An inflammatory pathological process that affects the alveoli and tissues of the respiratory organs is called allergic alveolitis. The development of the disease is facilitated by the penetration of allergens into the respiratory canals.
The insidiousness of the disease is that its primary symptoms are difficult to recognize. Seeing a doctor will help save the patient's life.
What it is? Types of pathology
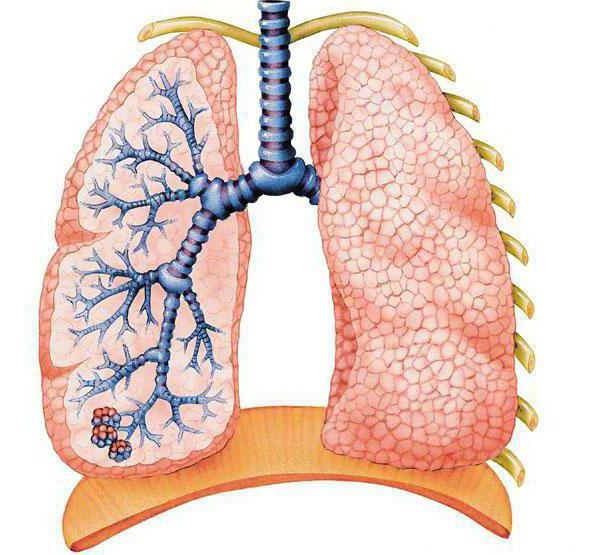
Pulmonary alveolitis is a diffuse inflammatory disease of the alveoli.
Alveoli are small sacs in the lungs, part of the lung tissue that fills with air. Normally, they are empty, and the doctor, listening to the lungs, should hear vesicular breathing. That is, it should be problem-free, without heavy sighs, whistles and wheezing. And wheezing just means that the alveoli are inflamed. Allergic alveolitis is also called inhalational pneumopathy. Alveolitis can have complications if the source of the allergy is not understood. But the disease goes away easily if the cause is eliminated.
All alveolites are divided into 3 types:
- fibrosing;
- allergic;
- toxic.
But we will consider in detail only one - exogenous allergic alveolitis, since questions about its treatment are more relevant. Treatment is carried out in the only way. It is necessary to reduce tissue inflammation with the help of medications that inhibit the body's immune defense. This is the only way to relieve shortness of breath and cough so that a person can breathe normally.
Prevention of alveolitis
Prevention of alveolitis involves following the rules for working with toxic substances and eliminating irritants that cause an allergic reaction. It is necessary to undergo regular examinations by a pulmonologist and rheumatologist. Prevention of alveolitis with the help of medications is not provided.
Author of the article:
Alekseeva Maria Yurievna |
Therapist Education: From 2010 to 2020 practicing physician at the therapeutic hospital of the central medical unit No. 21, the city of Elektrostal. Since 2020 he has been working at diagnostic center No. 3. Our authors
Diagnostics
Acute form
Exogenous allergic alveolitis of this type develops after massive introduction of an antigen in adults in an industrial environment, in children - at home or from the environment. Signs appear after 5-12 hours. The clinical picture includes shortness of breath, weakness, chills, joint and muscle pain, and a feeling of heaviness in the lungs. Sputum discharge is not abundant, there is cyanosis of the integument.
When auscultating the lungs, a characteristic crunching sound is observed, in the basal zones there is a whistle. Patients also complain of headaches.
Symptoms can last from a day to 72 hours, then disappear. Occur again with repeated exposure to the agent. In children, shortness of breath persists for several weeks, especially after physical exertion.

Acute allergic alveolitis is difficult to diagnose, since the symptoms are similar to atypical pneumonia. In patients with mycotoxicity, serum radiographs do not show precipitation. Small-nodular or diffuse infiltration and gas exchange disturbance are detected.
Subacute form
The intensity of allergen penetration is much weaker, usually characteristic of home conditions, so this type more often develops in children. Symptoms: shortness of breath, pain in the lungs, increased fatigue, fever. When coughing, mucous sputum is released. Crepitational rales are soft. Rapid shallow breathing reaches more than 20 breaths per minute in adults, and over 40 in children.
