Formed blood cells provide different functions and have their own purpose. Formally, they are divided into several classes.
- Platelets or red blood platelets. They ensure normal blood clotting and prevent the development of critically dangerous conditions. They act as a kind of cement for blocking damaged blood vessels.
- Red blood cells. Red blood cells. Transport hemoglobin. Due to their functions they can transport oxygen and carbon dioxide. There and back again. Their main task is gas exchange and cellular respiration.
The remaining structures are granulocytes and agranulocytes. The latter are represented by lymphocytes and monocytes. They provide a late immune response. That is, they enter into battle with bacteria, viruses and fungi somewhat later than the main cells.
It is granulocytes that provide the primary functioning of the body's defenses.
They are represented by three groups of structures:
- Neutrophils. They make up up to 70% of the total mass of the named cytological units. They are the first to enter the battle.
- Basophils. The cells are larger. Act as scavengers of the body. They ensure the destruction of anomalous agents, their destruction and processing of remaining substances.
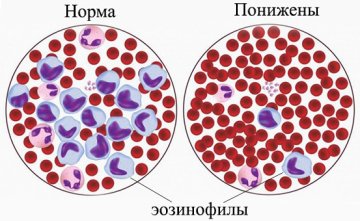
- Eosinophils. These are small cells with small nuclei; they are capable of phagocytosis, that is, relatively speaking, collecting garbage from the body. But they can only absorb relatively small particles of matter.
Eosinophilia is a condition in which the concentration of eosinophil cells increases. It is the third type of granulocytes that will be discussed. What should you know about a disorder in which the number of cytological structures increases?
Eosinophils in the blood during allergies
Eosinophils in the blood during allergies are an indicator in a general analysis that allows you to quickly identify the onset of the disease and begin to treat it.
The normal number of eosinophils depends on the age and gender of the child or adult. A blood test can tell a lot about a person's health. Everyone knows that there are red and white blood cells in the blood, that is, red and white blood cells that play their role. But not everyone knows that not all white blood cells are the same. They are different, but together they form a leukocyte formula, in which each type of leukocyte is responsible for its own area. One of these leukocytes are eosinophils. The number of eosinophils in the blood increases during allergies, so they play an important role in the diagnosis of such diseases.
What are eosinophils
These blood cells are produced by the bone marrow, mature within 3-4 days, circulate in the blood for several hours, then move to the tissues of the lungs, skin and gastrointestinal tract. The main task of these cells, like other leukocytes, is to destroy foreign proteins that enter the body. They provide the production of protective antibodies, and also bind and absorb parasitic cells.
There are norms for the content of this type of leukocytes in the blood; a change in their number may indicate certain disorders in the human body. It is generally accepted that eosinophils are responsible for allergies, and if they are present, their number increases. Also, their increased level may indicate infection with parasites, and a decreased level may indicate problems with immunity and hematopoiesis, as well as severe inflammatory processes and heart disease. The role of eosinophils in the development of allergies is obvious - the more allergen enters the body, the more leukocytes are produced to suppress it. That is, this is a symptomatic protective reaction of the body, and not part of the pathology itself. And if eosinophils are elevated in allergic rhinitis, it is the runny nose and allergies that need to be treated, and not the blood count and test results.

Blood levels
The norm of eosinophils depends on the age of the person.
| Age | Content of eosinophils in the blood, % of the total number of leukocytes |
| Children up to 2 weeks from birth | 1-6 |
| Children from 2 weeks to 1 year | 1-5 |
| Children from 1 year to 2 years | 1-7 |
| Children from 2 years to 5 years | 1-6 |
| Children aged 5 years and older | 1-5 |
| Adults | 1-5 |
The content of these white blood cells varies depending on the time of day. This is due to the work of the adrenal glands. Therefore, it is customary to take a general blood test in the morning on an empty stomach to obtain a more reliable picture. The table shows that due to physiological characteristics in children, the rate is higher. As a rule, eosinophils are increased by 10% or more in allergies. To see what level of eosinophils is acceptable for allergies, laboratories use special analyzers. However, the standards for this indicator may differ in different laboratories. Therefore, it is possible to decipher a blood test and carry out diagnostics based on it only based on the values that are used in a particular laboratory.
Signs of allergies
In what cases should you not worry, and in what cases should you promptly find out the cause of such a reaction and begin urgent treatment?
How many eosinophils do a child have with allergies?
- with a mild degree of pathology - no more than 10%;
- with an average degree - from 10 to 15%;
- in severe cases - from 15% or more.
