Hello, dear readers. Today we will talk about respiratory allergies in children .
How to recognize this insidious disease that awaits your baby? How to distinguish it from a regular viral infection?
Which children are at risk? What are the ways to treat and prevent respiratory allergies? How to protect children from dangerous diseases?
Respiratory allergies are a complex of allergic diseases of the upper respiratory tract.
Respiratory allergies can affect individual areas (nasopharynx, bronchi, trachea, etc.) and the entire respiratory system.
Most often, respiratory allergosis occurs in children with a family history (parents suffered from allergies), and in infants who, for some reason, cannot receive breast milk.
And also in children 2-4 years old as a reaction of the immune system to food products or elements of cosmetics introduced for the first time.
Also at risk are children with weakened immune systems due to frequent colds or intestinal disorders.
Symptoms of respiratory allergosis are similar to those of viral respiratory tract infections:
- itching and burning in the nose and throat;
- cough, sneezing;
- nasal congestion, watery or mucous discharge;
- sore throat, swelling;
- redness of the eyes, tearing.
As you can see, the symptoms are very similar to a common viral infection.
Sometimes parents do not pay due attention to the listed signs, they say, “all children get sick, who grew up without a runny nose?”
But if respiratory allergosis is not treated in time, serious complications can begin: conjunctivitis, laryngitis, bronchial asthma, Quincke's edema.
How to distinguish respiratory allergosis from a viral infection? As a rule, with a viral infection, these symptoms appear gradually, with an increasing effect; with respiratory allergosis, they appear quite quickly and immediately.
In addition, a child suffering from respiratory allergosis does not have an increase in body temperature, good appetite, and there is no lethargy, moodiness or other signs of the patient.
Often the disease “gives out” an abrupt course. For example, you notice that the attacks worsen after visiting the neighbor’s children (and there is a kitten in that apartment), or while cleaning the apartment, or after going to the circus, etc.
Briefly about the main thing
Simply put, an allergy is the body’s response to an irritant.
As you know, our immunity has various kinds of protective means, thanks to which dangerous substances are perceived as suspicious and neutralized.
In some cases, the immune system may perceive quite ordinary, ordinary elements as threatening and develop certain antibodies to them. When the body comes into contact with these substances a second time, an allergic reaction will occur.
Classification
In accordance with the International Classification of Diseases, 10th revision (ICD-10), respiratory allergosis has a specific designation. This indicates that this type of illness is very common and requires certain medical intervention.
ICD code for respiratory allergosis: J40 – J47. The disease is included in the section “Chronic diseases of the lower respiratory tract”. This indicates that the disease can have a long and protracted course.
According to the ICD, respiratory allergosis may have some signs and symptoms of such serious diseases as bronchitis, asthma and others.
Possible complications
The disease is especially dangerous because it can become chronic with the development of bronchial asthma.
In severe cases, a life-threatening condition may occur.
In order to avoid such a disease, a number of preventive measures are necessary:
- It comes down to limiting contact with the allergen . To do this, you need to know exactly the time of flowering of herbs and trees, if possible, plan a vacation away from places where they grow, and carefully select products taking into account the chemical composition.
- During an exacerbation of the disease, introduce a hypoallergenic diet with a limitation of possible irritants.
- Clean the cavities of the upper respiratory tract more often , since it is on them that foreign particles can be deposited. For this you can use pure distilled water.
- Do not self-medicate , but at the first suspicious symptoms, seek help from qualified specialists.
Modern methods of treatment
Treatment of allergosis in children
Recommendations in the presence of this disease, first of all, consist in maximally limiting the patient’s contact with allergens that provoke the disease.
The most commonly used medications are antihistamines or hormonal drugs. Allergic rhinitis, for example, as prescribed by a doctor, various aerosols containing corticosteroids are used to relieve swelling of the nasal passages. The most commonly used antihistamine drugs are Suprastin, Zyrtec, Zodak and others.
Along with the listed drugs, vitamin therapy and a variety of physiotherapeutic procedures are actively used. Regardless of the nature of the symptoms, some bronchodilators in the form of inhalations or tablets are used to alleviate the situation.
The most modern treatment methods include allergen-specific immunotherapy (ASIT). With this method, substances that contain certain allergens (those that cause allergies) are introduced into the patient's body, gradually increasing the dose. The body gradually gets used to the stimulus and stops reacting to it. Perhaps this can be called the only way to treat, and not alleviate the condition. True, ASIT can only be performed from the age of five.
Types of disease
In medicine, respiratory allergies are divided into infectious and non-infectious.
The first type of disease is caused by infectious pathogens (bacteria, mold, fungi, viruses).