Chronic form
If dust enters the lungs for a long time, allergic alveolitis develops into a chronic form. Characteristic signs are increasing shortness of breath and a sharp decrease in body weight, up to anorexia. Subsequently, fibrous interstitiality and heart and lung failure develop.
Radiology
In the acute form, no special changes may be observed, but in some cases a pronounced interstitial and pneumosclerotic picture is revealed. The indicators are displayed in the haze of the lung silhouettes and the distribution of nodular shaded areas. The size of the lesions does not exceed 3 mm and affects the entire area of the organs, except for the apexes and basal areas.
In the chronic type, the linear outlines have clear boundaries and preserved tissue hemodynamics. The interalveolar septa are thickened, numerous foci are found along the branching of the lymphatic vessels.
During an attack of the disease, a leukocytic shift to the left is observed. Precipitants are found in most patients. This is important when the nature of the antibodies remains unclear.
Spirometry tests show a decrease in lung capacity. There are symptoms of obstructive changes in the bronchi. The patency of small vessels is also reduced, tissue extensibility is reduced, and hypoxemia is pronounced.
Biopsy
Transbronchial or open analysis can reveal the existence of infiltrate, accumulations of fibrous tissue, and granulosa lesions. Also shows lymphocytic and interstitial changes. Pneumothorax may occur as a result of the procedure.
The clinical picture of exogenous allergic alveolitis depends on the nature of the disease: acute, subacute or chronic. Of great importance for diagnosis is an indication of contact with rotting hay or other sources of organic dust. In the acute course, patients complain of the appearance 6-8 hours after contact with the antigen of shortness of breath, chills, fever and cough with the release of scanty, sometimes blood-stained sputum.
Some patients develop cyanosis. Crepitating rales are heard over the entire surface of the lungs. A clinical blood test may reveal moderate leukocytosis. ESR is slightly increased. Changes in the lungs during X-ray examination are insignificant. There may be some enhancement of the pulmonary pattern and mildly expressed small focal disseminated shadows in the lungs.
In the chronic course of the disease, the clinical picture is dominated by signs of respiratory and cardiac (mainly right ventricular) failure, shortness of breath and cough become constant, and radiographically this process is accompanied by the appearance of more pronounced pneumosclerosis and the progression of disseminated focal changes in the lungs. Sometimes an X-ray appearance described as a “honeycomb lung” appears.
When the disease is more than 10 years old, 60-70% of patients have chronic bronchitis, and 25% have pulmonary emphysema. Spirography most often (45% of cases) determines a combination of obstructive and restrictive disorders of external respiration; only restrictive changes were noted in 30% and purely obstructive changes in 3% of patients.
To diagnose exogenous allergic alveolitis, the determination of precipitating antibodies to the antigen, contact with which is considered as the most likely cause of the disease, can be used. High titers of precipitating antibodies to the test antigen can indicate its etiological significance only in the presence of clinical, radiological and functional manifestations of the disease, since in 30-40% of practically healthy individuals who have contact with the test antigen, precipitating antibodies are detected in diagnostic titers [IIIerBop N.V. - In the book: R15man A., 1980].
To clarify the diagnosis in individual patients, a provocative test is performed, during which the patient is placed in the environment in which he fell ill, and the resulting changes in the patient’s condition are assessed. The need for such a test is most obvious in cases where the microflora found in air conditioning and humidifying installations is suspected as the cause of alveolitis. However, this test should be carried out only in isolated cases and with great caution, as it can lead to a worsening of the patient’s condition.
Differential diagnosis should be made with disseminated lung lesions (alveolar and metastatic cancer, miliary tuberculosis, sarcoidosis and other fibrosing alveolitis, aspergillosis, etc.).
Lung cancer differs from exogenous allergic alveolitis in the absence of a connection between the disease and exposure to an exogenous allergen, the steady progression and greater severity of the disease, the peculiarities of radiological signs of lung damage, and the absence of precipitating antibodies to any allergen in the blood serum.
Miliary pulmonary tuberculosis differs from exogenous allergic alveolitis in the absence of connection with external antigens, more pronounced severity and duration of the disease, the peculiarity of radiological manifestations, positive serological and skin reactions with tuberculosis antigen, and the absence in the blood serum of increased titers of precipitating antibodies to any exoallergen , which can lead to allergic alveolitis.