Even 10% of the total number of leukocytes in the analysis already requires adjustment. True, it is necessary to evaluate the entire anamnesis as a whole. Indeed, in addition to allergies, these may be symptoms of the presence of parasites or inflammatory processes in the body. The doctor will make a diagnosis based on a combination of symptoms and test data. There are situations when eosinophils are normal in a child with allergies. Therefore, when diagnosing, you should not rely only on the indications of a general analysis; it is advisable to conduct additional research.
How many eosinophils are there in adults with allergies? As in children, allergic reactions can occur when the indicator in the leukocyte formula increases to 10%. But a doctor must make a diagnosis and prescribe treatment.
Causes, symptoms and treatment
There are quite a lot of disorders. We need to consider the main ones.
Helminthiasis
Mainly found in children. As was said, these are helminthic lesions. The mechanism in this case is twofold.
- On the one hand, eosinophils are produced to fight foreign agents. They synthesize reactive oxygen species and special proteins that destroy the uninvited guest.
- On the other hand, waste products of foreign agents cause hypersensitization of the body. The body literally rejects toxic substances and becomes overly sensitive. Allergies begin. The concentration of eosinophils increases several times.
By the number of cells we can talk about the degree and severity of the pathological process.
As for the main reasons, the culprits are opisthorchises and roundworms. Less commonly, tapeworms.
Localization can also provoke one or another degree of damage. Eosinophils reach their highest levels when the functioning of the brain, organs of vision, and liver is impaired. Although this is not always the case.
The symptoms of the pathological process also depend on the location of the worms. For example, with classic localization in the gastrointestinal tract, the manifestations will be as follows:
- Diarrhea.
- Constipation.
- Digestive disorders.
- Rapid weight loss.
- Acne.
- Changes in skin quality. Conditions of hair and nails. This is the result of poisoning of the body.
- Abdominal pain.
- Increased production of intestinal gas due to accelerated protein decay.
- Increase in body temperature. Not always, but this is also possible.
- Discomfort in the right side.
- Liver dysfunction with a pronounced increase in ALT and AST, bilirubin in a biochemical blood test.
These are just some of the manifestations.
Treatment is etiotropic. We need to get rid of helminths. This is where special drugs come to the rescue. Praziquantel, Biltricid and dozens of other names.
It all depends on the severity of the invasion, the type of organism and the individual characteristics of the clinical situation.
As for non-drug methods, following a proper diet is highly recommended. High in protein and carbohydrates.
The diet must be nutritious to cover the lack of substances.
Allergic reactions
Allergies are considered the most common cause of eosinophilia. This is quite logical if we take into account the mechanism of development of disorders. You can imagine it like this:
- When reacting to an allergen, the body releases a large number of basophils.
- When combined with antigens, granulocytes release histamine and a special mediator substance. It attracts eosinophils like a beacon and indirectly promotes the production of new granulocytes.
- The result is a persistent increase in the number of cytological structures in the bloodstream.
As a rule, the concentration increases insignificantly. There is a mild or, at most, moderate degree of eosinophilia. If a person is an experienced allergy sufferer, then there is likely a zero or reduced number of granulocytes of the type in question.
This happens because the cells die as a result of the immune reaction. But new ones simply do not have time to be synthesized.
Allergy symptoms are quite typical:
- Skin itching.
- Formation of a rash that you want to scratch.
- Painful sensations.
- Respiratory dysfunction.
- Tearing.
- Runny nose.
- Swelling is possible, it all depends on the type of severity of the pathological process.
Treatment is determined by the specific disease. To correct the allergy itself, antihistamines are used. First generation (Pipolfen, Tavegil, Suprastin, similar) or third (Cetrin).
Attention:
The second generation of antihistamines is prescribed much less frequently, since their negative effect on the heart has been proven. Especially with the systematic use of drugs.
When the lungs and bronchi are affected, dilators are used. Means for dilating the respiratory tract. Berotek, Berodual and similar.
It is imperative to fight the primary agent. The substance that provokes allergies. If possible, it is recommended to avoid meeting him.
A hazardous substance can be anything: from any product to dust, particles of animal saliva.
Respiratory system diseases
Some lung pathologies can also cause eosinophilia. This is a fairly rare condition, but it is possible.
Among the anomalous processes:
- Complicated pneumonia. In this case, the cell concentration increases significantly. And the stronger the inflammation, the more intense the secondary changes. Gradually, as recovery progresses, everything returns to normal.
- Fungal infection. The genus Aspergillus or, much less commonly, Candida. As a result, the body tries to fight off foreign agents by producing large numbers of specialized granulocyte cells. Based on the concentration, one can again judge the severity of the pathological process and the effectiveness of treatment of the disorder.
