If an allergic reaction occurs, you always need to clarify what exactly caused the alarming symptoms. There are a considerable number of antigens that provoke the disease. They are collected in a frequently used pediatric allergy panel, which allows you to find out what exactly the human body cannot tolerate. It is difficult to understand on your own why the negative symptoms arose. Perhaps the person has an intolerance to wool or dust. It also happens that hives appear due to detergent or washing powder. An allergen panel is useful if it is unclear what exactly led to the negative manifestations. You should definitely consult a doctor, as testing yourself cannot be translated.
In general, an allergy panel is useful because it allows you to find out what substance is causing the painful symptoms in an allergic person. It contains the most common irritants, but, of course, it does not contain absolutely all components. Before using the pediatric major allergen panel, you need to be well prepared. This is required in order to obtain the most reliable conclusion. It is useful to know that there are different types of tools, for example, food allergen panel, inhalation panel. A person must decide which option is right for him in order to undergo a specific test.
What types of allergy panels exist?
There are a considerable number of antigens in the world that are poorly tolerated by the body of different people. For some, intolerance manifests itself since childhood, while others encounter it in adulthood. In any case, if unpleasant symptoms appear regularly, it is necessary to undergo diagnostics and understand which substances are best avoided.
It should be understood that provocateurs can enter the body in different ways. Some of them are ingested through food or liquid and then irritate the digestive system. There are situations when a patient inhales an element, say pollen, which causes pathological manifestations. There are frequent cases of contact allergies, for example, after interaction with a cream, detergent, or medication.
People often wonder what kind of allergen panels there are now. Before testing, you have to choose what exactly to test.
Varieties:
- Food. An immunopathological reaction often occurs to food products that have significant allergic indicators. For this reason, it is recommended to check what foods the allergy sufferer's body cannot tolerate. The list includes various ingredients. For example, apples, soybeans, chicken eggs, milk, nuts, oranges and lemons, tomatoes, potatoes. It is definitely worth checking how the body perceives seafood, as it often provokes rashes, intestinal upset and itching.
- Inhalation. The list includes respiratory antigens. They enter the body by inhalation through the nose or mouth. This phenomenon is common, so you should definitely check whether there is an inhalation type of allergy. Provocateurs include fur and skin particles. It is especially necessary to check the reaction to pets, since the patient is in constant contact with them.
- Mixed. It includes all irritants, both inhaled and food. This option is recommended for citizens who do not understand why their pathology is worsening. An expanded list of substances allows you to identify a specific antigen as accurately as possible.
The pediatric panel is a separate type that includes about 20 components to which children are most often allergic. This option is suitable for minors who most often do not understand what exactly causes a rash, cough, runny nose, watery eyes and other symptoms.
It contains the following elements:
- Pollen from birch and alder.
- Chicken eggs: interested in both the white and the yolk.
- Fermented milk products, cow's milk.
- Creeping wheatgrass.
- Wool and elements of the dermis of cats and dogs.
- Meadow foxtail.
- Two types of mites living in house dust.
- Tares.
- Meadow fescue.
- Fragrant spikelet.
- Peanut.
- Wheat flour.
- Carrot.
- Fungus Alternaria Alternata.
- Alpha-lactalbumin.
- Beta-lactoglobulin.
- Bovine serum albumin.
It is worth noting that the test is carried out in different ways, as it depends on the age of the minor. Children under three years of age should not undergo a skin test, as it is ineffective. The results are significantly distorted and do not correspond to the truth. Analysis of total immunoglobulin type E is not prescribed for patients who are not even 6 months old. The procedure will not give the right answers, since immunity is just beginning to develop.

To determine the irritant, blood is donated from a vein for testing. Before 5 years of age, the hemotest is not used, as it will not give reliable results. Let’s say there is a negative reaction to the milk of a goat or cow, and when testing the serum for immunoglobulin, an indicator of 0 will be obtained.
Causes of allergies
When a foreign element enters the body, the immune system begins to fight the foreigner. Antibodies block the allergen, binding it with a membrane, thereby forming IgE and IgG4 antibodies. The interaction of the allergen and antibodies leads to the appearance of histamines, which provoke an allergic reaction.