Sarcoidosis differs from exogenous allergic alveoli, in addition to clinical, laboratory and radiological data, by enlargement of the hilar lymph nodes, changes in joints, eyes and other organs.
Distinctive features of fibrosing alveolitis in systemic connective tissue lesions are vasculitis and multiorgan involvement. Bronchopulmonary aspergillosis differs from exogenous allergic alveolitis by pronounced eosinophilia and the predominance of obstructive changes in the bronchi with bronchospasm over restrictive changes.
In cases where the differential diagnosis is especially difficult, for example, in the chronic course of allergic alveolitis, a biopsy of the lung tissue is performed with a histological examination of the biopsy material.
The following symptoms of exogenous allergic alveolitis are distinguished:
- Shortness of breath when there is difficulty in exhaling. It is the main symptom indicating this disease. Appears during physical activity, then in a calm state;
- Cough with sputum production;
- Weight loss;
- High temperature, fever;
- Bilateral chest pain;
- Fatigue, malaise, decreased performance;
- Loss of appetite;
- Wheezing when breathing;
- Hyperemia;
- Accelerated sweating;
- Blueness of the skin;
- Changes in the shape of the fingers, in which the bones thicken and the nails become convex.
Since a person rarely pays attention to indolent symptoms, he continues to work in an environment full of antigens. As is known, prolonged contact with allergens leads to the development of bronchial asthma or EAA.
Treatment
Timely identification and elimination of the cause may be sufficient to suppress inflammation, especially with minor and short-term exposure to a negative factor. With further progression of the pathology and acute damage to the lung tissue and other organs, the doctor prescribes:
- glucocorticosteroids;
- bronchodilators;
- mucolytics;
- cardioprotectors;
- antacids, prokinetics.
According to official clinical recommendations, the synthetic glucocorticoid Metipred and similar medications provide the best treatment results for both toxic-allergic alveolitis and ordinary toxic alveolitis.

Metipred
Expert opinion
Anna Sandalova
Pulmonologist, doctor of the highest category
Ask a Question
The type of drug, its dosage and duration of use are determined by the age of the victim, the tolerability of certain drugs, and the severity of the condition.
When a secondary bacterial infection occurs, the therapeutic regimen must be supplemented with broad-spectrum antibiotics. If there is a threat of pulmonary edema and a decrease in oxygen in the blood, oxygen therapy is indicated. All patients with toxic alveolitis are recommended breathing exercises and physiotherapy.
For chronic inflammation, treatment is largely aimed at reducing the rate of progression of the pathology. The doctor understands that a significant amount of normal lung tissue has been replaced by connective tissue that does not perform any functions, so he often prescribes symptomatic medications (bronchodilators, mucolytics).
See also review about pneumoconiosis
Fibrosing alveolitis
This is a progressive lung disease in which sclerosis of the alveolar septum and inflammatory infiltration are observed. The course of fibrosing alveolitis is rapidly progressive, as respiratory failure increases rapidly. The patient has the following symptoms:
- Chest pain.
- Cough (dry).
- Hemoptysis.
- Loss of body weight.
- Enlargement of the phalanges of the fingers.
And also at the last stage of inflammation, the referred to “honeycomb lung” is formed, or in scientific terms - cystic-bullous transformation of the lungs. Treatment of such alveolitis requires immunosuppressive therapy.
Exogenous allergic alveolitis includes diseases of the bronchi and lungs, in which inhalation of organic dust causes hypersensitivity reactions with primary damage to the alveoli and bronchioles. The disease is especially widespread among people whose work is related to agriculture.
Causes and mechanisms of development
At this stage of studying the problem, clinicians distinguish three forms of alveolitis , taking into account the etiology, pathogenesis and clinical picture of the disease:
- idiopathic;
- toxic allergic;
- exogenous toxic.
The latter type is characterized by the absence of disorders of the immune system. The disease occurs due to the influence of a certain chemical compound or complex of toxic substances. Often its formation is facilitated by inadequate doses of medications:
- cytostatics and immunosuppressants;
- antibiotics and other antibacterial agents;
- oral hypoglycemic medications and many others.
