What is insect allergy
Insect allergy is an allergic reaction that occurs in a person during or after contact with insects.
This disease is often confused with an allergy to insect bites, but there are differences between them.
They lie in the fact that with insect allergies, a reaction can begin to develop after contact with insects, as a result of particles of the body of Hymenoptera or products formed during their vital activity entering the respiratory organs.
The similarity is that severe allergic insect reactions occur when insects sting or bite them.
Hypersensitivity to the venom of stinging insects (bees, bumblebees, wasps) can be found in 0.4-85 of the planet's population.
The risk group includes beekeepers and those people who live near apiaries; their percentage of insect allergies reaches 15-43%.
With the development of an anaphylactic reaction to the venom secreted by Hymenoptera, the fatal outcome reaches up to 80%.
In addition to stinging insects, insect allergies are caused by blood-sucking insects - bedbugs, fleas, mosquitoes.
There are allergic reactions to cockroaches and insects that are used as fish food.
Rice and granary weevils contain a special substance called cantharidin. If it gets on the human body or inside, it causes skin irritation, headaches, vomiting and often convulsions.

Products contaminated with black flour beetle (small) or grain grains cause acute stomach and intestinal disorders. Such products are potentially dangerous even after the insects have been removed.
Several species of beetles belonging to the darkling beetle family live in people's homes and in warehouses with flour and grain.
The beetles themselves and their larvae damage food supplies, leaving feces on them. The chitinous cover of these insects is filled with allergens that have common features with mite allergens.
Beetles belonging to the genus Diamphidia locusta, Paederus are also poisonous to humans.
Dangerous toxic substances are contained in the blood of ladybugs, soft beetles, blister beetles, red wings, and little ones.
Toxic substances are contained in the hemolymph of small beetles of the genus Paederus, family Staphylinidae.
These beetles live along the banks of natural bodies of water, which makes it possible for them to land on caught fish.
Even one bug that enters the human digestive system causes severe poisoning.

Insect allergies most often occur in people who have a history of other types of allergic reactions and a hereditary predisposition.
In addition to beekeepers, the risk group includes employees of silk production enterprises and entomological laboratories.
Insect allergy has its own code in the international classification of diseases.
The ICD 10 code for the disease is “W57 Bite or stinging by non-venomous insects and other non-venomous arthropods.”
Symptoms

Often, an allergy to insect bites occurs suddenly (15-20 minutes after contact). At the site of the bite or sting, a rash appears, redness of the skin, pain, itching, local swelling, which in most cases is accompanied by weakness, nausea, high body temperature, as well as inflammation of nearby lymph nodes.
If there have been many insect bites, the toxic effect of the poisons often leads to loss of consciousness. If a person has hypersensitivity to poisons, then an insect sting can provoke anaphylaxis and even lead to death.
The main signs of insect allergies:
- swelling at the site of the bite, itching of the skin, urticaria,
- disruption of the stomach and intestines: bloating, vomiting, diarrhea, stomach pain, deterioration in general condition,
- severe swelling of the throat, lips, tongue (if bitten in the mouth or neck), which can cause difficulty breathing or shortness of breath. In severe cases, bronchospasm and tachycardia (heartbeat disturbance) occur.
- severe dizziness, loss of consciousness,
- anaphylactic shock is the most dangerous complication of allergies, which is characterized by a decrease in blood pressure, fainting, and in 10% of cases death can occur (usually in older people).
The most dangerous are the bites and stings of a large number of insects; in this case, a lot of poison enters the human body at the same time, which can cause severe intoxication.
Routes of allergen entry into the body
There are several ways insect allergens enter the body:
- Along with poison at the moment of sting. This method of penetration of allergens is typical for exposure to Hymenoptera.
- Together with saliva that gets under the skin when bitten by insects from the order Diptera (diptera).
- By contact or inhalation method. Allergens are found on scales or dust from the body of insects. More often, this method of penetration occurs through contact with lepidoptera and caddisflies. Inhalation insect allergy sometimes occurs to Hymenoptera; this type of reaction includes the so-called bronchial asthma in beekeepers.