There are 4 types of antibodies that cause 4 types of allergies, each corresponding to a wide list of pathogens. For example:
- citrus fruits (lemons, oranges, tangerines);
- wool;
- eggs;
- plant pollen;
- dust mites;
- nuts;
- starch;
- a red pigment from fruits and vegetables called lycopene;
- animal proteins.
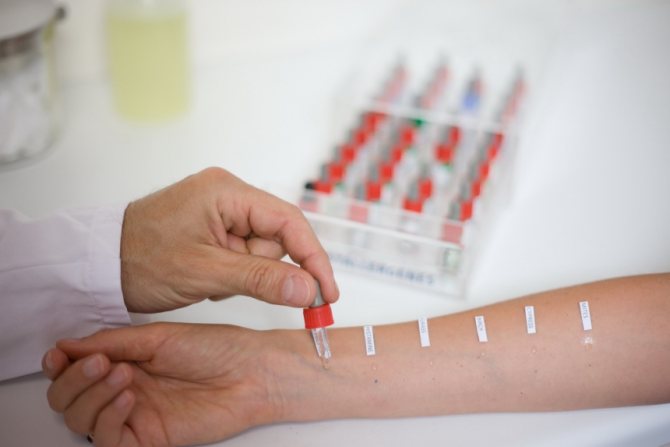
To determine the allergen, doctors conduct tests. About 15 tests can be performed at a time. The patient's hand is scratched and the allergen is introduced. After fifteen minutes, the patient’s skin will respond to the reagent with redness and itching. A negative factor of this method is the likelihood of a false positive result.
Such tests are not performed if there are symptoms of infection and fever, or in children under three years of age.
Preparation for the procedure
Testing using an allergen panel is prescribed for children who have suspected allergies. If the disease does not go away for a long time or constantly recurs, it is necessary to accurately determine the provocateur. If your immunoglobulin E level is high, you will need to be tested for allergies.
The test is never performed during a period when children have respiratory, viral and bacterial pathologies. They can influence the level of immunoglobulin in the blood. For this reason, the results will be significantly distorted and will not answer the main question.
It is recommended to schedule the procedure in the morning - it is best to start the process between 7 am and 11 pm. This is the most favorable period for donating biological material. In addition, children will not have to suffer because they cannot eat food before the study. Therefore, you cannot sign up for a time in the afternoon or in the evening, since it is easiest to get through the fence in the morning.
If an allergy is present, regardless of severity, diagnosis is postponed. During an exacerbation, in any case, there is a specific work of the immune system. Again, it will not be possible to figure out exactly what you are dealing with.
It is necessary to take into account a number of rules that every patient must follow:
- Blood for further research is donated exclusively on an empty stomach. In the morning you are allowed to drink only water. Strong tea, cocoa and coffee should be avoided.
- At least 8 hours must have passed since the last meal. It is advisable for the baby to have dinner three hours before bedtime, and then not eat anything.
- Blood is drawn before the start of medication use. This rule may not be followed if a course of therapy has already been started. In this case, before testing you will have to wait at least 7 days from the moment you stop taking the drugs. If medications cannot be abandoned, and the test is urgently required, then it is indicated what medications the allergic person took, as well as in what dosage.
- The day before the test, it is recommended to avoid fried and fatty foods, alcohol-containing drinks, and intense physical activity. Such factors can distort the final results.
The patient must familiarize himself with how the procedure is performed in advance. The parent must explain to the child what exactly awaits him. It is important that the baby does not worry or be afraid of medical manipulations, otherwise the task will become more complicated.
The doctor himself will interview the patient or his parents about alarming symptoms and the presence of allergic diseases in relatives. It should be mentioned what an immunopathological reaction could presumably be to, in order to make the doctor’s task easier. For children, the doctor uses a pediatric panel, since it contains the most relevant stimuli.

Before the process, the doctor will treat the patient’s arm with an anesthetic, then clamp it slightly above the elbow area with a special tourniquet. The allergist will ask you to tense your limb, as this will make the vein appear. This is required for further blood sampling. Using a syringe, the doctor will take the required amount of liquid, after which the child can go home.
The conclusion will be ready in about a week. If necessary, express diagnostics are carried out, and in such a situation the answer can be obtained in just two days.