Toxic fibrosing alveolitis also develops due to prolonged inhalation of oxygen, inhalation of irritating gases (chlorine, ammonia, mercury compounds, beryllium, herbicides).
The pathogenesis is clear and simple: the etiological factor directly affects the walls of the pulmonary capillaries and leads to disruption of microcirculation in the alveoli. Edema and infiltration appear, and pneumosclerosis develops.
Pathogenesis of Exogenous allergic alveolitis:
The pathogenesis of exogenous allergic alveolitis has not yet been sufficiently studied. There are indications that precipitating antibodies to rotting hay antigens were found in the blood serum of 80% of patients with “farmer’s lung”. The pathogenic role of antibodies in patients with “farmer's lung” is currently disputed, since precipitating antibodies were also found in a large percentage of practically healthy farmers who had contact with rotten hay.
A number of studies have demonstrated the presence of hypersensitivity reactions of types I and IV in patients with exogenous allergic alveolitis. It turned out that antigens from organic dusts can stimulate an alternative pathway for activating complement. The experiment established the participation in the pathogenesis of exogenous allergic alveolitis of reactions caused by activated alveolar macrophages.
Pathological changes depend on the stage of the disease and are characterized by changes of varying severity from acute alveolar-interstitial reaction to diffuse pulmonary fibrosis [Crafton J., Duglas A., 1974J. In the acute course of exogenous allergic alveolitis, histologically, as a rule, diffuse inflammation of the interstitium, the formation of granulomas, and, less commonly, bronchiolitis obliterans, acute inflammation with infiltration of polynuclear cells, vasculitis, and hemorrhages are observed. In immunofluorescence studies, the C3-fraction of complement and immunoglobulins fixed in the lungs are rarely detected.
Symptoms of Exogenous allergic alveolitis:
The clinical picture of exogenous allergic alveolitis depends on the nature of the disease: acute, subacute or chronic.
Of great importance for diagnosis is an indication of contact with rotting hay or other sources of organic dust. In the acute course, patients complain of the appearance 6-8 hours after contact with the antigen of shortness of breath, chills, fever and cough with the release of scanty, sometimes blood-stained sputum. Some patients develop cyanosis. Crepitating rales are heard over the entire surface of the lungs. A clinical blood test may reveal moderate leukocytosis. ESR is slightly increased. Changes in the lungs during X-ray examination are insignificant. There may be some enhancement of the pulmonary pattern and mildly expressed small focal disseminated shadows in the lungs. When contact with allergenic agents is stopped, clinical and radiological signs of the disease may spontaneously disappear after 3-4 weeks, but repeated contact leads to a subacute course of the disease, in which clinical and radiological changes disappear much more slowly. In the chronic course of the disease, the clinical picture is dominated by signs of respiratory and cardiac (mainly right ventricular) failure, shortness of breath and cough become constant, and radiographically this process is accompanied by the appearance of more pronounced pneumosclerosis and the progression of disseminated focal changes in the lungs. Sometimes an X-ray appearance described as a “honeycomb lung” appears.
When the disease is more than 10 years old, 60-70% of patients have chronic bronchitis, and 25% have pulmonary emphysema. Spirography most often (45% of cases) determines a combination of obstructive and restrictive disorders of external respiration; only restrictive changes were noted in 30% and purely obstructive changes in 3% of patients. In addition, in patients with exogenous allergic alveolitis, impaired patency of both large and small bronchi, changes in the distribution of air in the lungs, a decrease in the diffusion capacity of the lungs and an increase in pressure in the pulmonary artery were identified.
