Planning your pregnancy in advance
A woman suffering from allergic reactions should ideally plan the birth of her child in advance. This means that she must come to the gynecologist and report her desire to have a child and a history of an allergic disease.
The doctor, in turn, sends the woman for tests that will help identify the allergen and the state of the immune system. Based on the test results, the woman is prepared for pregnancy.
The doctor may prescribe a course of medications or describe in detail how to eliminate a food or household allergen and what preventive measures will help reduce the likelihood of the body developing a response to the introduction of a foreign protein.
The preventive measures taken will eliminate or reduce the likelihood of developing the disease, so a woman is more likely to avoid developing allergies during pregnancy.
Allergies during pregnancy, developmental features
According to statistics, about 30% of pregnant women are susceptible to allergies. And most expectant mothers have had this type of disease in the past, that is, before conception.
Patients from this category know the symptoms of the pathology and the factors that provoke it. Pregnancy is considered a specific catalyst, under the influence of which exacerbations of allergies occur, its course becomes more severe, or pathology occurs for the first time.
The main reason for this is the increased load on the organs of the immune system, as a result of which the body can react inadequately to any irritant.
The most common allergies during pregnancy are:
- Household dust;
- Microparticles of flowering plants;
- Pet proteins;
- Food products with chemical additives;
- Medicines;
- Solar radiation;
- Components of cosmetics and perfumery;
- Low temperatures.

The risk of developing allergies increases if a pregnant woman’s body is exposed to a number of provoking factors:
- Prolonged stress;
- Uncontrolled use of medications;
- Decreased immune defense;
- Constant use of household chemicals;
- Excessive passion for cosmetics;
- Wearing synthetic clothing, especially underwear;
- Failure to comply with the rational diet of the expectant mother;
- Abuse of foods rich in allergens;
- Poor environmental conditions in the place of residence;
- Work in hazardous production.
The more disease-provoking factors act on a woman’s body, the higher the likelihood of unwanted allergic reactions.
Types of allergies in pregnant women
Doctors most often diagnose expectant mothers with several allergenic diseases:
- ALLERGIC FORM OF RHINITIS. The main manifestations are abundant formation of mucous secretion, itching of the nasal passages, and paroxysmal sneezing. An exacerbation can be provoked by inhalation of house dust and particles of vital activity of pets, and pollen during the flowering season of plants. The cause of allergorinitis during pregnancy can also be toxicosis that occurs in some women;
- CONJUNCTIVITIS. Uncontrolled lacrimation, hyperemia of the sclera and conjunctiva, itching, and photophobia are noted. Usually, pregnant women develop rhinoconjunctivitis simultaneously. The causes of eye inflammation are caused by the same provoking factors as in allergic rhinitis. If conjunctivitis occurs separately, then the influence of cosmetics on the eyes should be excluded, read the article - allergies to cosmetics;
- HURTIC WITH DERMATITIS. Visually, urticaria resembles a burn resulting from contact with nettles. Blisters in a pregnant woman can be localized either to a specific area or spread throughout the body. Small pinpoint rashes with swelling and localized redness of the body are also characteristic. Skin pathological changes occur with severe itching, which adversely affects well-being. A localized form of urticaria occurs at the site of skin contact with an allergen, for example, on the face when using low-quality cosmetics;
- Quincke's edema. Increasing swelling is clearly visible in the eyelids and lips. The most dangerous thing is if the swelling moves to the oral area, first the tongue begins to swell, then the tissues of the larynx and trachea are involved in the pathological process. As a result, breathing becomes difficult, and in severe cases, suffocation occurs. In some cases, Quincke's edema also affects joint tissues - pain appears in the joints of the arms and legs, and there is limited mobility and swelling. With swelling of the digestive organs, the main symptoms of edema include pain in the abdomen, difficulty defecating and symptoms of intestinal obstruction;
- ANAPHYLACTIC SHOCK. One of the most dangerous manifestations of allergies. This is especially true for pregnant women. The first signs are clouding of consciousness, a sharp decrease in blood pressure, pale skin, fainting, developing within one to two hours after contact with a substance that provokes the body’s reaction. Most often, anaphylaxis occurs in response to exposure of the body to microparticles of plants, components of cosmetics and medications.
Signs and symptoms
The most common runny nose, which most people are accustomed to not paying attention to, is called rhinitis in medicine.
Rhinitis is an inflammation of the epithelial tissues of the nasal passages. As a rule, it is the main symptom of ARVI or allergies. Rhinitis in pregnant women is a fairly common occurrence. According to reviews, almost every second expectant mother experienced it. The main thing is to understand the causes of a runny nose.
There are the following types of rhinitis in pregnant women:
- hormonal (vasomotor) rhinitis – caused by changes in hormonal levels in a pregnant woman;
- Allergic rhinitis is the first manifestation of an allergic reaction.
- viral rhinitis - also called infectious, manifests itself as a symptom of the initial stage of ARVI.
Depending on the type of runny nose, the symptoms may vary slightly. Let's look at how rhinitis manifests itself during pregnancy:
- Rhinitis in pregnant women always manifests itself as a symptom such as swelling of the nasal airways, this sensation is especially intensified when lying on your back or during physical activity;
- Nasal congestion can lead to a decreased sense of smell, decreased appetite, sleep disturbances and, as a result, worsening mood;
- Nasal congestion may become more noticeable during pregnancy due to a deviated nasal septum.