The second type of disease can be triggered by non-infectious irritants. They are differentiated into:
- household (house dust, which carries the excreta of mites and cockroaches and can be found everywhere - in carpets, toys and even on the bed);
- pollen (poplar fluff, mold spores, plant and flower pollen);
- food (most often found in fruits, chocolate, etc.);
- medicinal (this may include some antibiotics, antiseptics and even painkillers);
- chemical (chemicals, preservatives, some cleaning products and detergents, and even cosmetics).
What are the main manifestations of respiratory allergies?
Etiology
The causes of the development of the disease are the following factors:
- Hereditary. If the pathology is diagnosed in one of the parents, the risk of its development in the child increases.
- The impact of allergens on the body. The most common triggers are: street and house dust, pollen from flowering plants and herbs, mold spores, medications, pet hair, fluff and feathers from pillows, household chemicals, face and body care products, food.
- Poor environmental conditions. Living in large cities increases the risk of allergies.
- Frequent respiratory diseases. Untimely treatment can contribute to the development of allergosis.
The presence of one or more factors significantly increases the likelihood of pathology formation.
Respiratory allergies - let's restore free breathing
Respiratory allergy is an inadequate, intense pathological immune reaction of the body to the penetration of allergens into the mucous membrane of the respiratory tract.
The term allergen refers to various third-party substances or exposure factors that provoke the occurrence of such a painful reaction of the immune system.
The respiratory form means that allergens enter the mucous membrane when breathing.
Microscopic pathogens are in the air, and when we breathe they get inside, attacking the mucous membrane of the nose and throat. Hence the name - aeroallergens.
The onset of a respiratory allergic reaction occurs if there is contact with an allergen to which a person has developed hypersensitivity. The immune system, perceiving a harmless factor (foreign body) as a serious danger, begins to protect and “attack” the pathogen.
The key problem of any type of allergy is the body’s excessive, overly aggressive response to the antigen, in contrast to the normal immune reaction.
The disease occurs in different ways, for some allergy sufferers it is limited to minor discomfort (inconvenience).
Manifested by itching, runny nose. However, in some situations, such an immune disorder can cause a real threat, causing significant damage to organs and tissues. An example is the risk of anaphylactic shock.
List of typical aeroallergens:
- house dust
- plant pollen
- epithelium of insects, domestic animals
- fungal spores
- household chemicals
- cosmetics
- varnishes, paints
In addition, the following are recognized as possible catalysts for an allergic reaction:
- food products
- sunlight
- cold
- stinging insect venom
Along with the respiratory form manifested (asthma, allergic rhinitis, hay fever, conjunctivitis), other, fairly “popular” types of allergosis are classified:
When choosing treatment tactics, the following are taken into account:
- factor that causes an allergic response from the immune system
- clinical manifestations of the disease
Do not try to solve this problem on your own; use only your doctor’s recommendations. Be sure to consult an allergist before using folk remedies; self-medication without consultation with a doctor is unacceptable.
The body becomes familiar with respiratory allergies most often in childhood or adolescence.
In an adult, such immunity disorders (failures) are possible as a negative consequence of a history of respiratory tract pathology.
Exacerbations (attacks) occur in 2-3 quarters of the year, since in the spring-summer season the air is oversaturated with odors and pollen.
Respiratory allergies
There are two basic types that manifest this type of immune disorder:
- Bronchial asthma is a common type of respiratory allergic reaction. Due to inflammation and swelling, at the time of an asthma attack, the bronchi “narrow” in an asthmatic, causing noticeable breathing difficulties during the exhalation phase.
- Allergic rhinitis is a runny nose of a non-infectious nature, lacrimation, redness of the eyes.
The symptomatic picture is supplemented by:
- cough
- sneeze
- swelling of the eyelids, throat
- mucosal irritation
In allergic rhinitis, there are two pathology scenarios:
- Seasonal - probable exacerbations occur in spring and summer, the allergen is pollen and the smell of flowering plants.
- Year-round - nasal congestion, sneezing, lacrimation become systematic, the disease receives a permanent, year-round “registration” in the body. To these characteristic clinical manifestations are added general signs of malaise: rapid pulse, increased sweating. The catalyst for problems is often factors that we encounter on a daily basis. These include house dust, animal hair, and fungal spores.
Complete elimination of contact with the identified irritant is a fundamental condition for successful treatment of allergic rhinitis.
In most cases, the patient knows what causes such problems. By his actions, a person tries to minimize or completely eliminate the “encounter” with the allergen.
Conventionally, it is permissible to consider angioedema as a manifestation of respiratory allergy, when the swelling “affects” the mucous membrane of the respiratory tract.
Treatment of allergosis
The therapeutic process requires an integrated approach; it is necessary to correctly diagnose the allergen causing the reaction.
