Loeffler's syndrome
Loeffler's syndrome (W. Loffler, Swiss doctor, born in 1887; synonyms: volatile pulmonary infiltrates, eosinophilic pneumonia, eosinophilic lung infiltrates) is a combination of transient pulmonary infiltrates, determined by X-ray examination, with high blood eosinophilia. Similar infiltrates are found in other organs.
First described by Leffler in 1932. It is found relatively rarely in all countries, more often in tropical countries.
Etiology. Caused by various pathogenic factors. The main etiological factor is infestation by helminths (roundworms, hookworms, trichinas, flatworms Taenia saginata, liver fluke, schistosomes, strongyloides, and cat fluke), the larvae of which migrate through the lungs. There are known cases of infection of people, especially children, by Toxocara larvae, an roundworm-like parasite of dogs and cats. Toxocara larvae migrate through the lungs, but, unlike roundworm larvae, they form cysts in the lungs, liver and other organs before reaching maturity. The migration process of these larvae may be accompanied by Loeffler's syndrome. The second group of etiological factors of Loeffler's syndrome is chemical agents and medications. There are known cases of Loeffler's syndrome with prof. contact with nickel and zinc and from many medications as with prof. contact, and during therapeutic use (penicillin, acetylsalicylic acid, sulfonamides, nitrofurans, PAS, radiocontrast agents and others). Cases of Loeffler's syndrome have been described in women who received hormonal drugs (testosterone propionate and sinestrol) in combination with radiation therapy for breast cancer. The third group of etiological factors is various exogenous allergens (plant pollen, fungal spores, tobacco and others) that cause atopic diseases of the respiratory system (see full body of knowledge Atopy). Transient eosinophilic pulmonary infiltrates are described among other manifestations of serum sickness, as well as periarteritis nodosa, which occurs with high eosinophilia; There are indications of their connection with tuberculin allergy and amoebiasis. Often the etiology of Loeffler syndrome remains unclear.
Pathogenesis. The pathogenesis of Loeffler syndrome is based on the formation of allergic eosinophilic alveolitis. The most likely is an immediate type of allergic reaction (see the full body of knowledge Allergy), which is confirmed by positive skin tests, as well as some features of the clinical course: the “volatile” nature of the infiltrates, their complete reverse development without the formation of foci of sclerosis. In some cases, it is possible to detect an increased level of IgE in the blood serum in children suffering from ascariasis, which is typical for diseases caused by immediate allergic reactions. Intense infiltration of lung tissue by eosinophils and pronounced blood eosinophilia give reason to assume that in Loeffler's syndrome, a special role in the formation of foci of allergic inflammation belongs to the eosinophilic chemotactic factor of anaphylaxis (see full body of knowledge Mediators of allergic reactions). The formation of high titers of precipitating antibodies to antigens in some cases of Loeffler's syndrome is apparently explained by the participation of allergic reactions developing according to the Arthus phenomenon (see the full body of knowledge of the Arthus phenomenon). In the experiment, eosinophilic pneumonia similar to Loeffler's syndrome was obtained in rabbits sensitized with horse serum after permissive intratracheal injection of this serum.
Clinical picture. The most characteristic clinical picture of Loeffler syndrome is infiltrates in the lungs, which are detected by X-ray examination, and blood eosinophilia (from 7 to 70%) with moderate leukocytosis. Complaints and symptoms (slight dry cough, slight malaise, weakness, sweating, low-grade fever) may be absent or very mild. Percussion with extensive infiltrates reveals a shortening of the pulmonary sound. On auscultation, small amounts of moist fine bubbling rales are occasionally heard. The upper lobe of the right lung is most often affected. A combination of eosinophilic Latin infiltrates with dry pleurisy has been described (see full body of knowledge), and there may be pain when breathing in the corresponding half of the chest and a pleural friction noise can be heard.
Symptoms of the prodromal period can occur in the form of catarrhal nasopharyngitis. Sometimes the temperature reaches 38-39°. In sputum, if it is separated, predominantly eosinophils are detected.
When eosinophilic infiltrates are localized in other organs, mild transient symptoms of damage to the corresponding organs and systems are usually observed - gastritis, pancreatitis, appendicitis, meningoencephalitis and others - in combination with blood eosinophilia.
The diagnosis is established on the basis of x-ray data with their characteristic rapid dynamics and the presence of pronounced blood eosinophilia. Loeffler's syndrome is often detected accidentally during a preventive X-ray examination.