- Increased values of eosinophils in the blood are possible with bronchitis. The same goes for asthma.
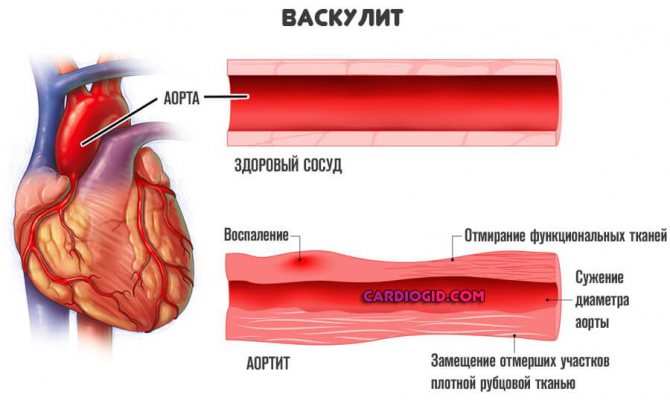
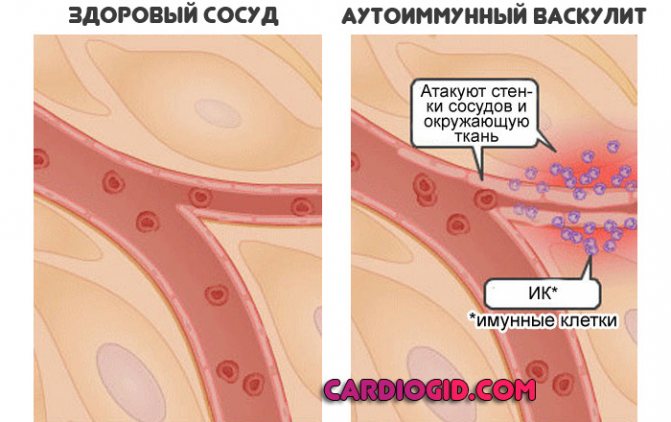
There are also rare diseases. For example, systemic vasculitis, inflammation of blood vessels localized in the lungs. These conditions are idiopathic. That is, it is impossible to accurately determine their cause. A thorough diagnosis is required.
Treatment depends on the specific disease.
- For pneumonia and infectious bronchitis, antibiotics are prescribed. First, a sputum flora analysis is performed. After this we can talk about effective therapy.
Anti-inflammatory drugs of non-steroidal origin are used. It is important to prescribe bronchodilators that will restore normal breathing.
If possible, take glucocorticoids, but carefully. They inhibit the functioning of the immune system, which is why prolonged pneumonia is possible. The dosage is selected separately.
- Fungal infections require the use of fungicides. Specialized means.
- For bronchial asthma, glucocorticoids and antihistamines are used.
- As for vasculitis, in addition to hormones, immunosuppressive drugs are needed. Which will slow down the intensity of the body’s defenses. Because most often it is the immune system that attacks the blood vessels.
- Viral and bacterial forms are treated with antibiotics and anti-inflammatory drugs.
Recovery is most effective in the early stages.
Blood pathologies
Basically, eosinophils are elevated due to myeloproliferative, malignant diseases. Leukemia and others. There are two main mechanisms of the process.
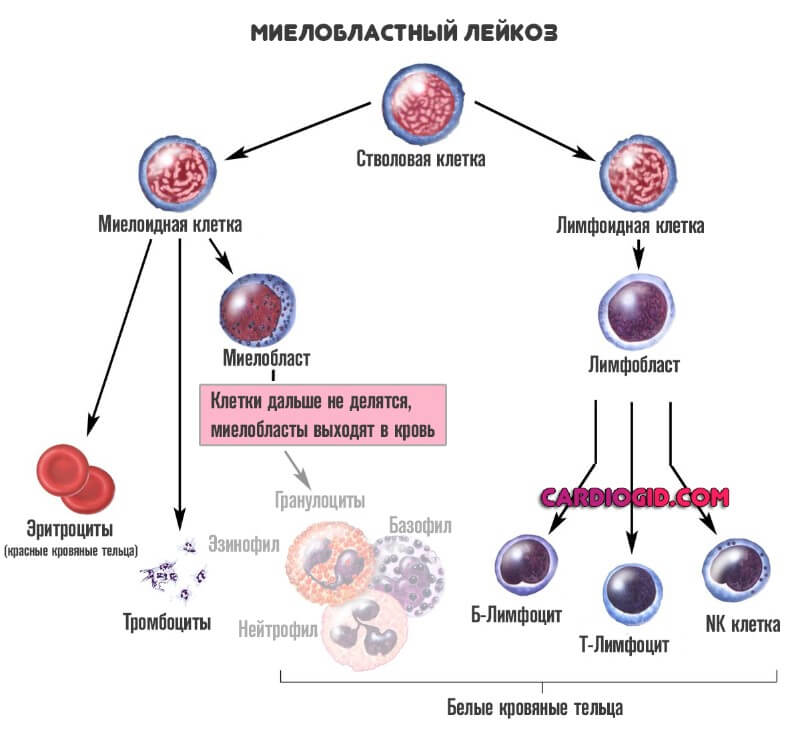
First. The synthesis of eosinophils and their maturation occurs in the bone marrow. With diseases of the described type, its tissues literally go crazy and begin to produce granulocytes at tremendous speed. This is a specific sign.