Got a runny nose
Rhinitis in pregnant women can be distinguished from a common cold or allergy by the absence of the following symptoms:
- nasal discharge, coughing and sneezing are most often a sign of viral or allergic rhinitis;
- itching in the nasal passage, redness of the skin around the nose, watery eyes are constant symptoms of allergies;
- temperature indicates the occurrence of an inflammatory process, and is also the main sign of infection.
The effect of allergies on the fetus during pregnancy
If allergic reactions occur, women expecting a child should not worry that the disease will negatively affect the formation of internal organs in the fetus and the overall development of the child.
The only danger is that a predisposition to allergies can be inherited. If mom is sick, then this probability is 50%, if dad is sick - up to 20%. If both parents are allergic, then the risk of their children becoming frequent patients of an allergist reaches 70%.
During pregnancy, it is not the allergy itself that is dangerous, but what is used to treat it. If before conception a woman could, without hesitation, purchase any antihistamine and with its help successfully cope with the symptoms of the disease, then after fertilization such an approach to treatment is strictly prohibited.

Many antiallergic medications contain teratogenic components, and how they affect the health of the fetus is unknown. Some drugs disrupt the blood supply to the placenta, which leads to fetal hypoxia and insufficient supply of microelements and vitamins, and these factors are the root cause of developmental abnormalities.
Your doctor should tell you what you can do about allergies during pregnancy, and you should fully listen to his advice and recommendations on the use of antihistamines.
The table below describes the features of possible changes in the fetus with the development of an intolerance reaction in the expectant mother.
| Periods of pregnancy | The influence of a woman’s allergic reactions on the fetus |
| 1st trimester | In the first trimester, the formation of the placenta is just beginning, so there is no complete protection of the embryo. The pathogenetic influence of medications can negatively affect the development of future systems and organs, leading to abnormalities in their development and the death of the fetus. |
| 2nd trimester | The placenta actively performs its protective function, due to which the components of the medications taken by the mother have practically no effect on the unborn child. But this applies only to those drugs that are not contraindicated by their manufacturers during pregnancy. |
| 3rd trimester | Provoking factors and antiallergic drugs do not have access to the fetus. But the woman’s poor health can have a negative impact on the child’s condition, especially with regard to complicated forms of allergic reactions. |
Despite the absence of an immediate danger of an allergy to the fetus, the need for treatment of diseases cannot be underestimated.
The mildest, but persistent allergic rhinitis can provoke an asthmatic attack and anaphylaxis, in which breathing is impaired. That is, the woman experiences a lack of oxygen, and the baby suffers from hypoxia along with her.
Constant fatigue with weakness, discomfort, cough, skin irritation and sleep disturbances that appear when a woman has allergies also negatively affect the condition of the fetus.
Possible complications
The risk of developing complications from allergic rhinitis poses the greatest danger to the fetus in the 1st trimester, when the need for drug treatment entails the threat of intoxication. During this period, the best decision would be to refuse medications and alleviate the patient’s condition with general measures and folk remedies.
However, the addition of a bacterial infection may leave the expectant mother with no choice - after all, in this case there is a risk of developing a number of inflammatory processes in the respiratory organs, which without proper treatment can take a very severe form.
All efforts of a pregnant woman during this period should be aimed at ensuring normal nasal breathing. Otherwise, fetal hypoxia may occur, and, as a result, developmental abnormalities and even miscarriage. Using medications without consulting a doctor is no less dangerous.
In subsequent periods, with the formation of the placenta, the risk of intoxication is significantly reduced, but the threat of hypoxia still remains, as well as the negative impact on the pregnant woman’s body:
- Nosebleeds caused by thinning of the nasal mucosa;
- Deterioration in odor recognition;
- Acute forms of sinusitis;
- Overgrowth of the mucous membrane (polyps);
- Tonsillitis during pregnancy, pharyngitis, laryngitis (with the addition of a bacterial form).
If a vasomotor runny nose in a pregnant woman is accompanied by severe congestion, this can lead to an increase in pressure and interruptions in the functioning of the heart. If the expectant mother begins to breathe through her mouth, the risk of infection entering the body increases. If left untreated, a runny nose is accompanied by headache, dry mucous membranes, and weakness.
Prevention of rhinitis
A woman carrying a child must monitor her health many times more carefully than she did before. You need to walk more in the fresh air, but you need to dress in such a way as not to freeze, but also not to overheat.
The room must be ventilated, cleaned and moistened, which helps to avoid drying out of the mucous membranes, the appearance of itching and crusts on the nose.
During pregnancy, it is better for a woman not to attend events where a lot of people are present, not to contact sick people, give up coffee, but drink more fluids so that the body does not become dehydrated.
If you have a runny nose, you should visit a doctor rather than treating the symptoms yourself. Simple prevention will help a woman protect her health and give birth to a healthy baby, which she is looking forward to.
You can find out more about the use of Pinosol spray in the treatment of rhinitis here.
Allergy symptoms during pregnancy
As already mentioned, most often when carrying a child, a woman is worried about allergic rhinitis or rhinoconjunctivitis. In second place in terms of frequency of occurrence are skin reactions. The diseases listed above occur in the same way as in the absence of pregnancy, but expectant mothers need to know a few facts:
- Swelling of the nose, causing congestion and difficulty breathing while expecting a baby, may indicate not only an allergy, but also high blood pressure and eclampsia. Both conditions are extremely dangerous during pregnancy, so they must either be excluded or confirmed with subsequent treatment;
- Red spots on the abdomen and severe itching of the skin may indicate hepatosis - a disorder of the liver. Some forms of hepatosis in pregnant women require immediate treatment.
POPULAR WITH READERS: Yeast allergy, causes of pathology, methods of treatment