Some people want to know in advance the transcript of the results of the pediatric panel in order to independently understand what exactly they are dealing with. It is worth focusing on certain criteria in order to find out to which substances an immunopathological response was detected.
Options for interpreting results
A positive result indicates the presence of sensitivity, but does not confirm that one or another allergen plays a major role in the development of symptoms. The panel is a screening to identify potential allergy triggers. If, according to tests, the child is sensitive to tree pollen, and began coughing and sneezing in winter, there is no need to associate the symptoms with the identified allergen, since it is seasonal, and in the room the child could encounter household allergens, for example, animals or dust.
Quality option
It is intended to visually evaluate changes on the test membrane. The laboratory technician compares the test allergy test with the test sample. This option is subjective, since the evaluation criterion can only be the saturation of the color. The result implies two answers: positive (confirmation of antibodies); negative (no immune intolerance). The disadvantage of the method is the poor level of content of the response; it is impossible to determine the severity of sensitivity to the allergen, track changes over time and find out how significant a given allergen is for a given patient.
Semi-quantitative option
Involves interpretation of the answer in conventional units for a specific laboratory. These are six classes, starting from zero (negative indicator), that is, the absence or low concentration of antibodies that will not cause symptoms in the patient. The assessment is carried out visually or using special devices, the data of which is processed by special programs. But the principle is the same: the brighter the test line, the stronger the reaction.
Quantitative option
This method is more convenient for the doctor. It is used to determine the concentration of antibodies in a patient's blood sample using a pediatric allergen panel. Decryption is carried out by specialists using reference data:
- Class 0. Less than 0.35 kU/L. The patient is not sensitive to the allergen, the result is negative.
- Class 1. From 0.35 to 0.7 kU/L. The result is considered doubtful, there could be errors, the results cannot be interpreted qualitatively, and there are often no allergy symptoms with such results.
- Class 2. From 0.7 to 3.5 kU/L. Weak positive result. The reaction should be confirmed by additional studies.
- Class 3. From 3.5 to 17.5 kU/L. Positive result. There is definitely an allergy.
- Class 4. From 17.5 to 52.5 kU/L. Moderately high level
- Class 5. From 52.5 to 100 kU/L. High level
- Class 6. More than 100 kU/L. Very high level
Severe reactions occur in patients with levels of 17.6 and above . In such situations, treatment and monitoring by a doctor is necessary. The pediatrician may prescribe antihistamines in tablets (or syrup if the child is under two years old), ointments that reduce redness and itching, and diet.
It happens that parents are to blame for a child’s dust allergy due to poor cleaning or food allergies due to poor nutrition.
When the pediatric panel does not give results, it is necessary to consult a gastroenterologist. Dysbacteriosis can also have consequences in the form of peeling, rash and itching.
What is a pediatric allergen panel and what does it mean?
The pediatric allergen panel is the simplest and most reliable way to help identify allergies to any product, product, wool, or pollen.
Table of contents:
The method is successfully used to diagnose allergies in adults and children from 6 months of age.
The allergopanel helps to identify a negative reaction to a certain substance, because differentiating an allergen in everyday life is not easy.
The panel indicates the most common allergens that are dangerous to the body.
Food allergen panel. Indications
Like any other disease, food allergies are not asymptomatic.
On the contrary, one usually does not have to wait for their occurrence. Moreover, sometimes the symptoms are quite pronounced:
- Nausea, vomiting.
- Pain in the stomach area.
- Bloating.
- Abnormal stool.
- The appearance of an itchy rash on the skin.
- With a pronounced allergic reaction, Quincke's edema and urticaria may occur.
In children under one year of age, characteristic symptoms will be:
- The presence of persistent diaper rash that does not go away even with careful care of the baby’s skin.
- Irritation around the anus. In boys, the tip of the penis may also turn red.
- The baby becomes restless, sleeps poorly and cries a lot.

All this may be a reason to consult a doctor and donate blood for a test. The food allergen panel is the name of a method for diagnosing allergies.