If a person is sick with lymphoma, the cells begin to produce cytokines that artificially stimulate the synthesis of eosinophils, thereby achieving their excessive number, the so-called hypereosinophilia.
Regardless of the type of pathological process, these are dangerous deviations. It is necessary to begin treatment as quickly as possible. Symptoms are determined by the specific condition.
The following subjective manifestations are mainly present:
- Skin itching.
- Blood clotting disorders.
- Increased body temperature.
- Significant sensitivity of the body to external factors.
- Tendency to allergic reactions.
Treatment depends on the diagnosis. Chemotherapy drugs are mainly used. Methotrexate and similar. Radiation treatment is possible. Gluocorticoids are also used in loading doses.
The dynamics of the pathological process are monitored, among other things, by the concentration of eosinophils. This is convenient because there is no need to perform a bone marrow puncture every time.
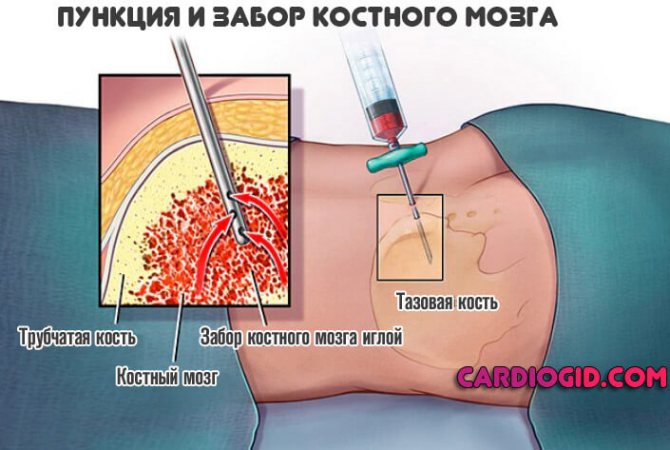
By the way, the procedure is quite risky and requires special preparation.
Digestive tract diseases
Pathologies of gastrointestinal structures can also provoke the growth of eosinophils. This is a relatively uncommon condition. The most common diseases that cause this scenario are:
- Gastritis. Stomach damage.
- Colitis. Inflammation of the intestinal mucosa.
- Others are extremely rare.
It is impossible to say exactly why, against the background of pathologies of the digestive tract, the content of eosinophils in the blood begins to exceed. The question is controversial. Research is being carried out.
Symptoms are determined by a specific pathological process. Granulocytes themselves, their increase, does not affect health in any way. This is a secondary manifestation.
As for the main signs, there are:
- Stomach ache.
- Indigestion.
- Stool disorders. Diarrhea, constipation or their alternation.
- Heartburn.
- Belching.
- Bloating. Increased production of intestinal gas.
- Vomiting and nausea.
- Rising temperature.
- Weakness, drowsiness.
- Loss of body weight. Dramatic weight loss.
Attention:
Differential diagnosis is necessary so as not to miss more dangerous pathologies - for example, cancer. Because it manifests itself in approximately the same way, but is treated only at an early stage.
Therapy is carried out by a gastroenterologist. It is necessary to fight the primary pathological process, then the cause of the increase in eosinophils will disappear on its own.
Drugs used:
- Antacids. Means for normalizing the acidity of gastric juice.
- Proton pump inhibitors. Omez and similar.
- Medicines to restore intestinal flora. Bifidum and others.
- For infection, antibiotics and anti-inflammatory drugs will be prescribed.
- Autoimmune lesions, such as Crohn's disease, are corrected with immunosuppressants and glucocorticoids.
The question is complex. A full examination is needed.