Giant urticaria, the spread of itchy blisters throughout the body, is also dangerous for pregnant women. It develops rapidly, the disease greatly worsens general health, causes severe itching, and increases nervous excitement.
Symptoms of an allergic type of disease
The following symptoms of allergic rhinitis during pregnancy include:
- itching in the nose;
- sneeze;
- clear, watery nasal discharge;
- difficulty breathing, characteristic of severe cases of allergic rhinitis;
- Nasal congestion worsening at night.
The appearance changes with exacerbation of allergic rhinitis. Swelling of the face appears, the patient breathes through her mouth, often red eyes, lacrimation. Allergic rhinitis is also accompanied by dark circles under the eyes.
There are severe, moderate and mild degrees of allergic disease. If the symptoms do not interfere with sleep and do not reduce performance, this is a mild degree; if daily activity decreases moderately, this is a moderate degree of severity, and if the symptoms are severe, this is a severe degree of the disease.
In the 1st trimester of pregnancy, rhinitis can be quite dangerous, especially in the early stages of pregnancy. It is not so much a runny nose that is dangerous as the disease that provoked it. If this is a viral disease, then the virus can enter the uterus with the blood and lead to abortion.
Diseases that cause a runny nose can also cause abnormal formation and development of the fetus, which occurs in the early stages: during the first eight weeks. A runny nose makes it difficult for the expectant mother to breathe, which reduces the amount of oxygen that enters her body and the fetus. This fact is relevant throughout the entire period of pregnancy, but most of all in the early stages.
This disease can be treated in the early stages by rinsing the nasal cavity with saline solution. To make such a solution, you need to dissolve a teaspoon of salt in half a liter of boiled water. Treatment of the disease can be carried out using “star” balm, which needs to be lubricated on the forehead, temples and bridge of the nose, but in moderation.
Also, rhinitis in pregnant women can be treated with a solution of menthol and vegetable oil; it should be instilled into the nose. Hot hand baths will help relieve congestion. In the early stages of pregnancy, you can also treat a runny nose by instilling fresh beetroot juice diluted with boiled water into the nostrils. Treatment can also be carried out with hot tea with honey, but honey is a strong allergen and can be consumed in limited quantities. Warming the nose with a bag of warm salt or a warm boiled egg will help treat rhinitis in pregnant women.
Vasoconstrictor drops can be used to treat a runny nose only in extreme cases, and not only in the early stages of pregnancy. Treatment is best done with drops for infants or newborns. But they can only be used for no longer than 3 days. Such products should be instilled into the nostrils before bedtime once a day.
The article is presented for informational purposes. Treatment should only be prescribed by a doctor!
- Why is dust dangerous?
- Cost of MRI of the spine
- Causes of skin diseases
What to do if symptoms appear
An allergic reaction may be the result of intolerance to a new type of food or a chemical contained in household chemicals, perfumes, and cosmetics.
With minor symptoms - a limited area of rash, skin irritation, sneezing, drug treatment may not be required. But this applies only to those situations where the source of the allergen has been independently identified and further contact with it is excluded.
Usually, after these conditions are met, the symptoms of intolerance disappear on their own within two to three days.
But if the allergy existed before pregnancy and reappeared after conception, then you should adhere to the following recommendations:
- Make an appointment with an allergist. It is necessary to establish the main allergen, which is possible only after diagnosis - the doctor prescribes a blood test for allergies and skin tests;
- Start treatment. Tablets are selected only by a doctor, since not all antihistamines are safe for the fetus and the woman’s body;
- Avoid repeated contacts with already established allergens;
- Stick to a hypoallergenic diet. Citrus fruits, nuts, and chocolate should be excluded from the diet;
- Use only those cosmetics that contain natural ingredients;
- Minimize the use of household chemicals. When cleaning, wear thick gloves and a mask.
It is imperative to maintain cleanliness and comfortable humidity in the house, ventilate more often or use air purifiers. It is advisable to avoid using air fresheners with strong scents.
Causes
Why does allergic rhinitis occur during pregnancy? There could be many reasons. But the main one is an allergic reaction to various irritants in the environment. Most often this is:
- Flower pollen;
- Poplar fluff;
- Tobacco smoke;
- Bleach and other detergents;
- Volatile substances from deodorants and air fresheners;
- Essential oils of citrus fruits;
- Wool of cats, dogs and other fauna;
- Feathers and down of birds.
Due to changes in hormonal levels, the level of hormones in the blood increases. Estrogen, progesterone and hormones responsible for growth are responsible for increasing the sensitivity of a pregnant woman's body to various allergens.
Another common cause of allergic rhinitis during pregnancy is the bites of various insects. For example: mosquitoes, wasps, bees, ticks, bedbugs, lice or fleas.
Here are the main causes of a runny nose:
- Bacteria. Most often, a bacterial infection is associated with a sluggish viral infection. Against the background of the disease, local immunity decreases, which promotes the proliferation of pathogenic microorganisms such as streptococci or staphylococci. If a clear liquid is released from the nose due to viruses, then at the time of bacterial infection the mucus becomes thick, green or yellowish.
- Allergic runny nose. May occur in spring or summer. Most often it occurs during flowering of plants, when their pollen floats in the air and settles on the nasal mucosa, causing irritation. As a result, it swells and secretes clear mucus; along with rhinitis, redness of the eyes and watery eyes may occur.
- Viruses. Viral infections are the most common cause of rhinitis. Viral runny noses occur mainly in the autumn-winter period; it is at this time that all respiratory diseases peak. Often the virus develops not only with a runny nose, but also with fever and general malaise.
Fortunately, there are now medications that can help pregnant women cope with all manifestations of a runny nose.
Even in women who are not predisposed to allergies, during pregnancy there are changes in hormonal levels and a decrease in the overall level of immunity. It would seem that ordinary smells or foods can cause an unusual reaction, the main manifestation of which will be nasal congestion and a severe runny nose.
The mechanism of allergy occurrence still remains unclear. The rapid development of innovative technologies has led to equally rapid changes in the environment - air, water, food. The human body often does not have time to adapt to such global changes; the immune system cannot recognize the nature of the irritant entering the body.
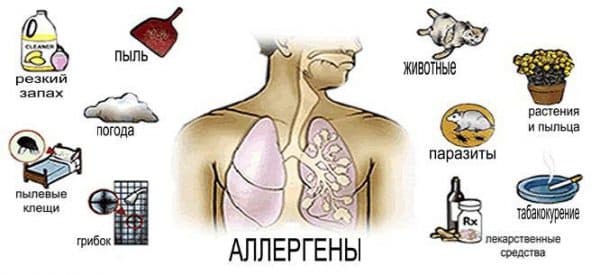
Popular allergens
The most common causes of a runny nose are the following allergens:
- Pollen of plants, cereals and cereal grasses;
- House dust, animal hair;
- Some food products;
- Smells of household chemicals, perfumes, cosmetics;
- Medications;
- Beekeeping products;
- The smells of building materials, mastics, polishes, new furniture.
Pregnancy makes a woman especially vulnerable, so the risk of allergies increases under the influence of the following factors:
- Frequent stress;
- Increased mental lability;
- Exposure to cold air;
- The presence of spicy foods in the diet.
The cause of allergic rhinitis in pregnant women is a foreign substance, an allergen. These usually include:
- dust mites;
- plant pollen (weeds);
- bites of insects and other animals (mosquitoes, bees);
- bacteria, viruses (staphylococci, E. coli);
- fungi (yeast, mold);
- products (vegetables, fruits, nuts);
- chemical compounds (medicines, household products);
- dandruff, saliva, pet hair (cats, dogs).
Why do women suffer more from allergic rhinitis during pregnancy?
Such changes can be explained by several factors:
- genetic predisposition;
- restructuring of the body’s immune system, as well as all organs in general;
- hormonal surge against the background of an increase in the concentration of estrogen, progesterone, human chorionic gonadotropic hormone.
Although changes in hormone production occur during pregnancy, not every pregnant woman suffers from rhinitis, although many do.
Contribute to the appearance of vasomotor rhinitis:
- deviation in the structure of the nasal cavity;
- bad ecology;
- tobacco smoke;
- unfavorable weather.
Unpleasant sensations in the expectant mother sometimes begin after eating spicy food with preservatives and flavorings, due to inhalation of cold air, the presence of a pungent odor.
During fetal development, the amount of estrogen increases significantly. This hormone acts on the nervous system, and it sends signals to the vessels, which negatively affects the condition of their walls, and the passages in the nose narrow, and the mucous membrane swells.
We suggest you read: Can a pregnant woman take lozenges from Doctor Mom?
Read this article on how to treat bacterial rhinitis.
Diagnostics
The diagnosis of allergies in pregnant women is made based on:
- Determining the history of pathology;
- Blood tests showing the total titer of immunoglobulin E;
- Tests that determine antibodies to certain allergens;
- Skin tests.