If the doctor was unable to immediately determine the cause, then laboratory tests are carried out:
- clinical blood test
- tests, samples for various antigens
After accurately identifying the irritant, the necessary antihistamines are prescribed. Medicines normalize the functioning of the immune system and help the body quickly get rid of (remove) antigens. Among medical prescriptions are antihistamines of four generations:
- first - Suprastin, Fenkarol, Tavegil
- second - Claritin, Kistin Zodak (drugs contraindicated for heart patients)
- third - Telfast, Zyrtec, Cetrin
- fourth - Erius, Desloratadine, Ebastine, Cetirizine
The selection of the drug and the choice of treatment tactics (dosage regimen) are carried out by an allergist, always taking into account the severity, nature of the disease and the age of the patient.
Since the treatment is complex, if necessary, the following is included in therapy:
- local treatments - ointments, drops, sprays
- physiotherapeutic procedures
Therapeutic measures for allergies are necessarily accompanied by strengthening the immune system.
Unfortunately, not everyone strictly follows the doctor’s instructions.
Many, after initial improvements and relief of symptoms, independently adjust the dosage, or, considering themselves recovered, completely stop taking the prescribed medications. This is a gross and unacceptable mistake.
Some people take antihistamines uncontrollably for a long period of time, mistakenly believing that this will cure them.
The final result is disappointing - allergic problems worsen, respiratory diseases intensify, becoming chronic.
The conclusion is simple - be sure to follow the doctor’s recommendations; independent medical manipulations are categorically unacceptable.
Folk recipes
The use of recipes requires caution, taking into account the individual response of the body to the components.
Consultation with your doctor is required!
In the recipes described below, we will focus on the fight against allergic rhinitis - a “popular” form of respiratory allergy.
Aloe
Drops from herbal components are an adequate replacement for vasoconstrictors, the use of which is limited due to mucosal degeneration. Take topically, orally.
Beneficial features
- The plant has a positive effect on the immune system, which provides significant support for allergies of various natures.
- The healing qualities are due to the rich content of biogenic stimulants - they accelerate the processes of growth and tissue regeneration (restoration). They activate vital processes, which enhances overall resistance to disease.
Aloe composition contains:
- phytoncides
- antioxidants
- polysaccharides
- beta carotene
- vitamin C, B, PP, E
- enzymes
Aloe juice is a reliable protection against viruses and bacteria; it is permissible to take:
- locally (drops) - eliminates swelling, inflammation, helps protect the mucous membrane from infections
- inside - normalizes digestive processes, which experience difficulties with enzyme deficiency, characteristic of food allergies
Antiseptic properties help against:
- burns, cuts
- boils, acne
- purulent inflammation
- eczema
- dermatitis
How to cook?
First leave the plant on a “starvation diet”, do not water it for a week, then the concentration of active substances will increase.
We place the cut leaves in the refrigerator - unfavorable conditions “force” the plant body to produce biogenic stimulants.
Ten days later, the foliage is thoroughly crushed, after being washed with cold water. Using a thick gauze layer, squeeze out, then boil for three minutes.
Useful qualities do not last long. Take freshly squeezed orally, diluting 100 ml with water, single serving 30 ml. The course is three weeks.
Contraindications
- hypertension
- haemorrhoids
- polyps
- fibrous formations
- liver pathology
Sea buckthorn oil
An auxiliary natural component that prevents the growth of bacteria. Eliminates dry mucous membranes that occur after vasoconstrictor drops.
The consistency is thick, the oil “gently” envelops the mucous membrane, inflammation subsides. As a result, swelling gradually subsides and the amount of secretion produced decreases. Nasal breathing is normalized.
Oil properties
- antioxidant
- regenerating
- antimicrobial
Honeycomb
Useful qualities are due to the composition:
- vitamins
- mineral acids, substances
- simple sugars (glucose, fructose)
- fats
- starch
There are diametrically opposed points of view about the benefits and harms of honey for allergy sufferers. The truth “sits” approximately in the middle, since allergies are an individual pathology.
Allergens vary among patients, so it is necessary to evaluate the possibility of using honey separately in each specific situation.
Previously, beekeeping products were clearly included in the list of active allergens that were categorically unacceptable for allergy sufferers.
However, honey is able to “qualitatively” strengthen the immune system, which is fundamentally necessary for allergic pathologies.
The percentage of patients with a “direct” (immediate) allergy to honey is insignificant. The connection between an allergic reaction and the pollen of plants from which the bee takes bribes is much stronger.
The main thing is to choose the right honey plant, using special testing that allows you to determine the degree of allergic influence of the plant on the body. Linden honey is considered the most “calm”.