Endocrine system disorders
The reason for the violation is obvious. The fact is that the hormones of the adrenal cortex trigger the process of planned cell death in the body. Including granulocytes. If there are not enough glucocorticoids, a pathological condition begins.
Among the main diagnoses that provoke an increase in the concentration of eosinophils:
- Addison's disease. It's called adrenal insufficiency.
- Weakening the function of the pituitary gland. When hormones become too low.
The symptoms are quite typical:
- Weakness.
- Drowsiness.
- Decreased body temperature.
- Headaches and dysfunction of the central nervous system.
These are just some of the manifestations. Treatment is carried out by endocrinologists. It is necessary to introduce artificial glucocorticoids, then the concentration of eosinophils quickly returns to normal.
Cancerous tumors
Many malignant neoplasias are able to produce a special substance. A factor that causes the production of eosinophils.
These include:
- Lung neoplasms.
- Tumors of the digestive tract.
- Neoplastic lesions of the urinary structures.
Symptoms depend on the specific tumor and the exact location of the pathological process.
Specific oncology treatment:
- Removal of formation. As radical as possible.
- Chemotherapy. Drugs that slow down the synthesis of altered cells.
- Radiation treatment.
Gradually, the concentration of eosinophils decreases, but this is a rather long process. It takes months to return to normal.
Immunological problems
They are extremely rare. We are mainly talking about pathologies of the primary type. Not about AIDS, but about congenital disorders.
Anomalies are accompanied by characteristic symptoms:
- The patient is often and seriously ill.
- All infections take an abnormally long time and occur in complex forms.
Caution:
Immunodeficiency has a high mortality rate. There is no treatment as such.
With immunodeficiency, eosinophils in the blood are increased several times, and constantly, the condition persists for years.
Eosinophils in the blood: what is the norm and what are the causes of deviations
Eosinophils are a type of white blood cell that is constantly produced in the bone marrow. They mature over 3-4 days, after which they circulate in the blood for several hours and move to the tissues of the lungs, skin and gastrointestinal tract.
A change in the number of these cells is called a shift in the leukocyte formula, and may indicate a number of disorders in the body. Let's look at what eosinophils are in blood tests, why they can be higher or lower than normal, what diseases this shows and what it means for the body if they are elevated or lower.
Correction
Self-correction of eosinophilia is impossible. To normalize the level of eosinophils, it is necessary to combat the cause. If eosinophilia is mild, is associated with taking drugs or vaccination, or occurs during the period of convalescence, there is no need to worry. It is necessary to observe the blood dynamics after 7-10 days. If persistent or high eosinophilia is detected in a blood test, you should contact a specialist so that, based on examination, complaints, and medical history, he can conduct a diagnostic search for the etiological factor and prescribe appropriate treatment. To treat most diseases accompanied by eosinophilia, drugs from the group of antihistamines or glucocorticosteroids are used.
What does it mean if the indicator is elevated?
A shift in the leukocyte formula with a high level of eosinophils (eosinophilia) indicates that an inflammatory process is occurring in the body .
A severe degree is considered a fairly dangerous condition for humans , since in this case there is often damage to internal organs due to oxygen starvation of tissues.
When diagnosing cardiovascular diseases
In itself, an increase in eosinophils in the blood cannot indicate damage to the heart or vascular system , but pathologies, the symptom of which is an increase in the number of this type of leukocytes, can cause cardiovascular diseases.
The fact is that in the place of their accumulation, inflammatory changes are formed over time, destroying cells and tissues . For example, long-term, severe allergic reactions and bronchial asthma can cause eosinophilic myocarditis, a rare myocardial disease that develops due to exposure to eosinophil proteins.
Main reasons for the increase
Excess eosinophil counts can have a number of different causes including:

- damage to the body by parasites: helminthic infestations, giardiasis, ascariasis, toxoplasmosis, chlamydia;
- acute allergic reactions and conditions (allergic rhinitis, urticaria, Quincke's edema, dermatitis of various etiologies);
- pulmonary diseases: bronchial asthma, sarcoidosis, pleurisy, fibrosing alveolitis;
- autoimmune pathologies, which include systemic lupus erythematosus, rheumatoid arthritis, periarteritis nodosa;
- acute infectious diseases or exacerbations of chronic ones (gonorrhea, tuberculosis, infectious mononucleosis);
- oncological diseases, including malignant blood tumors - for example, lymphogranulomatosis;
- taking certain medications - aspirin, diphenhydramine, papaverine, aminophylline, sulfonamides, anti-tuberculosis drugs, penicillin antibiotics, etc.
