores liver function
Possible complications
If you follow the recommendations of specialists, the prognosis for neurodermatitis is favorable in most cases. The main rule that patients must follow is the exclusion of factors that can provoke an outbreak of the disease. If the course of treatment is violated or the symptoms of neurodermatitis are ignored, serious complications can occur.
- Kaposi's eczema;
- chronic furunculosis;
- bleeding eczema;
- the addition of a secondary infection to a skin rash;
- formation of ulcers on the skin.
Diagnosis of the disease
Diagnosis of the disease is carried out using a visual examination. A specialist examines what the rash looks like. To clarify the diagnosis, the doctor prescribes an additional examination.
To determine the allergen, you will need to undergo examination by an allergist. The doctor will do skin tests to look for factors that cause an allergic reaction.
Using a blood test, a specialist will determine the level of ESR; in neurodermatitis, it is lower. Information about the number of lymphocytes and eosinophils in the blood is important. With this disease, their level is exceeded.
The following studies can be performed as additional diagnostic procedures:
- Ultrasound of the skin and subcutaneous tissue;
- skin biopsy;
- nail examination.
Additional diagnostics are prescribed in order not to confuse the disease with other diseases that have similar symptoms:
- chronic eczema;
- lichen planus;
- nodular prurigo.
To conduct a differential diagnosis, the nature of the rash is studied. The treatment and diagnosis of neurodermatitis is carried out by a dermatologist and an allergist.
Preventive measures
The main preventive measure for a tendency to neurodermatitis is the elimination of factors that can provoke an exacerbation of the disease. Experts recommend paying special attention to your diet. Excessive consumption of allergenic foods can cause skin rashes even if you have good immunity.
Preventive measures for neurodermatitis are the following recommendations:
- exclusion from the diet of foods that can cause allergies (or minimal consumption);
- timely treatment of diseases of the endocrine system;
- avoiding excessive physical activity;
- elimination of malfunctions in the digestive system;
- eliminating the lack of vitamins in the body;
- maintaining immunity with special medications;
- prevention of nervous system diseases;
- adequate sleep and nutrition.
Causes of the disease
There are 3 common causes of the disease:
- Pathology of the endocrine system.
- Nervous system disorder.
- Digestive disorders.
The disease can appear as a result of mental and physical stress. Negative emotions and stress increase the risk of developing the disease. Allergic factors play an important role.
Allergens can provoke an exacerbation of the disease:
- animal hair;
- feather filling for pillows and blankets;
- cosmetics and perfumes;
- Food;
- medications;
- plants and plant pollen.
In addition, it has been proven that neurodermatitis can be inherited.
This disease is of a psychosomatic nature. The psychosomatics of neurodermatitis are characterized by difficulties and conflicts associated with the psychological factor. The disease develops under the influence of strong emotions.
Neurodermatitis and its causes are not fully understood. It is not always possible to say with certain accuracy what exactly influenced the development of the disease. The causes of neurodermatitis are being studied by scientists to this day.