If necessary, the allergist sends the patient for a consultation with a gastroenterologist, dermatologist, or neurologist.
Features of treatment of various forms of disease manifestation
Any pregnant woman has a several-fold increased risk of developing allergies and this should not be forgotten. Preventive measures will help reduce the likelihood of unwanted immune system reactions.
It is necessary to minimize contact with synthetic detergents, cosmetics, perfumes, and limit allergenic foods in the diet.
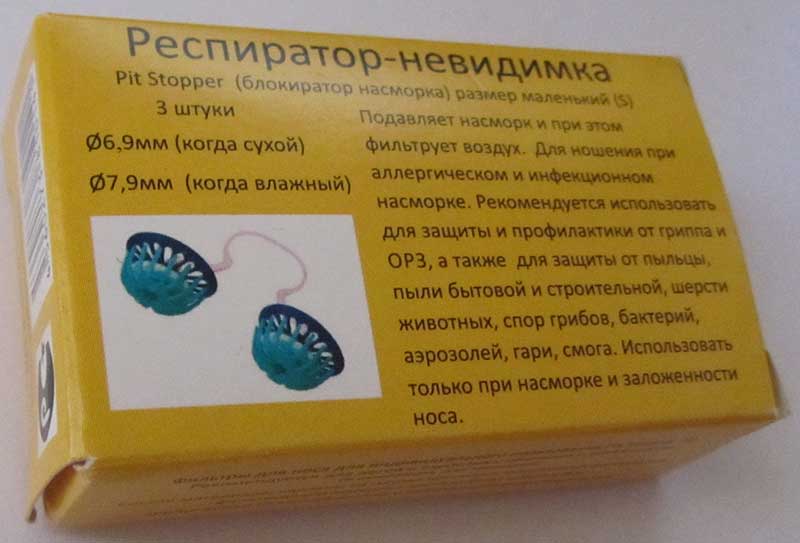
If you have seasonal pollen intolerance, you need to put on a mask and glasses before going outside, and after walking, thoroughly wash your hands and face, clear your nose, change your street clothes to clean ones, you can use special nose filters.
The likelihood of allergies is greatly reduced if a pregnant woman does not experience negative stressful situations, follows a work-rest schedule, and gets enough sleep.
If you have primary signs of the disease, you should immediately consult a doctor; an experienced allergist will tell you what to do and what medications you can use.
Treatment of allergorinitis
The best medications for allergic rhinitis for women in all trimesters of pregnancy are those made using natural ingredients. These are Aqua Maris, Aqualor, Dolphin.