Allergic alveolitis in ICD classification:
- J67 Hypersensitivity pneumonitis caused by organic dust (Selected ICD-10 diagnosis)
- Subsections:
- J67.0 Farmer's lung
- J67.2 Poultry farmer's lung
- J67.4 Malt handler's lung
- J67.5 Mushroom Worker's Lung
- J67.6 Maple bark harvester's lung
- J67.7 Lung in contact with air conditioning and humidifiers
- J67.8 Hypersensitivity pneumonitis due to other organic dusts
- J67.9 Hypersensitivity pneumonitis due to unspecified organic dust
- Related codes:
- J60 Coal miner's pneumoconiosis
- J61 Pneumoconiosis due to asbestos and other mineral substances
- J62 Pneumoconiosis caused by dust containing silica
- J63 Pneumoconiosis due to other inorganic dusts
- J64 Pneumoconiosis, unspecified
- J65 Pneumoconiosis associated with tuberculosis
- J66 Respiratory disease caused by specific organic dust
- J69 Pneumonitis due to solids and liquids
- J70 Respiratory conditions caused by other external agents
Clara:09/01/2015 Hello! My son started taking staloral, a mite allergen. The initial course ended, I took it according to the instructions. Now we need to take the maintenance course, the third bottle. How many days should I take the maintenance course?
Diagnosis of Exogenous allergic alveolitis:
To diagnose exogenous allergic alveolitis, the determination of precipitating antibodies to the antigen, contact with which is considered as the most likely cause of the disease, can be used.
High titers of precipitating antibodies to the test antigen can indicate its etiological significance only in the presence of clinical, radiological and functional manifestations of the disease, since in 30-40% of practically healthy individuals who have contact with the test antigen, precipitating antibodies are detected in diagnostic titers [IIIerBop N.V. - In the book: R15man A., 1980]. To clarify the diagnosis in individual patients, a provocative test is performed, during which the patient is placed in the environment in which he fell ill, and the resulting changes in the patient’s condition are assessed. The need for such a test is most obvious in cases where the microflora found in air conditioning and humidifying installations is suspected as the cause of alveolitis. However, this test should be carried out only in isolated cases and with great caution, as it can lead to a worsening of the patient’s condition. Differential diagnosis should be made with disseminated lung lesions (alveolar and metastatic cancer, miliary tuberculosis, sarcoidosis and other fibrosing alveolitis, aspergillosis, etc.).
Lung cancer differs from exogenous allergic alveolitis in the absence of a connection between the disease and exposure to an exogenous allergen, the steady progression and greater severity of the disease, the peculiarities of radiological signs of lung damage, and the absence of precipitating antibodies to any allergen in the blood serum.
Miliary pulmonary tuberculosis differs from exogenous allergic alveolitis in the absence of connection with external antigens, more pronounced severity and duration of the disease, the peculiarity of radiological manifestations, positive serological and skin reactions with tuberculosis antigen, and the absence in the blood serum of increased titers of precipitating antibodies to any exoallergen , which can lead to allergic alveolitis.
Sarcoidosis differs from exogenous allergic alveoli, in addition to clinical, laboratory and radiological data, by enlargement of the hilar lymph nodes, changes in joints, eyes and other organs.
Distinctive features of fibrosing alveolitis in systemic connective tissue lesions are vasculitis and multiorgan involvement. Bronchopulmonary aspergillosis differs from exogenous allergic alveolitis by pronounced eosinophilia and the predominance of obstructive changes in the bronchi with bronchospasm over restrictive changes.
In cases where the differential diagnosis is especially difficult, for example, in the chronic course of allergic alveolitis, a biopsy of the lung tissue is performed with a histological examination of the biopsy material.
Literature
- Roy Patterson, Leslie K. Gremmer, Paul A. Greenberg “Allergic diseases, diagnosis and treatment”, Moscow, Geotar Medicine, 2000, ISBN 5-9231-0011-8
- “Clinical allergology and immunology”, edited by L. A. Goryachkina and K. P. Kashkin, Moscow, “Miklos”, 2009, ISBN 978-5-91746-002-4
- V. I. Pytsky, N. V. Adrianova, A. V. Artomasova “Allergic diseases”, Moscow, “Medicine”, 1984
- G. I. Drynov “Therapy of allergic diseases”, Moscow, JSC “United Editorial Board Borges”, 2004
- N. M. Berezhnaya, L. P. Bobkova, I. A. Petrovskaya, S. I. Yalkut “Allergology”, Kyiv, “Naukova Dumka”, 1986
Treatment of Exogenous allergic alveolitis:
Treatment of exogenous allergic alveolitis begins with eliminating the allergens that caused the disease from the patient’s environment and stopping the patient’s contact with these allergens.