If there are no such problems, the body perceives honey products normally, then they must be included in the treatment of allergies. After all, they “work” by restoring the immune system, saturating the body with valuable microelements and minerals.
Regular chewing of honeycombs will help treat a runny nose (allergic is no exception), removing negative symptoms.
The course is long, the treatment interval is six months, but the effort expended will not be in vain, the risks of exacerbation of allergic rhinitis will be minimized.
The effectiveness of the therapy can last up to five years.
If, with the onset of seasonal exacerbation, the symptomatic manifestations of respiratory allergies are clear and pronounced, then preparatory preventive “work” must be started in advance.
In advance, before the onset of exacerbations, use according to Art. l. honeycomb honey
Until the allergy symptoms subside, continue to eat honeycomb honey, drink honey water, and chew the wax caps more often if necessary.
A reasonable combination of the above-mentioned actions contributes to the effective fight against non-infectious rhinitis.
Black elderberry
The berry helps with exacerbations of hay fever, restoring and strengthening the immune system. It is acceptable to use alone or in combination with other medicinal plants.
The chemical composition is enriched with flavonoids (strong antioxidants), more than in blueberries and cranberries.
Useful qualities:
- increases hemoglobin
- cleanses the blood
- enhances liver function
How to make elderberry juice
Select ripe fruits, wash, and pour boiling water for ten minutes. Then, pour into a colander, grind, squeeze out the juice, add sugar at the rate of 300 g. per kilogram of berries. Bring the resulting mixture of juice and sugar to a boil, fill pre-sterilized containers, and close with a lid. For exacerbations, take a tablespoon three times a day.
Herbal remedy for runny nose
The recipe is simple, but it can “support” the body in moments of struggle against respiratory allergies.
Required components:
- burdock rhizome, dandelion, nettle - 4 parts
- strawberry leaf - 3
- wormwood - 2
Grind thoroughly, mix, and brew in a thermos. One tbsp. l. collection per 300 ml. After steeping overnight, strain in the morning and drink in equal portions throughout the day.
Be patient, take two two-week courses, with breaks of thirty days.
In the future, keep your runny nose under control by repeating the course every year.
Source: https://life5plus.ru/allergiya/respiratornaya-allergiya.html
Signs of illness
The body's reaction to various pathogens is purely individual. That is, for each individual patient, the symptoms of respiratory allergosis may differ from each other in intensity and totality. However, most often the manifestation of this disease comes down to the following:
- itchy throat;
- stuffy nose, runny nose;
- frequent sneezing;
- a feeling of swelling in the throat, tongue and eyelids;
- dry cough;
- drowsiness.
In accordance with the symptoms listed above, several forms of the disease are distinguished.
Important to remember
- If there are allergy sufferers in your family, if the child was deprived of mother's milk, was often sick or suffered from intestinal infections, he is at risk and may develop respiratory allergosis.
- If a baby suddenly starts coughing, runny nose, itching and burning in the nose, throat, eyes (while the temperature, appetite, mood are normal), and then everything stops just as quickly - these are symptoms of respiratory allergosis, and therefore a serious reason to contact pediatrician
- If a child has been diagnosed with respiratory allergosis, you cannot limit yourself to antihistamines. Complex treatment is required.
We wish you and your children health!
Types, causes and symptoms of respiratory allergies. Methods for treating respiratory allergosis with medications, local remedies and folk methods.
Types of ailments
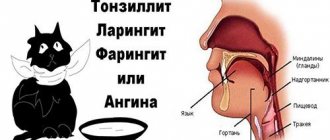
Respiratory allergosis (ICD code: J40 – J47) manifests itself in the form of such common ailments as:
- pharyngitis (swelling of the tongue and nasopharynx, sensation of a lump in the throat);
- rhinitis (stuffiness and itching in the nasopharynx, constant sneezing, lacrimation);
- laryngitis (swelling of the throat, hoarse voice, cough);
- obstructive bronchitis (dry cough, difficulty breathing, frequent sneezing, nasopharyngeal congestion);
- tracheitis (prolonged dry cough, worse at night, pain in the chest, hoarse voice).
How does the disease manifest itself?

Respiratory allergosis in children manifests itself in different ways. Symptoms depend on the location of the reaction and the type of stimulus:
- Allergic rhinitis most often manifests itself in childhood. In this case, the baby experiences congestion in the nasal passages with a relatively small amount of mucous discharge from the nose. All this is accompanied by conjunctivitis. The baby complains of an itchy nose and often sneezes. A headache and general malaise appear. Most often, allergic rhinitis torments young patients during flowering plants, but this deviation can occur year-round.
- Allergic pharyngitis manifests itself in the form of extensive swelling of the mucous tissues of the oropharynx. Sometimes the tongue area also becomes inflamed. Children often complain of a feeling of a foreign object, a “lump in the throat.” The process is accompanied by a strong dry cough.