They are used to cleanse the nasal cavities; rinsing helps remove allergens, moisturizes the mucous membrane and makes breathing easier. The listed medications do not have any effect on the body of a developing child.
Local treatment is not prohibited during pregnancy:
- PINE SCRATCHER. The drops are created using natural ingredients - mint and eucalyptus oils. Instillation of Pinosol reduces swelling of the mucous membrane, softens it and destroys pathogenic microorganisms;
- SPRAY PREVALIN. Spraying the medicine creates a protective film on the mucous membranes of the nasal passages, which prevents the action of allergens;
- SALIN. The basis of the medicine is sodium chloride. The main action is to cleanse the nose of possible irritants.
Treatment of conjunctivitis
During pregnancy, you can use Inox drops; they contain natural ingredients. Medicines reduce irritation and itching, remove redness.
Skin manifestations
To eliminate skin rashes, peeling and itching, expectant mothers are allowed to use zinc ointment. It relieves inflammatory reactions well and dries out the skin. The drug Tsindol, created on the basis of zinc oxide, is also safe.

To eliminate skin allergies in a pregnant woman, creams based on chamomile, calendula flowers, and celandine can be used.
Peeling is well removed by Bepanten cream and Psilo-balm. Physiogel helps with atopic dermatitis; under its influence, the skin softens and moisturizes, and cracks heal faster. A homeopathic remedy, Fleming's ointment, helps a lot.
Drug and food allergies
The well-being of a pregnant woman improves if, in the event of the development of a food or drug allergy, the body is cleansed. This can be achieved by taking enterosorbents - Enterosgel, Lactofiltrum for several days.
In case of severe itching and skin irritation, you can drink Activated Carbon once in a dosage - for every 10 kilograms of weight you need to take one tablet. Drinking clean water in large quantities also helps cleanse the body, but pregnant women can drink a lot only if there is no edema.
Features of the use of drops depending on the trimester
When choosing drops for a runny nose during pregnancy, you need to consider the following:
- type of rhinitis;
- gestational age;
- the presence of contraindications to the start of treatment;
- tolerability of therapy.
A runny nose in pregnant women can be caused by various reasons, depending on which you need to select medications. Types of rhinitis during pregnancy can be:
- Infectious. Most often, it is caused by a viral infection in the body, so antiviral drops are prescribed for it. Vasoconstrictors are used to relieve nasal congestion. When a bacterial infection occurs, the use of antibiotics is recommended.
- Allergic. When it develops, antiallergic and hormonal drops are recommended.
- Rhinitis in pregnant women. It occurs due to changes in hormonal levels during gestation and goes away only after childbirth. Hormonal and moisturizing agents are used to treat it.
It is very important to take into account the gestational age, since the effect of medications will differ depending on the trimester. First trimester
During it, the child’s organs are formed, and doctors do not recommend using drugs that contain synthetic chemicals
First trimester. During it, the child’s organs are formed, and doctors do not recommend using drugs that contain synthetic chemicals.
Prohibited drugs can cause spontaneous abortion and the development of fetal pathologies. During this period, moisturizers based on sea water are allowed.
If signs of infectious rhinitis appear, you can use immunostimulating drops, for example, Derinat, which is also recommended for the prevention of ARVI.
Recommended video:
In addition, antiseptic medications are allowed with it, for example, Okomistin. In the first trimester, you can use homeopathic drops and herbal preparations, such as Pinosol.
To treat allergic rhinitis and rhinitis in pregnant women, many hormonal agents can be used, since they are almost not absorbed into the general bloodstream and do not cause systemic adverse reactions.
For example, the drug Nasonex is allowed during this period. Also, after assessing the benefits for the mother and harm to the fetus, antiallergic medications based on cromoglycic acid, for example, Cromoglin, can be used in the first trimester.
Second and third trimester. During this period, all drugs that can be used in the first three months of pregnancy are allowed.
Also, at this period, you can take some medications that are contraindicated in the first trimester, since during this period the main organs of the fetus have already formed.
For example, starting from week 14, for allergic and vasomotor rhinitis, Nasobek can be used.
It should also be taken into account that a woman may have concomitant diseases that are a contraindication to their use; in addition, medications cause undesirable reactions.
Treatment of allergies during pregnancy
Anti-allergy medications during pregnancy should be prescribed by a doctor. A woman expecting a child should definitely notify her doctor about the symptoms of the disease. It is prohibited to take antihistamines on your own; they are especially dangerous before 12 weeks of pregnancy.
The doctor, taking into account the patient’s condition, test data and the risk of possible complications, selects drug therapy. Antiallergic drugs in the 1st trimester of pregnancy are prescribed in cases where the symptoms are severe and cannot be eliminated using safe methods.
Antihistamines prescribed at different stages of pregnancy
Allergies that develop in the first trimester of pregnancy can be treated only with natural-based drugs without the risk of complications for the embryo and mother. Almost all of them are listed above. Therapy can be supplemented with homeopathic remedies, as well as such as Euphorbium, Rinitol Edas 131.