Causes

There are several groups of insects that can cause an allergic reaction.
- Bloodsucking. The blood-sucking insect does not have a sting, but the reaction can be caused by components of the saliva of mosquitoes, fleas, bedbugs, some types of flies, horseflies, midges, and lice. Their saliva enters the human body with an insect bite.
- Stinging. Insects inject poison into the human body with the help of a sting; it is the poison that is the allergen.
- Household pests. These pests include dust mites and cockroaches. It is these insects that can provoke asthma attacks or suffocation. They can provoke an allergic reaction in the body without even contacting a person. Also, waste from pests can enter the body with oxygen, along with food or in the form of aeroplankton.
Types of allergic reactions to hymenoptera stings
When stung by Hymenoptera, a toxic or allergic reaction may develop.
These two forms of reaction have similar and distinctive features, but sometimes it is difficult for a non-specialist to separate them from each other.
Clinical picture of a toxic reaction.
A toxic reaction in humans occurs when insect toxins enter the bloodstream along with saliva.
The symptoms are mostly local and are experienced by most people who experience insect bites. This is swelling, redness and pain at the site of insect impact.
But if a person immediately receives multiple bites (sometimes up to five hundred stinging insects can attack at once), then a severe clinical picture develops, covering the entire body as a whole.
In addition to local, pronounced symptoms, severe toxic damage is indicated by:
- Headache and dizziness;
- Chills;
- Hemorrhagic syndrome;
- Convulsions and paralysis. Paralysis of the respiratory center is dangerous;
- Anaphylactoid reactions.

The occurrence of such symptoms in children is especially dangerous; the younger the child, the higher the likelihood of death.
In case of severe toxic poisoning, medical assistance should be provided immediately.
Clinical picture of an allergic reaction.
Allergies that occur when stung by insects are IgE-mediated reactions, so all symptoms occur quite quickly.
Pronounced local changes may be observed - various types of rashes (in severe cases, necrotization of the affected tissues is noted), erythema, swelling, itching.

However, a local reaction with a true insect allergy does not always occur.
More often, a person is diagnosed with Quincke's edema, a generalized rash and itching, urticaria, laryngeal edema, which turns into bronchospasm.
The main cause of death from insect stings is anaphylactic shock, which develops within a few minutes.
In addition to local and systemic manifestations of allergies, symptoms of intoxication may appear.
An allergic reaction can also be late, affecting blood vessels, liver, kidneys, and the nervous system.
This reaction sometimes occurs as hemorrhagic vasculitis or serum sickness.
There are several differences by which a toxic reaction to a sting by Hymenoptera is separated from an allergic one:
- Allergies occur only in some people. And most often it affects people with a predisposition to pathology or having other types of allergic reactions.
- The severity of the allergic reaction increases with each new sting.
- The amount of poison that enters the body does not affect the general well-being of allergies.
- During an allergic reaction in a person, antibodies related to immunoglobulin E are detected in the blood. The antibody titer depends on the severity of the allergy.
- Specific hyposensitization for allergies gives positive results, that is, the human body reacts less to insect bites.
Insect stings.
The maximum number of individuals in Hymenoptera colonies is observed at the end of summer. That is why in August and September the largest number of patients with stings and allergic reactions to them is recorded.

Clinic
All reactions are divided into local and systemic. There is never a general allergic reaction to the first sting in life. The severity of the reaction increases with each subsequent sting.
For a local allergic reaction
swelling and redness at the sting site have a diameter of about 10 cm and last for at least 24 hours. Severe itching is observed. Developed swelling in the mouth and throat is a dangerous prognostic sign, as it can lead to asphyxia.
Systemic allergic reactions
are detected in 0.8-5% of patients.
There are mild, moderate and severe
systemic lesions (see
).
For mild cases
a generalized rash, itching, malaise, and anxiety are observed.
If two more symptoms are added to these symptoms (such as angioedema, dizziness or pain in the heart, abdomen, dyspeptic symptoms), the reaction is regarded as moderate
.
For severe generalized damage
In addition to the listed signs, dyspnea, dysphagia, hoarseness, laryngeal edema, bronchospasm, and a feeling of impending danger are noted. The speed of appearance and growth of symptoms serves as an indicator of the severity of the condition: reactions that develop 1-2 minutes after the sting are the most severe, delayed reactions are milder.
Anaphylactic shock
develops a few seconds or minutes after the sting: suffocation, nausea, vomiting, drop in blood pressure, collapse, cyanosis, loss of consciousness, urinary and fecal incontinence are observed. Death may be caused by collapse or airway obstruction.
According to the European Allergy Society, after a local allergic reaction with a repeated sting, a systemic reaction develops in less than 5% of cases, after a mild systemic reaction - in 15-30%, and after a severe one - in more than 50%.
Repeated stings by insects play an important role in the development of allergies to Hymenoptera venom. Thus, among beekeepers, allergies to bee venom occur in 15-43% of cases, which significantly exceeds the prevalence of this allergy in the population as a whole (0.8-5%).
Classification of Hymenoptera
Hymenoptera order (Hymenoptera), stinging suborder (Aculeata), bee family (Apidae) and social wasp family (Vespidae).
The family Apidae includes:
- Subfamily of true bees (Apinae). Genus of bees - Apis L.
- Bumblebee subfamily (Bombinae). The genus of true bumblebees is Bombus Latr.
The family Vespidae includes:
- Subfamily of paper wasps – Vespinae. The wasp genus is Vespula Thorns, the long wasps are Dolichovespula Rohw, the hornets are Vespa L.
- Subfamily Polystinae. Genus Polistes - Polistes Latr.
Etiology and pathogenesis
The stinging apparatus of insects from the order Hymenoptera developed in the process of evolution from the ovipositor.
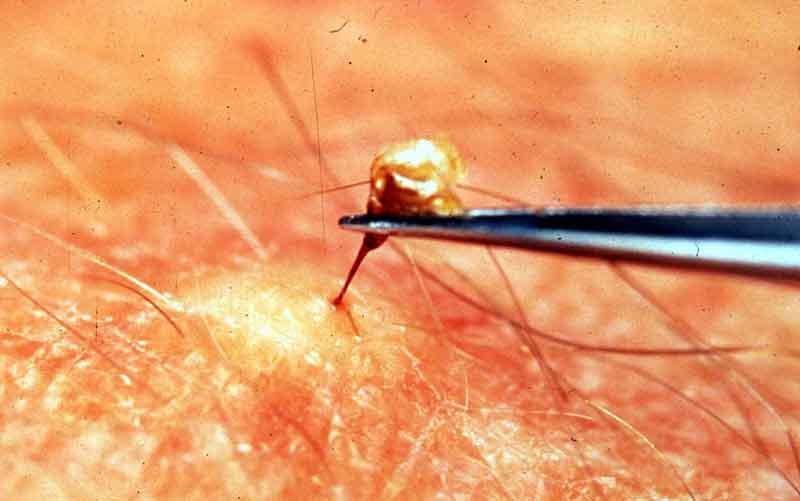
In a calm state, the sting is retracted into the abdomen. The bee's sting has distinctive features compared to other hymenoptera.
It has from 8 to 10 barbs; it is they that are fixed in the subcutaneous layers of mammals and the sting remains there.
POPULAR WITH READERS: Sesame allergy in infants, symptoms, treatment methods