In acute, severe and progressive disease, glucocorticosteroids are prescribed at 1-1.5 mg of prednisolone per 1 kg of patient weight per day. Corticosteroid drugs are used for several weeks with a gradual reduction in dose until complete withdrawal. The duration of treatment with corticosteroid drugs is highly individual and depends on the clinical effect and how the patient tolerates these drugs. With a mild course of the disease, no drug therapy is required and the symptoms of the disease disappear after stopping contact with the allergen. The prognosis of allergic alveolitis depends on the timely, possibly more complete and early elimination of the etiological factors causing alveolitis from the environment surrounding the patient, and the active treatment of this disease. With repeated recurrence of alveolitis and the appearance of complications from the lungs and heart, the prognosis becomes unfavorable.
Definition
Exogenous allergic alveolitis (EAA) - the term was proposed in 1967 to replace those previously used: allergic pneumonia, exogenous pulmonary granulomatosis, precipitin pneumonia, allergic pneumonitis, organic pneumonitis, organic pneumoconiosis, allergic interstitial pneumonia, hypersensitivity granulomatous pneumonia. EAA includes more than 20 diseases, united by a common pathogenesis and a single clinical picture, but caused by different causes. More than 20 etiological factors are known that are associated with its occurrence.
Pathogenesis of alveolitis
The main condition for the development mechanism is inhalation of the antigenic source in sufficient volumes over a long period. To settle in the lungs, it must have parameters less than 5 microns, but damage to the system is possible when large particles accumulate. Most people, even under such conditions, are not susceptible to developing the disease.
Antibodies and reactions activate the signaling system and the production of macrophages, which release proteolytics, free radical compounds, enhance the creation of fibroblasts and excessive production of collagen. As a result, granulosa interstitial lung disease develops.
In the reaction of the fourth, delayed type, the alveoli are infiltrated by neutrophils. Leukocyte substances are synthesized in small respiratory areas and inflammatory foci. With prolonged entry of allergens into the system, proliferation and transformation nodes are formed that are capable of cellular phagocytes.
Inhalation of irritants in people susceptible to allergies causes a negative reaction in the form of acute alveolitis. Alveolar and interstitial tissues are damaged from exposure to an allergen.
Repeated inhalation of irritants leads to the formation of precipitins and the formation of an immune response. Vascular permeability increases, substances - neutrophils and macrophages - are activated. They produce toxic products such as hydrolytic enzymes, cytocaines, and oxygen radicals. These substances further damage the interstitial tissue.
The pathogenesis of exogenous allergic alveolitis has not yet been sufficiently studied. There are indications that precipitating antibodies to rotting hay antigens were found in the blood serum of 80% of patients with “farmer’s lung”. The pathogenic role of antibodies in patients with “farmer's lung” is currently disputed, since precipitating antibodies were also found in a large percentage of practically healthy farmers who had contact with rotten hay.
A number of studies have demonstrated the presence of hypersensitivity reactions of types I and IV in patients with exogenous allergic alveolitis. It turned out that antigens from organic dusts can stimulate an alternative pathway for activating complement. The experiment established the participation in the pathogenesis of exogenous allergic alveolitis of reactions caused by activated alveolar macrophages.
Pathological changes depend on the stage of the disease and are characterized by changes of varying severity from acute alveolar-interstitial reaction to diffuse pulmonary fibrosis [Crafton J., Duglas A., 1974J. In the acute course of exogenous allergic alveolitis, histologically, as a rule, diffuse inflammation of the interstitium, the formation of granulomas, and, less commonly, bronchiolitis obliterans, acute inflammation with infiltration of polynuclear cells, vasculitis, and hemorrhages are observed. In immunofluorescence studies, the C3-fraction of complement and immunoglobulins fixed in the lungs are rarely detected.
Causes
Despite the diversity of etiological factors, EAA nevertheless represents a single disease due to the common pathogenesis, the identity of the morphological basis and clinical manifestations.