Decoding
The inhalation allergen panel is deciphered, just like the pediatric one, based on the level of IgE, IgG4. The indicators of these substances can range from 0 to 100. And depending on what the result of a laboratory test shows, one can judge the absence or presence of allergies. Decoding by indicators:
- 0.34 or less – no negative reaction (category 1);
- 0.34-0.8 – weak reaction to the substance (category 2-3);
- 0.8-3.6 – there is a respiratory or food allergy (category 4);
- 4-17 – pronounced allergic reaction with high dynamics (category 5);
- 17-100 – the immune response is very strong, the development of undesirable consequences hazardous to health is possible, considered a critical level (category 6)
Identifying respiratory allergies is important. Since the long course of the disease can subsequently lead to the development of bronchial asthma and anaphylactic shock.
Timely, accurate diagnosis helps to identify the type of allergen, begin proper treatment, and, if necessary, limit contact with the allergen.
allergolog1.ru
Pediatric allergy complex RIDA-screen No. 4, IgE
A comprehensive study that allows you to quantify the level of IgE antibodies in the blood separately to each of the most relevant allergens for children: household (mites D. farinae and D.
pteronyssinus), epidermal (epithelium and fur of cats, dogs), pollen (birch, mixture of meadow grasses), fungal (Alternaria alternata) and food (chicken egg white and yolk, cow's milk, casein, alpha-lactalbumin, beta-lactoglobulin, bovine serum albumin, potatoes, carrots, wheat flour, soybeans, hazelnuts, peanuts) .
Detectable allergens:
- House dust, Derm.pteronyssinus
- House dust, Derm.farinae
- Birch
- Mixture of herbs: rye (Secalecereale), meadow timothy (Phleumpratense), meadow fescue (Festucaelatior pratensis), tall ryegrass (Arrhenaterumelatius), fragrant spikelet (Anthoxanthumodoratum), awnless brome (Bromusinermis), creeping wheatgrass (Agropyronrepens), hedgehog grass (Dactylisglo merata ), chaff (Lolium perrene), meadow foxtail (Alopecurus pratensis), woolly milkweed (Holcuslanatus), pig's finger (Cynodondactylon)
- Cat
- Dog
- Alternaria alternate
- Milk
- a-lactalbumin
- b-lactoglobulin
- Casein
- Egg white
- Egg yolk
- Bovine serum albumin
- Soya beans
- Carrot
- Potato
- Wheat flour
- Hazelnut
- Peanut
Synonyms Russian
Specific IgE antibodies to food and respiratory allergens RIDA.
English synonyms
RIDA qLine Allergy Panel 4 (Pediatric Panel).
Research method
Immunoblotting.
Units
IU/ml (international unit per milliliter).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Do not eat for 2-3 hours before the test; you can drink clean still water.
- Do not smoke for 30 minutes before the test.
General information about the study
Recently, allergic reactions are being recorded more and more often, and the frequency of allergic diseases is growing significantly throughout the world.
And if in adults sensitization to inhaled allergens (entering through the respiratory system) predominates, then in children hypersensitivity to food products is more significant, which is associated with the immaturity of the gastrointestinal tract.
In most cases, children under 5-6 years of age develop tolerance to food allergens, but sometimes sensitization to certain foods remains for life.
Reactions in children, as in adults, can be either truly allergic or pseudoallergic, which clinically manifest themselves similarly, but differ in the mechanisms of development and approaches to prevention and treatment.
Particular attention is paid to immediate (anaphylactic, reagin, IgE-related) hypersensitivity reactions, which are involved in many allergic diseases, including cases of severe anaphylaxis.
With this type of allergic reaction, it is possible to identify provoking allergens or exclude sensitization to them by determining specific IgE antibodies in the blood serum.
However, it must be taken into account that an increase in the level of IgE antibodies may indicate existing sensitization of the body, which is not accompanied by visible clinical symptoms, and therefore may not require the complete exclusion of a food product that is important for the child. However, this should only be decided by the attending physician.
This study determines IgE antibodies to respiratory and food allergens, to which hypersensitivity is most often observed in childhood.
Allergens can enter the body through the respiratory tract (inhaled allergens), with food, or through the skin and mucous membranes.