- Allergic tracheitis causes hoarseness. The patient suffers from a strong dry cough (especially at night) and chest pain.
- The most common manifestation of allergies is allergic obstructive bronchitis. In this case, only the lower respiratory tract is involved in the process. Mild bronchial asthma may develop.
- Clinical manifestations of allergic laryngitis are barking cough, hoarse voice and laryngeal swelling.
Drug therapy
First of all, you should see a therapist. You may also need to consult an allergist. Then the patient will be recommended to undergo special tests to find out which substance is perceived by the immune system as an irritant.
When the allergen is identified, the patient will be advised to completely or partially exclude any contact with the pathogen. In most cases, this will be enough for recovery.
But what to do if the disease turns out to be advanced or it is not possible to completely eliminate its cause? Then the patient is prescribed complex drug therapy.
Treatment of respiratory allergosis will be carried out in several directions:
- Local medications that will relieve negative symptoms (drops in the nose or on the mucous membranes of the eyes, gargling).
- Antiallergic drugs. For mild forms - Telfast, Zyrtec, Erius; for acute - “Diphenhydramine”, “Diazolin”, “Suprastin”, “Tavegil”.
- Sorbents. Used to remove toxins from the intestines. Activated or white carbon, Enterosgel, Smecta, etc. are prescribed.
- Prebiotics. Used to normalize intestinal microflora and increase local immunity. Lactacid, Lactovit, and Duphalac are used for these purposes.
Risk factors
There are many circumstances that contribute to the occurrence of a respiratory form of allergy. They can have both a complex effect on the body and act as a single cause.
Factors provoking specific immune reactions:
- Hereditary. If one of your immediate relatives has an allergy, then the child will inherit this predisposition in 50% of cases.
- Ecological – unfavorable environment. Every year the atmosphere becomes polluted, the air becomes saturated with allergens, and the human body weakens. Constant exposure to antigens, especially on a child’s body, increases the chances of becoming sensitized.
- Harmful working conditions – constant contact with allergens.
- A decrease in the protective functions of the immune system against the background of diseases: regular exacerbations of chronic diseases, acute infectious pathologies of the upper respiratory tract, ARVI. In moments of illness, the body is most vulnerable.
- Incorrect behavior of parents - untimely introduction of a new product to the child, premature cessation of breastfeeding
- Taking medications, in particular antibiotic therapy. Certain medications may not be suitable for each person individually.
- Incorrect selection of cosmetics and household chemicals.
- Immaturity of the body (applies exclusively to children). The immune system, which is not yet fully formed, may react incorrectly; as you grow older, the problem may disappear on its own.
- Emotional stress.
- Bad habits, especially smoking. A child's body can act as a passive smoker - this is an extremely dangerous role for a baby.
Respiratory allergosis in children
This diagnosis is overwhelmingly given to children. Some people live with allergies for a long time, but many manage to overcome it and forget it in their youth.
It is worth noting that the symptoms, diagnostic methods and treatment stages for children and adults are no different. The only exceptions may be very young patients, under the age of 5 years. For such patients, the use of certain medications and several treatment procedures is excluded.
If a child suffers from respiratory allergy, then his parents should adhere to the following rules to protect him from contact with irritants:
- Visit new premises with caution (cafes, clubs, game rooms, shops and theaters);
- Use only hypoallergenic household chemicals and fragrance-free cosmetics;
- Do not experiment with new perfumes, but use only those that do not cause a reaction in the child;
- During repairs or general cleaning, take the child to another place, since household dust is a causative agent of the reaction;
- Spices can also be allergens, so when preparing an exotic dish it is important that the child is not in the kitchen;
- During flowering, if possible, take the allergic person to a place where it will be easier for him. Also, do not plant flowers in the house or arrange bouquets;
- Before buying a new thing: toys, carpet, clothes, etc. , - it is important to be sure that the child will not develop an allergy to new clothes;
- Do not have pets or visit guests who have them. It must be remembered that even dog or fish food can cause an allergy;
- Do not give your child untested medications;
- Don't offer new food.
Causes of non-infectious allergies
prolonged artificial feeding of the child, passion for products with a high content of artificial preservatives.
In addition, inhalation of polluted air when living in close proximity to industrial facilities or busy highways, long-term treatment with medications, and frequent respiratory diseases have a negative impact and contribute to the occurrence of allergies. Respiratory allergosis is very common in children. If for the smallest of them the most common allergens are food products: cow's milk, oranges, berries, chocolate, then in schoolchildren increased sensitivity is observed to household irritants, such as dust, animal hair, tobacco smoke, and plant pollen.