In the 2nd trimester of pregnancy, medical options for treating allergies in expectant mothers expand. The fetus is already protected from external irritants by the placenta and most of the internal systems are formed, so medications taken by the mother cannot have a significant negative effect.
An allergist may prescribe:
- DIAZOLIN. A first generation antihistamine containing Mebhydrolin as an active substance. The drug copes well with the symptoms of allergorinitis, urticaria, hay fever, and drug intolerance. During pregnancy, it is advisable to take Diazolin in a short course for up to 5 weeks. The medicine is safer if it is used in the last weeks of the second trimester. The dosage is selected by the doctor; side effects include drowsiness;
- PHENIRAMINE. In normal practice, allergists rarely use this drug. Pheniramine is good at eliminating swelling and nasal congestion, so it is often taken for colds. During pregnancy, the medicine can be effective in eliminating rhinitis, conjunctivitis, and itching of the skin. Side effects include lethargy, dry mucous membranes, and drowsiness;
- SUPRASTIN. The drug can be used for rapidly developing symptoms of an acute allergic reaction. Suprastin begins to act in 20-30 minutes, with its help you can stop the progression of the disease. But for further treatment of allergies, the doctor must select other drugs;
- ASCORBIC ACID AND VITAMIN B12. They are considered natural antihistamines and help reduce the severity of dermatoses and bronchial asthma. Vitamins improve and strengthen the functioning of the immune system;
- HORMONES. The doctor may prescribe Prednisolone, Dexamethasone. Allergists prescribe glucocorticosteroids during pregnancy when it is necessary to relieve rapidly developing symptoms of pathology. The dosage and duration of their use are determined by the doctor. Hormonal ointment for allergies during pregnancy can only be used in short courses.
In the third trimester it is allowed to use:
- FENISTIL. Available in the form of gel, emulsion, drops and capsules. In the 3rd trimester, it is best to use Fenistil drops; the drug is prescribed in a short course of up to 7-10 days. The gel and emulsion are used topically, so they are not dangerous for the child, but they can only be applied to a small area of the skin;
- ZIRTEK. Dosage forms – drops, tablets. The drug is effective in the treatment of rhinitis, hay fever, dermatoses with rashes and itching, and urticaria. You can take both drops and tablets. Zyrtec, here are the complete instructions for the drug, belongs to the second generation antihistamines, so there are practically no adverse reactions when taking it. Treatment with the drug is continued until allergy symptoms disappear;
- FEXADINE. A drug of the third generation of antihistamines. The antiallergic effect develops quickly; the medicine should be taken once a day. A short course of taking Fexadine is recommended for pregnant women. Trade names: Telfast, Telfadin, Allegra.
- TAVEGIL. It is a first generation antihistamine. The medicine effectively eliminates swelling and nasal congestion and itchy skin. Tablets are prescribed twice a day, but the drug is contraindicated if the woman has a history of bronchial asthma. The most common side effects of Tavegil are headache, decreased blood pressure, and increased fatigue. Prescribed to pregnant patients only if absolutely necessary;
- LORATADINE. Available in the form of syrup and drops. Can be used from the second trimester of pregnancy. Loratadine helps with hay fever, urticaria, Quincke's edema, conjunctivitis and nasal congestion. Complete analogues of Claritin and Lomilan.
IMPORTANT: Any medicine from the antihistamine group, even the new generation, should only be prescribed to a woman, regardless of the trimester of pregnancy, by a doctor. It must be remembered that even short-term treatment with antihistamines does not guarantee that it will be one hundred percent safe for the child.
Barrier drugs
This term refers to a separate group of nasal sprays that prevent allergens from reaching the nasal mucous membranes.
POPULAR WITH READERS: What is autoallergy and can this disease be cured?
Spraying an aerosol allows you to create a protective layer in the nasal cavity, which serves as a barrier against irritants. Allergens do not enter the tissues, and thus an allergic reaction does not develop, that is, complexes of inflammatory mediators are not formed.
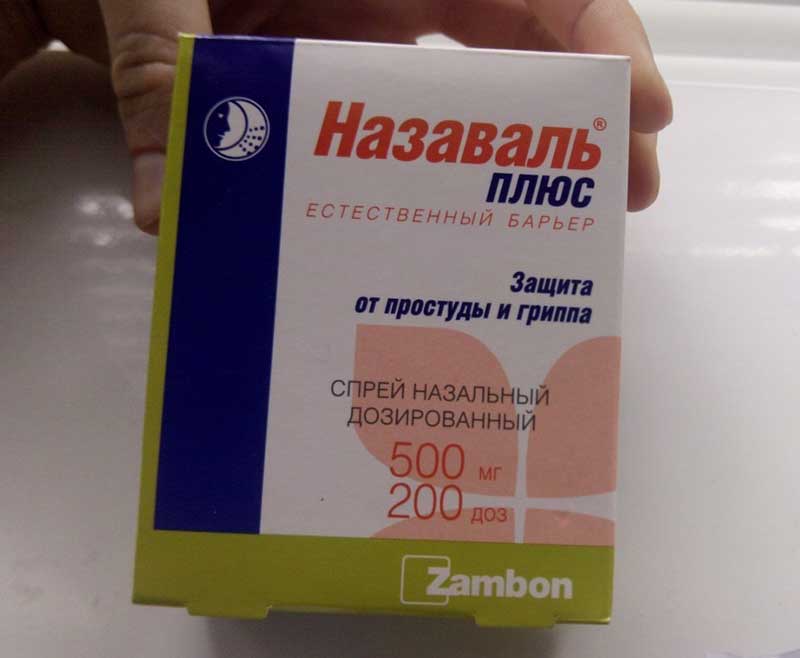
Currently, there are two barrier drugs - Prevalin and Nazaval, they have common and distinctive properties and nuances of use.

Prevalin
The drug contains natural oils and emulsifiers; when sprayed, they turn into a gel, which in the form of a thin film reliably covers the entire nasal mucosa.
Prevalin is effective as a means of preventing allergic rhinitis; the drug is suitable for pregnant women and for eliminating the first signs of runny nose allergenesis.
It is necessary to spray the product approximately 20 minutes before possible contact with the allergen - usually this is done before going outside during the flowering season of plants. The components of the aerosol do not enter the systemic bloodstream, therefore Prevalin is safe for both the pregnant woman and the fetus.
The barrier function of the drug is maintained for 5 hours after its spraying. The manufacturer recommends using the medicine every 4-6 hours, but after blowing your nose, the spray must be repeated, even if the specified time has not passed.
Prevalin can be used without restrictions. The only contraindication is increased sensitivity to the components of the spray. The effectiveness of the barrier function also depends on how accurately the steps of the instructions included with the medicine are followed.