This division is somewhat arbitrary, since, for example, wheat flour, dried egg whites can also act through the respiratory system, skin and mucous membranes, and plant pollen can provoke reactions when it comes into contact with the skin or cause symptoms of food allergy when consumed with food.
House dust mites (D. pteronyssinus, D. farinae), spores of the fungus Alternaria alternata, epithelium and animal hair (cats, dogs) are common inhalation allergens that can cause year-round allergic rhinitis, bronchial asthma, as well as exacerbations of atopic dermatitis.
Pollen from birch and meadow grasses is associated with seasonal manifestations of allergic reactions during the period of plant dusting. In spring, symptoms are more often associated with flowering trees, in June-July - with meadow (cereal) grasses, and in August-September - with weeds.
The grass pollen mixtures presented in this study include rye (Secale cereale), timothy grass (Phleum pratense), meadow fescue (Festuca elatior/pratensis), tall ryegrass (Arrhenaterum elatius), sweet grass (Anthoxanthum odoratum), and bromegrass. awnless (Bromus inermis), hedgehog (Dactylis glomerata), tares (Lolium perrene), meadow foxtail (Alopecurus pratensis), woolly milkweed (Holcus lanatus), pigtail (Cynodon dactylon). Using this parameter, the level of IgE antibodies is determined in total.
Food allergens (chicken eggs, cow's milk, peanuts, hazelnuts - hazelnuts, potatoes, carrots, wheat flour, soybeans) can provoke not only symptoms of gastrointestinal disorders (nausea, vomiting, abdominal pain, diarrhea), urticaria, angioedema , but also cause exacerbations of atopic dermatitis, respiratory forms of allergies and even severe allergic reactions up to anaphylactic shock. Food allergens are often hidden allergens in foods (eg, nuts, peanuts, eggs in confectionery and baked goods), which pose a particular danger to patients with severe anaphylactic reactions.
Allergy to the white and yolk of a chicken egg, which differ in composition and allergenic properties, is significant. The main allergens of chicken eggs are contained in the protein - ovomucoid, ovalbumin and ovotransferrin.
Ovomucoid is resistant to heat treatment and the effects of digestive enzymes, and is responsible for maintaining sensitization for many years.
The yolk of an egg is less allergenic, and if you are sensitized only to the white, it can be consumed after being washed to remove the white.
Most often, children are allergic to cow's milk proteins, the main ones being casein, alpha-lactalbumin and beta-lactoglobulins, and bovine serum albumin.
The reaction to whole cow's milk, alpha-lactalbumin and beta-lactoglobulin in the absence of sensitization to casein allows the consumption of fermented milk products in most cases.
Casein hypersensitivity does not always go away during childhood and may persist for many years into adulthood or throughout life. Bovine serum albumin is responsible for cross-reactions between cow's milk and beef.
At one time, soybeans were considered a safe ingredient in formula for infants with milk allergies, but the opposite has been found. Soy can act as a hidden allergen in various processed meats, cheeses, sauces, and sweets.
Food allergies can often be confused with food intolerance associated with other reasons (features of food preparation, product composition, metabolic disorders, gastrointestinal diseases).
The patient may have hypersensitivity to only one allergen or to several at the same time. The level of antibodies correlates to some extent with the severity of clinical manifestations of allergy symptoms, but this pattern is not always observed.
Identification of a causally significant allergen allows one to take adequate measures to limit or completely eliminate contact with it, which in most cases significantly improves the patient’s condition.
For hypersensitivity reactions to certain inhaled allergens (for example, birch pollen, meadow and weed pollen, as well as house dust mites), it is possible to use allergen-specific immunotherapy (ASIT) after 5 years of age.
The results of this analysis should be interpreted and subsequent recommendations made only by an allergist, taking into account the clinical symptoms, individual characteristics of the patient, history of his disease and other important parameters.
What is the research used for?
- Identification of sensitization to the main inhalation and food allergens in children;
- determination of a causally significant allergen in allergic rhinitis, allergic conjunctivitis, atopic bronchial asthma, atopic dermatitis, food allergies, urticaria, angioedema in children;
- prescribing rational elimination measures to reduce allergen exposure.
When is the study scheduled?