Respiratory allergies often occur under the influence of house dust. It contains microscopic mites, mold fungi, wool, animal down and feathers, particles of epidermis, book dust, various chemicals: cleaning products and washing powders, cosmetics. Often for various medications: vitamins, antibiotics, antiseptics, aspirin, novocaine.
In addition to non-infectious sources of allergies, there are also infectious ones, which are various microorganisms: bacteria, viruses, fungi. Foci of chronic infections in the body may well serve as sources of increased sensitivity and the subsequent development of allergies. In general, susceptibility to several substances often occurs, rather than to just one, and this series tends to expand throughout life.
Allergic rhinitis is perhaps the most common respiratory allergosis, the symptoms of which include nasal congestion, itching, sneezing, watery secretions and tearing along with swelling of the mucous membranes of the nasal cavity. It is often seasonal in nature, but can also be year-round, occurring both independently and in combination with sinusitis and otitis.
Characterized by swelling of the pharyngeal mucosa. There may be painful sensations when swallowing, a feeling of a foreign object in the throat, a dry cough. Along with pharyngitis, allergic tonsillitis and laryngitis are often observed.
Respiratory allergies also include pathologies such as allergic tracheitis. It involves attacks of an obsessive, painful, dry cough, like whooping cough, mainly at night. Fever and even vomiting are possible.
Allergic bronchitis is a protracted disease characterized by frequent relapses. The general condition of a person may be painful, and the temperature may be elevated. The nature of the cough changes over the course of the disease from dry to wet; wheezing in the bronchi is clearly audible when inhaling, but there are no attacks of suffocation. In the case of allergic obstructive bronchitis, because there is a narrowing of the bronchi.

Continues the list of diseases such as respiratory allergies and allergic pneumonia. This is the most severe form of damage to the respiratory system, which basically has an allergic reaction due to the body’s hypersensitivity to a particular irritant. With this disease, cough, shortness of breath, chills, and general weakness are observed.
Correct recognition of the allergic cause of respiratory tract diseases is possible only with a complete analysis of all data. As a rule, the course of such diseases is protracted, with constant relapses. The allergic nature of such pathologies is indicated by certain changes in the composition of the blood, the results of special samples and tests.
Treatment of respiratory allergies comes down primarily to limiting contact with the allergen, and this requires its correct identification. If it is difficult to understand on your own what exactly caused the pathological process, you cannot do without consulting an allergist who will conduct the necessary tests.
Drug treatment is carried out using antihistamines in combination with enterosorbents and prebiotics. If necessary, symptomatic therapy is carried out, which consists of taking temperature-reducing medications and painkillers. Physiotherapy gives good results: baths and inhalations, as well as treatment by staying in the microclimate of salt caves.
The same approach is applied if it is necessary to prevent respiratory allergy in children. Treatment consists, first of all, of preventing contact between the child and the irritant, be it some product, dust, tobacco smoke, chemical or medication, following a hypoallergenic diet, and carrying out vitamin therapy.
The best prevention of allergies is to strengthen the immune system by all means, exercise and breathing exercises. If there is a danger of hereditary hypersensitivity to various irritants, the expectant mother should adhere to a diet even during pregnancy, and after the birth of the baby, do not transfer him to artificial feeding for as long as possible.
Respiratory allergosis is a combination of various pathologies through which the respiratory tract is damaged due to interaction with the source of the allergy. The disease can occur in a child or an adult. But, in most cases, it is observed in children 2-4 years of age. The use of treatment is aimed at eliminating the symptoms of this pathology.
- nasopharynx;
- larynx;
- trachea;
- bronchi.
If the allergy penetrates through infection, the activity of the respiratory organs undergoes some changes due to the penetration of bacteria, viruses or foreign elements.
- symptoms appear due to the penetration of allergens, which include: plant or grass pollen, dust particles with elements contained in it, mites and pet hair;
- irritation occurs as a result of exposure to food allergens on the body;
- the development of allergic diseases is associated with the use of certain medications;
- Often, symptoms of respiratory damage appear due to close interaction with chemicals and cosmetics.
Depending on the presence of certain causes, a sick person requires immediate examination in a medical facility.
Based on the results, the necessary treatment is compiled only by a specialist in this field.
Respiratory allergosis in children can manifest itself through various forms, which have some features in eliminating the source of infection.
Often, the signs of respiratory allergosis are compared with acute respiratory viral infections. As a result, incorrect treatment is prescribed, which can cause serious complications.
- if the baby has allergies, then his physical activity does not differ in any changes;
- the child’s appetite is good, no problems are observed;
- there is no high body temperature characteristic of ARVI;
- the periods of wakefulness and sleep are not disturbed, activity and mobility are the same as in healthy people.