Eosinophils in adults
For adults whose condition does not cause concern, the level of eosinophils does not exceed 0.3 per 109/l.
Increases are divided into three groups:
- insignificant – the indicator increases by no more than 10%;
- moderate – the increase is about 20%;
- high – more than 20%.
If in adults, in regular tests, the doctor notes that eosinophils are higher than normal, this means that an acute allergic reaction, a helminthiasis process is occurring in the body, or leukemia is developing.
Just as in children, an increase in the level of the indicator can be caused by diseases of the skin and blood. Quite often, pathology can be observed in such an autoimmune disease as systemic lupus erythematosus.
Disturbances in the functioning of the gastrointestinal tract also cause an increase in eosinophils.
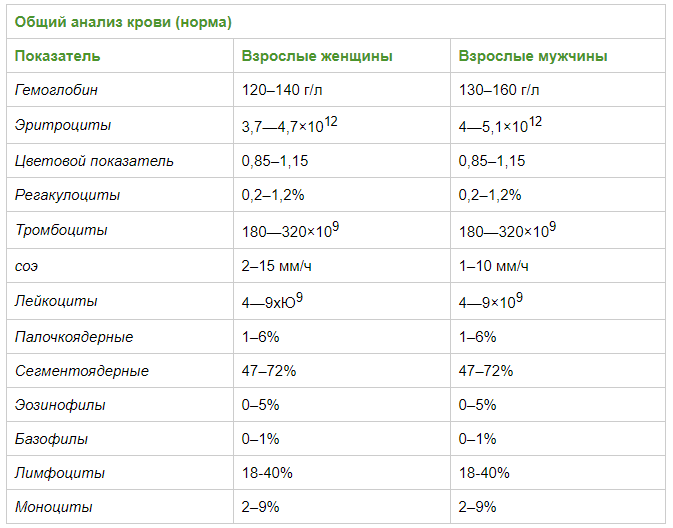
Table of norms
Reduced content in the results of the general analysis
A decrease in the level of eosinophils in the patient’s blood (eosinopenia) is no less dangerous than their increase. It also indicates the presence of an infection , pathological process or tissue damage in the body, as a result of which protective cells rush to the source of danger and their number in the blood drops sharply.
What does it mean for diseases of the heart and blood vessels?
The most common reason for a decrease in eosinophils in the blood in heart disease is the onset of acute myocardial infarction . On the first day, the number of eosinophils may decrease until they completely disappear, after which, as the heart muscle regenerates, the concentration begins to increase.
What causes the decrease
Low eosinophil counts are observed in the following cases:
- severe purulent infections and sepsis - in this case, the leukocyte form shifts towards the young forms of leukocytes;
- in the first stages of inflammatory processes and in pathologies requiring surgical intervention: pancreatitis, appendicitis, exacerbation of cholelithiasis;
- severe infectious and painful shocks, as a result of which blood cells stick together into mud-like formations that settle inside the vessels;
- dysfunction of the thyroid gland and adrenal glands;
- poisoning with lead, mercury, arsenic, copper and other heavy metals;
- chronic emotional stress;
- advanced stage of leukemia, when the concentration of eosinophils can drop to zero.
Eosinophils below normal
If the absolute number of eosinophils per milliliter of blood falls below 200, the condition is interpreted as eosinopenia.
In severe purulent infections, including sepsis, when the population of leukocytes shifts towards young forms (band and segmented), and then the leukocyte response is depleted. At the beginning of inflammatory processes, with surgical pathologies (appendicitis, pancreatitis, exacerbation of cholelithiasis).
On the first day of myocardial infarction. In case of infectious, painful shock, when the formed elements of the blood stick together into mud-like formations inside the vessels. For poisoning with heavy metals (lead, copper, mercury, arsenic, bismuth, cadmium, thallium). For chronic stress. Against the background of pathologies of the thyroid gland and adrenal glands. In the advanced stage of leukemia, eosinophils drop to zero.
Change in quantity in childhood
High eosinophils in the blood of a child are a fairly common occurrence. In premature babies, this condition is considered a variant of the norm, and disappears when normal body weight is reached.
In other cases, the most common causes of increased cell levels are:
- In newborns and bottle-fed infants, eosinophils can normally be elevated due to a negative reaction to cow's milk, as well as a number of medications. Also, eosinophilia in infants can be a sign of Rh conflict, hemolytic disease, staphylococcal sepsis or enterocolitis, pemphigus and hereditary diseases - for example, familial histiocytosis.

- At an older age, the number of protective cells in the blood of children often increases with atopic dermatitis and food allergies (often coinciding with the introduction of the first complementary foods), as well as helminthic infestations (the presence of pinworms and roundworms in the body).