- When examining children with suspected respiratory or food allergies, manifested by some of the following symptoms: nasal congestion and rhinorrhea, nasal itching, sneezing, redness and/or itching of the eyes, cough, shortness of breath, wheezing in the lungs, skin rashes, swelling of the skin and mucous membranes , gastrointestinal disorders after taking a possible allergen;
- during dynamic observation of children with polyvalent sensitization;
- when choosing an adequate hypoallergenic diet.
What do the results mean?
Reference values, (IU/ml)
| House dust, Derm.pteronyssinus | 0.00 – 0.34 |
| House dust, Derm.farinae | 0.00 – 0.34 |
| Birch | 0.00 – 0.34 |
| Mixture of herbs: rye (Secalecereale), meadow timothy (Phleumpratense), meadow fescue (Festucaelatior pratensis), tall ryegrass (Arrhenaterumelatius), fragrant spikelet (Anthoxanthumodoratum), awnless brome (Bromusinermis), creeping wheatgrass (Agropyronrepens), hedgehog grass (Dactylisglo merata ), chaff (Lolium perrene), meadow foxtail (Alopecurus pratensis), woolly milkweed (Holcuslanatus), pig's finger (Cynodondactylon) | 0.00 – 0.34 |
| Cat | 0.00 – 0.34 |
| Dog | 0.00 – 0.34 |
| Alternaria alternate | 0.00 – 0.34 |
| Milk | 0.00 – 0.34 |
| a-lactalbumin | 0.00 – 0.34 |
| b-lactoglobulin | 0.00 – 0.34 |
| Casein | 0.00 – 0.34 |
| Egg white | 0.00 – 0.34 |
| Egg yolk | 0.00 – 0.34 |
| Bovine serum albumin | 0.00 – 0.34 |
| Soya beans | 0.00 – 0.34 |
| Carrot | 0.00 – 0.34 |
| Potato | 0.00 – 0.34 |
| Wheat flour | 0.00 – 0.34 |
| Hazelnut | 0.00 – 0.34 |
| Peanut | 0.00 – 0.34 |
Reasons for negative results:
- lack of sensitization to allergens included in this mixture;
- long-term restriction or exclusion of contact with allergens.
Important Notes
- The absence of sensitization to the allergens included in this study does not exclude the presence of allergies to other sources of allergens. In some cases, further allergy testing may be required to clarify sensitization to other possible allergens.
- The presence of allergen-specific IgE antibodies to allergens may not always be accompanied by the presence of clinical symptoms.
- The results of the analysis do not constitute a diagnosis or information for self-medication. Recommendations are made only by an allergist, taking into account the individual characteristics of the patient and the results of all studies performed.
Also recommended
[02-029] Clinical blood test with leukocyte formula and ESR [08-017] Total immunoglobulins E (IgE) in serum [21-673] ImmunoCAP ISAC allergy chip (112 allergy components) [21-845] Mixed allergy complex RIDA-screen No. 1 [21-846] Respiratory allergy complex RIDA-screen No. 2 [21-847] Food allergy complex RIDA-screen No. 3
+ determination of specific immunoglobulins class E for other allergens
Who orders the study?
Allergist, gastroenterologist, pulmonologist, otorhinolaryngologist, ophthalmologist, pediatrician, therapist, general practitioner.
Literature
- Bousquet J, Chanez P, Michel FB. The respiratory tract and food hypersensitivity. Food Allergy, Adverse Reactions to Foods and Food Additives. Metcalfe DD, Sampson HA, Simon RA. Boston, MA, USA: Blackwell Scientific Publications. 1991:139. ISBN:0-86542-094-7.
- Host A et al. Allergy testing in children: why, who, when and how? Allergy 2003;58:1-11.
- Wal JM. Cow's milk proteins/allergens. Ann Allergy Asthma lmmunol 2002;89(Suppl 1):3-10.
- Volcheck GW Clinical Allergy. Clinical Allergy: Diagnosis and Management, Mayo Foundation for Medical Education and Research. – Abington: Human Press, 2009.
- Werfel T., Breuer K. Role of food allergy in atopic dermatitis // Curr. Opin. Allergy Clin. Immunol. – 2004. – Vol.4. – P. 379-385.
Source: https://helix.ru/kb/item/21-848