Etiological diagnosis is more difficult; skin testing is used with allergens prepared from helminths, plant pollen, fungal spores (see full body of knowledge Skin tests); serological tests - precipitation reaction (see the complete body of knowledge) in various modifications and the complement fixation reaction (see the full body of knowledge), as well as cellular tests, such as the Shelley basophil degranulation reaction (see the complete body of knowledge Basophil test) and the mast cell degranulation reaction (see full body of knowledge) with relevant allergens. Occupational “nickel” Loeffler syndrome is usually combined with allergic contact dermatitis; a compress (application) test with nickel is positive. In cases caused by intestinal parasites, it is possible, but not always, to detect parasite eggs in the feces, that is, during primary invasion, migration of larvae through the lungs occurs before the parasites reach maturity and release eggs. However, this method can be applied in anticipation of the possibility of an invasion that precedes the one that led to the formation of Loeffler's syndrome. When infested by Toxocara larvae, the parasites do not reach maturity in the human body, so eggs are not found in feces.
All about Loeffler's syndrome
Classification of Loeffler's syndrome
Loeffler's syndrome is classified according to the causes of its occurrence. There are three main types of Loeffler syndrome:
- Loeffler's syndrome, which developed after an allergy to medications;
- Loeffler's syndrome, which was caused by infection of the human body with parasites;
- Loeffler's syndrome, which was caused after an increase in the body's sensitivity to aeroallergens.
Who is at risk for contracting Loeffler's syndrome?
Almost everyone is at risk, regardless of age or financial situation. It was also noted that Loeffler's syndrome occurs with equal frequency in both men and women. More often, this syndrome affects people aged 15 to 40 years. As for eosinophilic pneumonia, we can say that it is most common in tropical latitudes.
What symptoms are observed in patients with Loeffler's syndrome?
After observations, it was noted that the patients did not show any symptoms, they felt normal and did not complain about anything. In more rare cases, patients may be bothered by a cough; it can be either dry or a small amount of sputum; in very rare cases, blood has been noticed in the sputum. The patient's temperature can remain at 37-37.5 degrees for a long period of time. In almost all cases, cough manifests itself in combination with bronchospasm.
Symptoms
Eosinophilic pneumonia is divided into three types of process: simple , acute and chronic . With a simple type of inflammation, associated with the presence of HIV and tobacco smoking, the symptoms are mild.
The main features include:
- increase in body temperature to low levels,
- rare dry cough, sometimes with sputum mixed with blood,
- slight pain in the trachea area,
- general weakness and increased fatigue.
As the parasitic attachment progresses, rashes appear on the body, accompanied by itching. The illness lasts from several days to two weeks.
With an acute type of inflammation , the body temperature rises sharply, the cough intensifies, becomes paroxysmal, and the person feels unwell and drowsy. This type of pneumonia passes with all the signs of severe intoxication. This course is characterized by signs of respiratory failure. Breathing becomes incomplete and weak, wheezing appears. All symptoms are accompanied by dull pain in the sternum and muscle myalgia. The causes may be helminthiasis, allergic reactions to medications, poisoning with nickel salts and mycoses. This condition can last from several days to a month.
The chronic form (Carrington syndrome) manifests itself with less pronounced symptoms.
Occurs predominantly in women of fertile age (after 40). The pathological process in the lungs increases slowly, but almost always leads to respiratory failure. The impetus for development may be the presence of bronchial asthma or allergic rhinitis. Symptoms of this disease are dry cough, sweating, shortness of breath, anemia, weight loss, hepatomegaly, swollen lymph nodes and fever. X-ray images reveal the presence of diffuse infiltration. The disease lasts from four weeks to several months, relapses are possible.
Loeffler's syndrome
Loeffler's syndrome is another allergic disease that occurs when the number of eosinophils in the patient's blood increases. At the next stage, an infiltrate develops in one or both lungs and as a result, the patient develops a disease such as pneumonia.
In fact, the first and second syndromes are distinguished:
For the most part, the disease most often occurs in adults aged 16 to 40 years. Men and women suffer from the disease with equal frequency. The most favorable place for the disease to occur is the subtropics. More often than others, people who suffer from other allergic reactions and have an increased sensitivity threshold are susceptible to developing the disease. [contents]
Etiology
There are no exact causes of eosinophilic pneumonia, but there are known signs of this disease. These include:
- Hypersensitive reaction of the body to foreign allergens (sensitization).