An essential feature of respiratory tract diseases is the nature of their occurrence. That is why, when observing the first symptoms of respiratory damage, it is necessary to seek help from a specialist.
Basically, they appear some time after certain actions that can cause the development of the disease. But with ARVI, the state of health worsens after some time.
When respiratory allergosis is diagnosed in children, treatment occurs with the use of certain antihistamines, which must be prescribed by a doctor. A specialist can prescribe medications that are produced in the first, second or third generation. Thus, drugs that have an antihistamine effect include:
- Suprastin.
- Gistalong.
- Claritin.
- Telfast.
- Diazolin.
For young children, therapeutic measures are carried out using special drops. These include Zyrtec, Fenistil and Zodak. However, in case of serious complications, Suprastin is still used, and the dosage of the drug will be calculated taking into account the age of the baby. In addition, therapeutic actions aimed at accelerating recovery are suggested.
- Nazivin.
- Otrivin.
- Tizin.
They help relieve swelling of the nasal passages, prevent runny nose and mucus from the nose. In addition, they are aimed at normalizing the activity of the respiratory system, through which full breathing is possible. Therapeutic measures can be carried out in conjunction with the use of some other medications, the use of which is vital. However, such changes while taking medications should be discussed with a specialist.

You can eliminate the source of the allergy and remove it from the body with the help of certain medications: Enterosgel, Smecta and activated carbon. All of them have a beneficial effect on the cause of allergies and in a short time will help get rid of the pronounced signs of the disease. It is also possible to restore the intestinal microflora through the use of certain probiotics:
- from baths;
- from speleotherapy;
- from inhalation.
- If the patient knows the irritants that cause allergies, then it is necessary to exclude them from his life as much as possible. For example, if a child suffers from seasonal allergies, then it is necessary to go to another region during flowering. It is known that life is much more difficult for allergy sufferers in southern latitudes, while symptoms are more easily tolerated in the north and northwest. This is explained by the too long period of flowering and fluff in the southern latitudes (from early spring to late autumn) and high humidity with a short flowering period in the north.
- In the case of bronchial asthma, the patient needs to train the respiratory system. Sports such as swimming, running, football, bicycle rallies, etc. are perfect for this. It is also useful for asthmatics to play wind instruments, or simply inflate balloons several times a week.
- Maintain order in the house. It is important to prevent the appearance of mold and mildew in your home, and also to throw away all “nuclear” household chemicals and switch to hypoallergenic products. It is important to remember that mold can be hidden in water filters, air conditioners, and bathroom walls. It is necessary to regularly clean surfaces from mold.
Complex therapy
What else can you do to help a patient overcome discomfort? Respiratory allergies will become a thing of the past if comprehensive treatment is used. For example:
- Physiotherapy, which includes procedures such as speleotherapy (long stay in a salt room) and inhalations (using sea salt, chamomile or chamomile).
- Immunotherapy (or strengthening the immune system). This method involves hardening procedures, gymnastic exercises, and the use of vitamin and mineral preparations.
- Treatment of concomitant diseases that may become aggravated in the event of respiratory allergies. Such therapy involves treatment of the gastrointestinal tract, parasitic infections, etc.
- Maintaining cleanliness of the home and household items.
- A diet designed to exclude foods that cause allergies from the diet (red vegetables or fruits, seafood, sausages, carbonated drinks, milk, citrus fruits, honey, and so on).
How does a doctor make a diagnosis?
Diagnostics and diagnosis Only an experienced allergist can accurately diagnose the disease, determine the causes of allergies and select appropriate therapy. In this case, skin tests are used to determine sensitivity to the most common allergens, or a blood test is taken to identify specific immunoglobulins E (IgE-immunoglobulins). The human body produces these globulins under the influence of corresponding allergens. Often both options are used.
If there is a suspicion of bronchial asthma, for patients over 5 years of age, a diagnosis of external respiratory function is prescribed before and after the administration of a bronchodilator drug using a spirograph and a special computer program.
Prevention
Prevention of this disease is of particular importance. After childbirth, parents should take all measures to protect the baby from the most likely allergens, especially during the most acute period - summer. To prevent the likely development of respiratory diseases in the unborn child, pregnant women with hereditary allergies must adhere to a strict hypoallergenic diet from the early stages of pregnancy. Without fail, the expectant mother must exclude from her diet foods containing preserves and chemical additives.
Natural, organic food during pregnancy will reduce the likelihood of the fetus developing immune abnormalities, which will later result in allergies.
It is very important to monitor the cleanliness of the premises in which the mother is in labor. Medical practice shows that constant breastfeeding maximally protects the baby from the occurrence of any allergic manifestations in the future. This can be explained by the fact that with natural feeding, the baby’s immune system is correctly formed, which helps him fight the manifestations of allergies.