Along with the sting itself, poisonous glands, a poisonous sac and the last node from the nerve chain of the abdomen also remain in the victim’s body.
The muscles of the poisonous sac contract even after the sting is separated from the body of its owner, so the poison is released into the victim’s body for some time.

The amount of poison released by the sting structures during a sting varies from 0.05 to 0.3 mg.
The venom of any Hymenoptera is a complex mixture of antigens. There can be from 2 to 21 antigenic fractions in the venom.
High allergenic activity was found in phospholipase A, otherwise this antigen is called the “major bee venom allergen.” Hyaluronidase is also a dangerous allergen.
In addition to the two allergenic components mentioned above, the venom contains acid phosphatase (allergen B), allergen C and mellitin.
All of the listed allergens enter the human body in varying quantities and, if there is a predisposition to allergies, cause its development.
The biological effect of Hymenoptera venom entering the victim’s body is a total effect that develops in response to 4 types of toxic effects of the poison.
These four types include the following body reactions:
- Hemorrhagic;
- Hemolytic;
- Neurotoxic;
- Histamine-like.
In almost all Hymenoptera, the toxic effects of poisons on the body have similar characteristics, although a number of differences have been identified.
Hornet venom causes a strong local reaction and pronounced hemolysis, but its neurotoxic effect is insignificant.
After being stung by insects from the aspen family, the risk of infection of the wound is increased; inflammation after the bite can develop either after a few hours or after three to five days.