- Sensitization of the respiratory system to fungal spores.
- Helminthiases.
- Immunological deficiency syndrome (HIV).
- Systemic connective tissue diseases.
- Churg-Strauss syndrome. It is a type of systemic vasculitis affecting small and large vessels of the respiratory tract. Histological diagnosis reveals eosinophilic infiltrates. The cause may be a viral or bacterial infection (such as hepatitis B or staphylococcal infection of the nasopharynx).
Causes of the syndrome
The syndrome was first described by Wilhelm Leffler in 1932. The professor was employed at the University of Zurich and at that time carried out studies of lung tissue for inflammation through helminthization. Over time, this disease developed into pneumonia and pneumonia. The disease can occur at any time when almost any parasite enters the body: pinworms, trichinella, cat fluke and other organisms. Recently, toxocariasis, which develops due to intestinal parasites of domestic animals, has become very widespread. With this disease, inhalation allergens appear that enter the human body through inhalation. However, much more often, the appearance of the syndrome is provoked by an as yet unstudied allergen, and sometimes medicine cannot identify the disease and offer the optimal treatment method.
Diagnosis of the disease
Identifying the disease is not difficult. This is because a typical sign of the disease is high eosinophils in the patient's blood. Also, in addition to the main symptom, there are volatile pulmonary infiltrates. However, difficulties arise. This is due to the presence of such manifestations as:
If there are suspicions of other diseases, then the allergist should refer the sick person for examination to other specialists, for example, to an otolaryngologist if seasonal rhinitis is suspected.
Eosinophils in a blood test.
How is the disease detected in the laboratory?
Laboratory tests are not just necessary, but are a prerequisite for treating the syndrome. The information obtained as a result of the examination helps determine the complexity of the disease and draw up a further treatment plan. As noted earlier, the patient’s body is examined for the presence of eosinophils. To obtain the desired results, specialists take a sputum sample and do a general blood test. In addition to identifying allergenic proteins, obtaining information about the presence of Charcot-Leyden crystals is added.
If there are more than 20% eosinophils in the patient’s blood, then we can talk about the presence of Loeffler’s syndrome. However, there is a small nuance that any doctor should know. After the disease becomes chronic, the level of eosinophils returns to normal, and testing the blood for this compound no longer makes sense. During this period, a blood test should be done to check for the presence of immunoglobulins.
Skin tests are also carried out, which are aimed at identifying the causative agent of the disease: harmful spores, pollen, helminths. In some cases, the doctor prescribes inhalation and nasal tests. Stool analysis is mandatory. This provides information about the presence of helminths and other parasites in the patient’s body. At the same time, the doctor also determines the development cycle of parasites, since, for example, roundworms invade the human lungs one to two weeks after appearing in the body. With toxocariasis, parasite larvae may not be isolated at all, since these helminths do not develop to adulthood.
Serological tests are often used to determine specific types of immunoglobulins. It also happens that doctors prescribe x-rays, where infiltration can be immediately noticed. After this, additional bronchomotor tests are performed to determine the presence of asthmatic symptoms.
Diagnostics
Treatment for the disease can be prescribed only after diagnosis. It includes several manipulations.
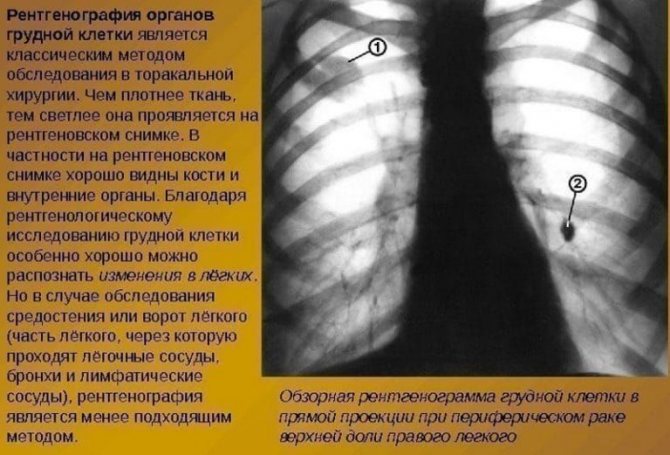
X-ray to diagnose pneumonia
Radiography. In the presence of pathology, the procedure will allow one to identify single, subpleurally located darkenings with unclear contours, the intensity of which is moderate, and the shape is irregular. The diameter of the formations can reach 3–4 centimeters. The pulmonary pattern surrounded by infiltrate is more pronounced. No later than 2 weeks from the moment of detection, the infiltrates disappear, but before that they migrate through the pulmonary fields. If the inflammation does not go away, then cysts and fibrotic foci may form in the tissues.