Parents are required to closely monitor the child's behavior, especially if mom or dad has an allergic disease. First of all, they should be alerted to a long, dry, persistent cough, sudden difficulty breathing, swelling of the throat or nasal passages in the baby outside of a cold.
In this case, the child may become lethargic and lethargic, but allergosis may not affect his behavior in any way. At the slightest suspicion, you should consult an allergist. After all, the sooner the correct diagnosis is made and treatment is started, the more successfully it will be possible to cope with the disease.
Children whose allergies primarily affect the lungs or bronchi should train them. For this, it is recommended to engage in sports that contribute to the development of the so-called. "correct" breathing. These are, first of all, swimming, martial arts, hockey, and figure skating.
In addition to improving well-being, breathing training will strengthen the baby’s immunity, which will make it possible to stop attacks in the future. Such patients should spend as much time as possible in the fresh air, unless, of course, the cause of the disease is pollen in the summer.
Special gymnastics also helps to train proper exhalation. There is evidence that wind musical instruments, thanks to training the lower respiratory tract, can significantly reduce the number of allergic attacks and ease their course. There are practically no contraindications. The great thing about the breathing approach is that it can be practiced from a very early age.
And, of course, you shouldn’t despair! No matter how insidious this disease is, correct diagnosis and timely initiation of therapy can not only stop the development of the disease, but also ensure the good health of the little patient for a long time.
The process of allergy development is very complex, in simple terms it can be described as follows: a certain substance that is contained in food, or comes into contact with the skin, or is simply present in the air, for some unknown reason, is perceived by the body as a danger that can destroy its internal environment.
Immunity, in turn, is designed to protect the body from all kinds of threats; it perceives a dangerous substance as an antigen and produces antibodies. As you know, antibodies remain in the blood. When the body is exposed to a dangerous substance again, the antigen and antibodies cause an allergic reaction. Thus, the body reacts to.
ethnoscience
Respiratory allergies can also be cured with the help of folk remedies, but this should be done only after consultation with your doctor.
What recipes can help in the fight against an unpleasant disease? Below are some of them.
- Infusion of the tripartite series. Pour five grams of the herb into a glass of boiling water, let it brew for twenty-four hours, then take a glass orally in the morning and evening for a year.
- Herbal decoction. Take horsetail, St. John's wort, centaury, dandelion root and rose hips in equal parts. Pour water (at the rate of two tablespoons of the mixture per one glass of liquid), boil, leave and drink three times a day for three months. Helps a lot with dust allergies.
- Dandelion decoction will soften the manifestations of allergic reactions to the flowering of ragweed and poplar fluff. Squeeze the juice from dandelion leaves, mix it with water (1:1) and boil. Drink three tablespoons twice a day half an hour before meals.
- Chamomile infusion will relieve a runny nose. Pour boiling water (0.5 l) over forty grams of chamomile, leave for four hours and drink a glass morning and evening.
Main reasons
Respiratory allergies can appear for a variety of reasons. The most common of them is heredity, the transmission of the disease to a child from parents. This is why health problems most often appear in early childhood. An important role can be played by:
- use of artificial formula for feeding;
- the presence of perinatal pathologies in the nervous and respiratory systems;
- presence of atopic diathesis;
- the ecological situation in the area in which the baby grows and develops.
Eating foods containing preservatives, frequent colds, various skin lesions, and irritations of the gastrointestinal tract have a negative effect on the little person’s body.
Difficulties with diagnosis may often arise. Parents often mistake their child's respiratory allergy for a common cold caused by a bacterial or viral infection. A doctor can accurately determine the cause of damage to a child’s respiratory tract, who must first exclude the presence of an infectious process in the patient’s body.
general information
Respiratory allergosis is not a specific disease, but a complex of ailments based on allergic damage to the respiratory tract. Such disorders are more common in children of primary preschool age 6 from 2 to 4 years.
The peculiarity of respiratory allergies is that allergies occur against the background of active activity of infectious and non-infectious pathogens in the respiratory tract. Edema can affect the nasopharynx, larynx, trachea and bronchi.
During the course of a respiratory allergy, the mucous membrane of the respiratory organs is able to interact with all types of irritants. Hence the wide list of possible irritating components that can cause an outbreak of allergy. For example, food components enter the body through the pharynx and can therefore irritate the respiratory tract. People also inhale air that may contain various dangerous impurities and particles.
A specific irritating particle has its own specific properties. Most often, it is not the entire respiratory system that reacts to them at once, but only a certain part of it: the nose, larynx, bronchi, trachea, and sinuses. The affected area is usually the most sensitive of the entire respiratory tract. The allergic process starts on it, and the first symptoms appear.