Nazaval
The drug contains micronized cellulose and mint extract. If a pregnant woman has allergies, after spraying, a gel-like substance is formed on the mucous membranes, which performs protective functions.
Nazaval effectively protects against the penetration of house dust components, plant microparticles, animal epidermal scales, and fungal microorganisms.
It is recommended to spray 15 minutes before possible contact with the allergen. The barrier function is maintained for 6 – 8 hours.
The components of Nazaval do not enter the general bloodstream; during pregnancy it can be used at any stage.
Corticosteroids
Preparations with GCS are produced in the form of tablets, injections, creams and ointments. The mechanism of action of hormones is based on blocking Th-2 cytokines, under the influence of which allergic reactions develop.
Corticosteroids quickly and effectively eliminate swelling, irritation of the skin, nasal congestion and cough. However, GCS, such as Metypred, Dexamethasone, Prednisolone, significantly reduce resistance to infections, which can also negatively affect the development of the fetus.

Therefore, medications with hormones are prescribed to pregnant women as a last resort measure - when conventional antiallergic treatment does not give the desired result.
Useful video on how to properly rinse your nose at home
We advise you to read: acute respiratory infections during pregnancy, what is the danger for a woman and child
In a strict medical sense, rhinitis in pregnant women is chronic swelling of the nasal mucosa in a woman, leading to difficulty in nasal breathing and caused by hormonal changes in the body.

Actually, this disease differs from other types of rhinitis in its causes. For example, typical acute rhinitis (cold) is caused by a weakened immune system and increased activity of bacteria that are normally not pathogenic; viral rhinitis is caused by a viral infection; allergic rhinitis is caused by substances to which the patient is hypersensitive. That is, all typical rhinitis causes are external - hypothermia, infection, allergens. Rhinitis in pregnant women is caused by internal causes and does not depend on what kind of air the patient breathes and whether she becomes infected with something from others.
Obviously, rhinitis in pregnant women can also be caused by ordinary reasons - infection, allergies, hypothermia, dirty air. That is, if a pregnant woman becomes infected with ARVI, she will develop a runny nose, just like any other person. However, such a runny nose is not called pregnancy rhinitis in medical science, since it is simply a viral rhinitis that can equally occur in men and children. And rhinitis in pregnant women is a disease that can only develop in women during gestation and is caused by reasons that arise only when the woman’s body undergoes restructuring during fetal development.
Simply put, not every rhinitis during pregnancy is precisely rhinitis during pregnancy in the strict scientific understanding of the term. Moreover, the symptoms of rhinitis in pregnant women differ from the signs of typical runny nose.
What is prohibited for use
Almost all antihistamines for allergies during pregnancy are used only according to strict indications, but some of them are completely prohibited for use, these are:
- DIMEDROL. The drug increases the excitability of the muscular layer of the uterus, which can lead to its hypertonicity. As a result, spontaneous abortion develops in the early stages and premature birth in the later stages;
- PIPOLPHEN. The drug contains toxic substances that can lead to the death of the fetus in the womb;
- ASTEMIZOL. The mechanism of action is similar to Pipolfen;
- TERFENADINE. The medicine causes weight loss in the fetus.
Suprastin can only be used to relieve acute manifestations of allergic reactions.
How to cure cough in early pregnancy
To cure a cough faster, you need to turn your attention to time-tested folk recipes for treating coughs and colds in general.
Among these recipes there are effective and proven tips. Honey has always been one of the most popular ways to treat colds and coughs. Sticky, sweet and very healthy. Everyone in childhood drank milk with honey when they were sick, and to this day it remains one of the most popular recipes for a sore throat and cough. But you cannot treat a cough with honey in case of an allergic reaction to this product.
So, folk recipes:
- The simplest recipe is tea with honey. But it is better to choose herbal tea and drink it not scalding hot. You can eat honey as a bite, or use it to season tea instead of sugar.
- A recipe from my distant childhood - milk with honey. If possible, it is advisable to choose goat’s milk rather than cow’s milk. It is healthier, rich in vitamins and copes better with colds. If you can’t buy goat’s milk, then choose cow’s milk, but homemade. If you live in a metropolis and couldn’t find homemade milk, add a little butter to the milk and honey. This mixture will soften an irritated throat and the cough will subside a little, and honey will treat a cold.
- The best recipe with honey for coughs and colds in general is a combination of black radish juice with honey. This is the recipe our grandmothers used to treat themselves. The mixture tastes a little tart, but it helps well with a dry, tearing cough. And black radish contains a lot of vitamins.
- A combination of badger fat and honey. The mixture is, to put it mildly, unappetizing. However, if you take a spoonful of honey and a spoonful of badger fat every morning, even the most severe cough will be relieved.
It is impossible to treat a cough in the early stages of pregnancy using mustard plasters, you cannot use cups, and you cannot steam your feet. Many grandmothers advise you to eat more vitamin C, and everything will miraculously pass. No.
The most popular recipes from the Internet:
- tea with raspberries;
- onion syrup;
- tea with blackcurrant and plantain leaves;
- chew aloe, just a little, it tastes incredibly disgusting, but it helps;
- honey in combs on old foundation;
- aroma oils;
- figs with milk;
- onions with honey;
- horseradish juice;
- milk with sage;
- garlic with honey.
Unfortunately, effective folk recipes do not always taste good. The rule works: what is healthy is not tasty.
Traditional treatment
Folk remedies and methods for eliminating allergies during pregnancy should be selected as carefully as medications.
Particular care should be taken when using herbal medicines orally, since herbal preparations can either cause an allergic reaction themselves or provoke a worsening of an existing one.
Cough
In case of an allergic dry cough, the attack is well relieved by inhalation of mineral waters. Gas is first released from them.
Inhalation is carried out through a nebulizer, the procedure time is 5-10 minutes. You can use Borjomi, Narzan, Essentuki No. 17 or 4 as a solution. About an hour after the session, you can breathe over peach, eucalyptus, and olive oil.