People come into contact with most of the numerous etiological factors of the disease in an industrial environment, so it is often occupational. However, this does not mean that infection is impossible in other conditions, in particular in households, where the cause may be contact with birds, animals, etc. Molds are often found in houses, especially in their foundations, creeping plants, house dust, rotting products. Finally, no one is protected from the effects of microbes when they seasonally pollute the air.
But the susceptibility to the disease of persons who have systematic professional contact with potentially hazardous substances is immeasurably higher, and it is they who mainly suffer from EAA, which made it possible, after the first description of the disease called “farmer’s lung,” to continue the list of those suffering from representatives of other professional groups. Today, this division is purely arbitrary and can only be useful by accurately indicating the profession that was the cause of the disease, narrowing the range of possible etiological factors.
The pathogen enters by inhalation and manifests itself as an antigen, causing an immunological reaction predominantly of type III. Under the antigenic influence of an etiological factor, precipitating antibodies related to IgM are formed, which, combining with the antigen, form large-molecular immune complexes (IC) (they are isolated from the blood and lung tissue of patients with EAA). In this case, the complement system is activated, which results in, on the one hand, the formation of its components C3, C5a, which have the properties of inflammatory mediators, and on the other, the release from cells of biologically active substances endowed with anaphylactogenic properties. IRs are deposited under the endothelium of the alveolar capillaries, causing the development of Arthus-like processes. The reaction involves lysosomal enzymes that damage lung tissue. The final stage of alterative processes in the lung tissue is the development of necrosis and fibrosis.
In addition, type IV reactions are involved in the pathogenesis of EAA - cell-mediated, leading to the formation of characteristic morphological changes in the lung tissue in the form of cellular, predominantly mononuclear infiltrates and granulomas. And finally, a certain place in the pathogenesis of the disease belongs to type I reactions, evidence of which is an increase in the level of lgE. Perhaps this mosaic nature of the immune response in EAA is explained by the impact on the body of a multifactorial system: different antigenic substances of the same antigen or different antigens, some of which cause the formation of IgM, others - IgE, and others - a cellular immune response. The result of immunological reactions caused by the antigen is an acute inflammatory process in the lungs.
Exogenous allergic alveolitis: classification
Alveolitis is traditionally divided in medicine into acute, subacute and chronic. The subacute and acute forms disappear after the cause of the allergy is determined and the person stops contacting the allergen. But if the inflammation has reached a chronic stage of development, the person will be forced to take steroid hormones for a long time in order to relieve severe inflammation and swelling.
In the chronic stage, the cough is very severe, sometimes bloody, and is often accompanied by fever. It is clear that this is a division based on the nature of the course of the disease. But diseases are also distinguished depending on the allergen that caused the abnormal reaction. For example, the lung of a farmer, a cheese maker, or a person using an air conditioner.
Etiology
Allergens that cause this type of disease can be fungal spores that are found in broken hay, maple bark; less often - plant dust, protein antigens, house dust, medicines. They enter the body through inhaled air or (less commonly) through non-inhalation routes. As with ELISA, in exogenous alveolitis the main role in pathogenesis is played by the immune complex mechanism of tissue damage.[1] Antigen-antibody complexes are deposited in the walls of the alveoli, the smallest bronchioles and blood capillaries, causing their inflammation, resulting in fibrosis, and possibly the formation of granulomas.
Depending on the etiological factor, there are several variants of allergic alveolitis, which have quite exotic names.