- Common causes of this phenomenon in children include parasitic diseases (toxocariasis, hookworm), scarlet fever, chickenpox and eosinophilic gastroenteritis - a disease characteristic of patients under 20 years of age.
Eosinophils in children are reduced when there are viral or bacterial infections in the body and a general decrease in immunity . In addition, it can be caused by prolonged physical activity, severe psycho-emotional fatigue, as well as previous injuries, burns or surgical interventions.
In any case, a decrease or increase in the level of eosinophils in the blood is not an independent disease, but a symptom of a pathological process occurring in the body. To identify the problem and prescribe adequate treatment, the patient needs to undergo a set of additional studies and receive specialist advice.
Elevated eosinophils in the blood of women and children: causes of deviations and normal
Leukocytes in human blood are divided into several subtypes, one of which is eosinophils. Their characteristic features are a bilobed nucleus, as well as the ability to stain red under the influence of the substance eosin, from which this group of leukocytes gets its name.
Eosinophil levels are measured either as an absolute value per milliliter of blood or as a percentage of the total number of leukocytes. The second method is more common and is the one widely used in laboratories.
Increased normal eosinophil levels
In hematology, a condition in which eosinophils are elevated in an adult or a child is referred to as eosinophilia. This condition in itself is not a disease, but acts as a kind of marker of pathological changes in the body. There are three forms of eosinophilia:
At the same time, a number of hematologists expand the border of moderate eosinophilia to 20 percent, and expressed, accordingly, according to this gradation, starts from 21 percent. There is also a confirmed correlation between the form of eosinophilia and the complexity of the pathological process, which led to the growth of eosinophils in the blood: a higher degree of eosinophilia in most cases characterizes the complex course of the pathological process.
The reasons for the increased level of this type of leukocytes can be a number of reasons:
- atopic diseases (bronchial asthma, allergic rhinitis, hay fever);
- parasitic diseases (malaria, ascariasis, giardiasis);
- non-atopic skin diseases (pemphigus, dermatitis, epidermolysis);
- gastrointestinal diseases (gastritis, ulcers, cirrhosis of the liver);
- rheumatic diseases;
- hematological diseases (leukemia, anemia, polycythemia, lymphogranulomatosis, eosinophilic leukemia);
- lung diseases (pneumonia);
- weakened immune system;
- allergic reactions of all kinds. They are considered the most common cause of increased eosinophils in the blood;
- side effects from taking medications (most often eosinophilia is provoked by banal aspirin and a number of antibiotics in the form of injections).
Following the detection of a high level of eosinophils in the blood, the doctor prescribes additional diagnostics, which includes a biochemical blood test, ultrasound examination of the abdominal organs and stool sampling to determine the presence of worm eggs. In addition, if eosinophils exceed normal limits, it entails an immediate consultation with an allergist, who must confirm or rule out the presence of allergies - a prerequisite for the development of eosinophilia.
Diagnostics
Eosinophilia is detected by calculating the leukocyte formula of a clinical blood test. Since the range of pathologies accompanied by eosinophilia is quite wide, if changes in the tests are detected for the first time, you should consult a general practitioner. To confirm the disease that caused eosinophilia, taking into account clinical and anamnestic data, an examination is prescribed, which may include:
- Blood tests. The level of red blood cells, white blood cells, and platelets is determined. The presence of specific antibodies to helminths, fungi, anticytoplasmic antibodies (ANCA), and the concentration of certain hormones (cortisol, parathyroid hormone, estrogens, androgens) are checked. A genetic study is carried out for primary immunodeficiencies, as well as immunophenotyping, immunohistochemical analysis of blood cells to detect specific tumor antigens (CD markers).
- Allergy diagnostics. To identify the allergen, various allergy tests are performed - skin (scarification, patch, prick tests), provocative (nasal, inhalation, conjunctival), direct and indirect basophil tests. The ELISA method measures the level of immunoglobulin E (IgE).
- Sputum examination. A microscopic examination of sputum is carried out to study the cellular composition (the number of eosinophils, the presence of Charcot-Leyden crystals, Kurshman spirals), and to identify helminth larvae. Bacteriological and mycological culture of sputum is carried out to determine sensitivity to antibacterial and antifungal drugs.
- X-ray studies. One of the most informative methods for diagnosing pulmonary eosinophilia is chest radiography. The images reveal volatile (migrating) eosinophilic infiltrates in the form of darkened areas. With allergic bronchopulmonary aspergillosis, bronchiectasis and fibrosis of the upper lungs may be visible.