General blood analysis. The initial stage of the disease in most cases is characterized by leukocytosis and an increased number of eosinophils. The percentage of excess can reach 20–25%.
Allergy tests. Includes nasal and inhalation procedures and skin tests. The purpose of the tests is to identify pollen allergens, fungal spores, and helminths. It is important that an allergy to nickel salts is almost always combined with contact dermatitis.

Analysis of stool for the presence of parasite eggs. If the described pathology is present, worm eggs should be detected in a stool analysis.
Bronchoalveolar lavage. In the lavage fluid, the appearance of eosinophils is noted, the concentration of which exceeds the norm by 40% or even more.
Patients suffering from chronic eosinophilic pneumonia most often have a history of allergic reactions. If the disease is accompanied by atopic complications, the patient is recommended to consult an allergist; if accompanied by respiratory rhinitis, a visit to an otolaryngologist is necessary.
How to treat the syndrome?
It happens that a sick person recovers independently and completely unexpectedly, while he has not yet started drug treatment. This can only be done if the parasites that cause the disease are removed from the body. In other words, deworming is carried out. In this case, the patient is prescribed antiparasitic medications, such as:
If a lasting effect has not been achieved, then the doctor prescribes a course of antihistamines, the mechanism of which works based on the suppression of histamine formations secreted by the body. It is not recommended to resort to a course of corticosteroids, since these drugs contribute to the appearance and increase in the volume of infiltrates in the lungs, which complicates further diagnosis of the disease. These remedies are used only when a person recovers. Prednisolone is usually prescribed up to 20 mg per day. Every other day, the dosage is reduced by 5 mg, and then the daily dose is divided into three parts. Taking the drug lasts about a week.
ATTENTION! Don't self-medicate! It is impossible to exclude contacting a specialist when the first symptoms are detected!
If there are broncho-obstructive signs, then the following methods are used as treatment:
Treatment
Pulmonary eosinophilia in some cases does not require special treatment. But it happens that there is no way to do without therapy, then drugs are selected that eliminate the cause and symptoms of pathological inflammation. For complex treatment, glucocorticoids, bronchodilators, antihistamines and expectorants are used.
An important point in eliminating the causative factor is deworming and specific hyposensitization.
If eosinophilic damage to the lung tissue is associated with other diseases, immediate therapy is necessary.
Regression of symptoms in eosinophilic pneumonia is achieved mainly through the use of corticosteroids. Literally two days of treatment is enough to eliminate severe inflammation. Corticosteroids are given orally or intravenously. Among oral medications, prednisone has proven itself well; methylprednisolone is usually injected into a vein. For relapses of eosinophilic pneumonia, fluticasone is recommended (inhalation administration of the drug).

Prednisone is recommended to be taken once a day, the dose of the drug is 40-60 mg.
In pediatrics, prednisone is prescribed at a rate of 1-2 mg/kg/day in 2-3 doses.
If the patient has signs of respiratory failure, methylprednisolone is indicated. It is administered intravenously every 6 hours. Dose calculation – 60-125 mg (for adults) or as prescribed by the doctor.
Important! Despite the elimination of the acute form of the disease with hormonal agents, therapy continues for a long time. In each specific case, drugs for further rehabilitation are selected only by a pulmonologist . Read more about rehabilitation measures >,>,
Prevention of Loeffler's syndrome
As a preventive measure, a person susceptible to such diseases should periodically visit an allergist and other specialists. It is very important to observe all hygiene measures, and also to communicate less with pets. It is worth acquiring a standard set of medications aimed at preventing drug allergies. If the allergy occurs at the place of work, you should change it.
As a result, it can be noted that Loeffler's syndrome is not a critical and particularly dangerous disease that cannot be treated. On the contrary, the disease can be treated quite easily, provided that the patient fulfills all the requirements set by the doctor and in compliance with basic hygiene standards. The particular danger of the disease is that it can provoke severe complications such as pneumonia or bronchial asthma. Getting rid of these diseases is much more difficult. In order not to bring the patient to such a state, you should immediately consult a doctor, undergo an examination and begin the prescribed course of treatment.