| Type of alveolitis | Allergen source | Allergens for which there are precipitins |
| Barn disease | Scattered wheat | Granary weevil (Sitophilus granarius) |
| Bagassoz | Moldy sugar cane | Thermoactinomyces vulgaris |
| Pituitary powder inhaler disease | Powder of dried pituitary glands of pigs and cattle | Pituitary antigens |
| Coffee miller's disease | Coffee beans | Coffee bean dust |
| Disease of those washing in the sauna | Wet wood | Pullularia |
| Disease of those working with wood pulp | Wood pulp | Alternaria |
| Cheese factory workers illness | Some types of cheese | Penicillium casei Penicillium glaucum |
| Weavers cough | Moldy cotton | |
| Piper's lung | Dirty wind musical instruments | Fusarium oxysporum Penicillium species Rhodotorula mucilaginosa[2][3] |
| Tanner's lung | Moldy maple bark | Cryptostroma corticale |
| Bird lovers lung | Droppings and feathers of pigeons, chickens, budgies | Whey proteins |
| Furrier's lung | Karakul, fox fur | |
| Thresher's lung | Ground pepper | |
| Lung of New Guineans | Moldy reed dust | |
| Lungs working with mushrooms | Fungal spores | Thermoactinomyces vulgaris Micropolyspora faeni |
| Lungs working with malt | Rotted barley malt dust | Aspergillus fumigatus Aspergillus clatus |
| Farmer's lung | Rotten hay | Micropolyspora faeni |
| Summer hypersensitivity Japanese pneumonitis | Moist, warm indoor air containing fungal spores | Thermoactinomyces vulgaris Cryptococcus neoformans |
| Lycoperdinosis | Puffball mushroom spores | |
| Redwood | Mahogany sawdust | Aureobasidium pullulans |
| Suberosis | Cork dust | Mildew dust of balsa wood |
Correct treatment of pulmonary alveolitis
Treatment of exogenous allergic alveolitis begins with eliminating the allergens that caused the disease from the patient’s environment and stopping the patient’s contact with these allergens. In acute, severe and progressive disease, glucocorticosteroids are prescribed at 1-1.5 mg of prednisolone per 1 kg of patient weight per day.

Corticosteroid drugs are used for several weeks with a gradual reduction in dose until complete withdrawal. The duration of treatment with corticosteroid drugs is highly individual and depends on the clinical effect and how the patient tolerates these drugs. In mild cases of the disease, no drug therapy is required and the symptoms of the disease disappear after stopping contact with the allergen.
The prognosis of allergic alveolitis depends on the timely, possibly more complete and early elimination of the etiological factors causing alveolitis from the environment surrounding the patient, and the active treatment of this disease. With repeated recurrence of alveolitis and the appearance of complications from the lungs and heart, the prognosis becomes unfavorable.
The patient is hospitalized to undergo treatment for EAA under the close supervision of doctors. How to treat?
- The main factor in treatment is the elimination of the antigen that provokes the allergic reaction in the lungs.
- Glucocorticoid hormones and prednisolone are used to suppress the inflammatory process.
- If there is an overgrowth of connective tissue in the lungs (fibrosis), anti-fibrotic drugs are used.
- To eliminate shortness of breath, bronchodilators (bronchodilators) are used.
- To saturate the body with oxygen, oxygen therapy (inhalation) is performed.
- Antihistamines are used to eliminate the symptoms of pathology.
- Antibiotics or macrolides are used to kill bacteria.
To prevent the disease, industrial and household reagents that cause pulmonary disease should be avoided. Gauze dressings should be used if exposed to atmospheres containing antigens. Cromolyn, bronchodilators, nedocromil reduce the body's response to irritants in the early stages. Constant allergological examination by a doctor becomes part of the patient’s life.
The prognosis for acute alveolitis, as we learned, is positive. In the acute phase, Prednisolone or Dexasone is used for only a few days. The drug is prescribed to relieve inflammation, since the drug has the ability to suppress the functions of tissue macrophages and leukocytes that fight irritants.
In case of chronic alveolitis, you need to take a dose of corticosteroids for about 8 months. Adults take Azathioprine, a strong immunosuppressive drug. In addition to active treatment of inflammation, it is necessary not to forget about the general condition of the body. It is important to monitor serum iron levels, general blood and urine tests during treatment. This will help prevent the re-development of exogenous allergic alveolitis.
Prevention
The first step is to eliminate the antigen. In mild cases this can lead to a cure. If recovery does not occur, as well as in more severe cases of the disease, glucocorticoid drugs are used. In the acute form, the effect of steroid therapy appears after a few days, in the chronic form - after several months (40-60 mg per day for a week, then a maintenance dose for 4-6 weeks). In chronic cases, 20 mg is used to prevent relapses for several months. The effectiveness of therapy can be monitored by the IgE level (it increases before each exacerbation). There is a positive effect from intal. If the cause of EAA is fungi, hyposensitization is carried out with them. Bronchodilators and antifungal drugs are ineffective.