- Endoscopy. If eosinophilic lesions of the gastrointestinal tract are suspected, fibrogastroduodenoscopy and fibrocolonoscopy are performed with taking biopsy material. The morphological picture, in addition to eosinophilic infiltration, is characterized by fibrosis of the lamina propria of the mucous membrane.
- Spirometry. If the respiratory system is affected, the external respiratory function is assessed. The degree of patency of small and medium-caliber bronchi and the extensibility of lung tissue are measured. For patients with bronchial asthma, a decrease in the volume of exhaled air (Tiffno index) and an improvement in respiratory function after a pharmacological test with salbutamol are typical. With pulmonary eosinophilia, a decrease in the vital capacity of the lungs is observed.
- Histology. To confirm Churg-Strauss syndrome, a lung biopsy is taken. Perivascular eosinophilic infiltrates are noted. To study the morphological picture of the bone marrow (in case of suspected leukemia), sternal puncture and trepanobiopsy are used. Hyperplasia of the granulocytic lineage of hematopoiesis and hypercellularity due to eosinophilic myeloblasts are detected.
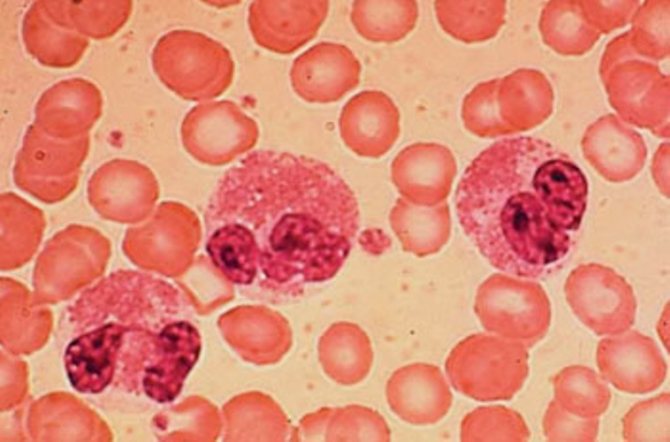
Eosinophilia in peripheral blood smear
Increased eosinophil levels in children
The reasons for the development of eosinophilia in children are somewhat different from adults and have a fairly clear age classification. In children under six months of age, eosinophils outside the normative values are in most cases provoked by the following reasons:
- Rhesus conflict;
- staphylococcal sepsis;
- atopic dermatitis;
- eosinophilic colitis;
- hemolytic or serum sickness.
Between the ages of six months and three years, eosinophilia in children develops due to the following prerequisites:
- atopic dermatitis;
- allergies to medications;
- Quincke's edema, which in most cases is also of an allergic nature.
At the age of three years and older, an increased rate of eosinophils in the blood of a child is mostly a manifestation of infectious diseases and allergic manifestations:
- scarlet fever;
- chicken pox;
- allergic rhinitis;
- allergies with manifestations on the skin.
Eosinophils in the blood exceeding the norm in combination with an increase in other indicators in the blood test are quite indicative. In particular, high eosinophils and monocytes are characteristic in the presence of an infectious process (this combination is indicative of mononucleosis), as well as in viral and fungal diseases. If eosinophilia is recorded against the background of high leukocytes, then this may indicate the presence of worms, the development of a viral infection against the background of allergies, and the onset of scarlet fever.
How to lose excess eosinophils?
After identifying the cause of excess of the norm, the identified disease can be cured. But: first you need to undergo an examination of the whole body. The child’s body is very weak; if a foreign particle gets into it, illnesses may arise, which may have consequences in the future.
If eosinophils are elevated, pathologies arise: rhesus - conflict skin diseases, vascular diseases, malignant tumors.
It is necessary: start treatment on time, and examine the child frequently in preventive plans.
Worm infestation is the reason for the increase
Causes of low levels of eosinophils in the blood
A decrease in the level of eosinophils in the blood below the standard value is designated by the term eosinopenia. At the same time, there is a decrease in this indicator down to zero, which is a very dangerous condition. If eosinophils are practically absent in the blood, this may indicate the development of acute appendicitis, typhoid fever or diphtheria, as well as an advanced form of leukemia.
In the case of a non-critical drop in this indicator, eosinopenia may be a consequence of a person’s post-operative condition, a consequence of injuries and burns, sepsis, or evidence of the onset of the development of any infectious disease.
Clinical studies also show that persistently low levels of eosinophils are characteristic of people with Down syndrome and people with chronic fatigue syndrome.