Treatment of urticaria
Skin itching due to allergies in pregnant women is eliminated by wiping the rash with solutions of menthol or salicylic acid. An infusion of dill seeds and plantain leaves is effective in relieving irritation.
To prepare the infusion, you need to mix a tablespoon of these components and pour about a glass of boiling water. After an hour, the antipruritic infusion is ready; you should use it to wipe irritated areas throughout the day.
Allergic dermatitis
To reduce irritation, dryness and hyperemia of the skin in pregnant women, you can use:
- A decoction of chamomile, St. John's wort, calendula and sage flowers. The herbs are mixed together, 1 tablespoon is taken from the collection and brewed with half a liter of boiling water. Leave for an hour, after straining, use for rubbing and lotions. You can drink this decoction a third of a glass twice a day;
- Infusion of plantain, chamomile flowers and calendula inflorescences. The raw materials are mixed, then 4 tablespoons of the mixture are brewed with two glasses of boiling water and kept under the lid for one hour. The strained infusion is used for compresses and rubbing;
- Rosehip seed oil. Take a teaspoon per day orally, externally to wipe irritated areas of the skin;
- Decoction of oak bark. 100 grams of crushed herbs are boiled in a liter of water for 30 minutes, left for two hours. Oak decoction is especially effective if dermatitis is accompanied by the formation of weeping areas.

If the entire skin is irritated, you can take medicinal baths with the herbs listed above. Before taking a herbal bath, you need to take a shower, and after the procedure it is advisable to let your body dry naturally.
Allergic eczema
During pregnancy, you can cope with allergy symptoms by using:
- FRESH CABBAGE LEAF. The washed and slightly softened sheet is applied to the inflamed area and secured with a bandage. The dressing needs to be changed once a day;
- COMPRESSES FROM EGG WHITE AND CABBAGE LEAF. Three tablespoons of crushed leaf should be mixed with one beaten egg white. The composition is applied to the area with eczema in the form of a compress;
- HERBAL COLLECTION. Buckthorn, fennel, dandelion roots, watch leaf and chicory should be mixed in a ratio of 2:2:1:1:1. Then one tablespoon of the resulting mixture is poured with boiling water (one glass), heated over low heat for half an hour, cooled and filtered. You should take ¾ cup twice a day;
- A MIXTURE OF APPLE VINEGAR, RAW EGG AND WATER. Mix them in equal proportions and apply them like a compress;
- BIRCH JUICE. Fresh juice is used to wipe the skin.
Series
A fresh decoction of the string can be used for allergies both internally and externally. As a rub, the decoction has a calming effect - relieves itching, irritation, and hyperemia.
Tea from the series is suitable for internal use. Take a teaspoon of string for a glass of boiling water. The tea is prepared fresh every time. You can drink it for several years, but after every 20 weeks of treatment the body should be allowed to rest for 8-10 weeks.

Natural antihistamines
A number of natural substances of natural origin help cope with allergy symptoms during pregnancy. Naturally, they will not eliminate all manifestations of the disease, but they can significantly alleviate their course.
Such substances include:
- ASCORBIC ACID. Vitamin C is especially effective in its antiallergic properties in the treatment of runny nose and bronchospasm. The daily dose is from 1 to 3 grams. Reception begins with a small dose of 500 mg per day, then it is gradually increased;
- LINOLEIC ACID AND FISH OIL. Prevents the appearance of skin irritation and itching, rash, lacrimation and hyperemia of the sclera. The dosage is determined by age and characteristics of the body;
- VITAMIN B12. Reduces symptoms of dermatitis and asthma. 500 mg of vitamin B12 is needed per day, treatment should be continued for up to 4 weeks;
- ZINC PREPARATIONS. Reduces the risk of allergies to chemical components. Taken internally as part of vitamin-mineral complexes;
- OLIVE OIL. Considered a natural antihistamine. You can use olive oil for preparing dishes - porridges, salads.
Prevention
Every expectant mother should understand that in her condition the risk of allergic reactions is greatly increased. To avoid allergies during pregnancy, you must adhere to the following recommendations:
- EAT CORRECTLY AND RATIONALLY. The diet should contain as much natural food as possible. You need to exclude or minimize foods rich in allergens - chocolate, citrus fruits, strawberries. During pregnancy, it is not advisable to try exotic dishes, vegetables and fruits;
- FOLLOW A HEALTHY LIFESTYLE. Good rest, daily walks, and giving up bad habits help not only prevent allergies, but also have a positive effect on the child’s health;
- TAKE CARE OF YOUR BODY CORRECTLY. Pregnant women need to select cosmetics and body washes especially carefully. It is better to purchase hypoallergenic products with a minimum of fragrances and fragrances. It is imperative to maintain hygiene and it is advisable to refuse to wear clothes made of synthetic materials.
Women with a predisposition to allergic reactions even before pregnancy or in the initial stages of its development should visit an allergist.
The doctor will conduct an examination, assess the risk of developing allergies and recommend preventive measures and medications that can be taken when symptoms of the disease appear.
If you find an error, please select a piece of text and press Ctrl+Enter.