Toxic reactions are more pronounced if a person is attacked by a large number of stinging insects. Cases of a violent reaction of the body with a fatal outcome have also been recorded after being stung by one or two insects.
A survey of beekeepers revealed that 2% of people in this profession, who previously had no reactions to stings, increase sensitivity to bee venom over the course of a year. In this case, urticaria, rhinorrhea, conjunctivitis, and bronchospasm develop.
The basis for the development of these symptoms is the immunological mechanism, which in turn appears when the body is sensitized.
The mechanism for the development of allergies due to stings is based on the reagin type of allergy, or otherwise type 1.
Sensitization occurs due to the presence in the human blood of hymenoptera venom-specific antibodies from the IgE class.
Summarizing all the data on the development of allergies due to stings, we can conclude that:
- Specific IgE antibodies to the poison are found in the serum of people who have an allergic reaction with general or pronounced symptoms. And these antibodies appear when bitten by one Hymenoptera.
- Specific IgE antibodies to the venom are not detected or their lowest concentration is detected in people without a predisposition to an allergy to Hymenoptera. This also applies to people who are allergic to other types of allergens.
- The level of specific IgE antibodies to the venom increases immediately after a sting and decreases against the background of specific hyposensitization.
- Specific IgE antibodies to the venom are found in the serum of beekeepers. Beekeepers whose bodies are resistant to stings may have high antibody titers.
- Specific IgE antibodies to the venom are present in patients who are allergic to stings. Their titer increases after hyposensitization. Antibodies in the blood of these patients play a protective role, that is, they are blocking.
Insect allergy. Part 1: Symptoms and Treatment
Insect allergy
(from the English insect - insect) is an allergic reaction of the body to contact with insects.
This reaction can be provoked by the following factors
:
- Penetration of hymenopteran insect venom during sting (bee, wasp, bumblebee, hornet, ant).
- Ingestion of saliva from a blood-sucking insect during a bite (mosquito, mosquito, gadfly, horsefly, bedbug, rodent, fleas, midges, etc.)
- Getting scales and other fragments of living or dead insects onto the skin or into the respiratory tract, mainly in the form of aeroplankton, that is, tiny particles floating in the air. The most popular “culprit” of allergies in this type is the cockroach; butterflies, moths, moths, mosquito larvae, locusts, and grasshoppers often also cause reactions.
The likelihood of insect allergies is influenced by heredity (if one of the child’s close relatives suffers from this disease), as well as the presence of other allergic diseases in the child, and a high level of IgE in the blood. With repeated bites, the reaction in most cases is even more severe than in previous cases.
To identify insect allergies in a child
, you can take the following tests:
- skin prick tests with insect extracts;
- radioallergosorbent test (RAST);
- multiple allergy sorbent test (MAST).
Clinical picture
The clinical picture of allergies that occur after insect stings is very diverse.
An allergic reaction is usually divided according to the time of its development from the moment of the bite into early and late.
Early allergic reactions to stings.
They make up from 95 to 98% of cases. Symptoms appear immediately after the sting or within an hour.
Several systems of the body are simultaneously involved in the pathological process.
According to the clinical picture, these reactions relate to anaphylactic shock, but with varying degrees of severity.
Early allergic reactions are classified into three degrees depending on the severity of symptoms.
- First degree reaction or mild general allergy. The pathological process involves the skin - the patient develops generalized itching and urticaria, and at the site of exposure there is swelling of the bite site itself, along with the skin and subcutaneous tissue.

Chills, a feeling of heat, hot flashes often appear, the temperature rises, an increase in excitement is possible, or, on the contrary, lethargy, drowsiness, and a depressive state. If the urticaria is gigantic in size, then a large amount of plasma is released from the blood, which threatens hypotension and dizziness. - Second degree reaction or general allergy of moderate severity. First of all, a spasm of the smooth muscles located in the internal organs occurs. This is manifested by bronchospasm, spasms of the digestive organs, and in women the uterus is involved in the process. Serous swelling of the mucous layer of the respiratory and digestive organs is also characteristic. Symptoms that arise during the first type of reaction are also recorded, but they are not expressed significantly. The patient is more concerned about headache, weakness, tachycardia, arrhythmia or bradycardia. A collaptoid state occurs, manifested by severe weakness, a drop in blood pressure, and darkening of the eyes.
- The third degree reaction is the most severe, this is anaphylactic shock. Symptoms of acute vascular insufficiency come to the fore - ischemic damage to the heart, central nervous system, bronchospasm, spasms of the uterus and gastrointestinal tract. Changes in the skin do not always occur, and if they do occur, they appear later than the acute stage. The occurrence of anaphylactic shock against the background of cardiovascular pathologies is characterized by an unfavorable course.
An allergy suffered after a sting often gives rise to an exacerbation of existing bronchial asthma or chronic urticaria.
Late reactions.
Occurs only in 2-5% of people with a predisposition who have suffered a sting. They develop in 6-12 hours.
They manifest as generalized vasculitis with damage to blood vessels, skin, liver, and kidneys. Possible damage to the nervous system - myelitis, neuritis, polyneuritis.
Based on the time of development and clinical symptoms, late reactions are classified as type III and partly type IV allergic reactions.
The symptoms of late allergies depend on the localization of pathological changes in the target organ.
Classification of reactions

Insect allergies have various clinical manifestations and are classified according to severity:
- Mild degree. Generalized vesicular, hemorrhagic or papular rash, malaise, widespread skin hyperemia, itching, generalized urticaria.
- Average degree. This degree includes all of the above symptoms and two or more of the following: chest tightness, dizziness, nausea, vomiting, diarrhea, angioedema, pain in the heart.
- Severe degree. Attacks of suffocation that are combined with any of the symptoms listed above, as well as two or more of the following symptoms: cough with viscous sputum, shortness of breath, dysphagia, drowsiness, weakness, confusion, fear of death.
- Anaphylactic shock. Any symptom of the above, as well as collapse, loss of consciousness, low blood pressure, urinary and fecal incontinence.
Diagnosis
If there is evidence that the victim had an allergy when stung, then it is not difficult to immediately make a diagnosis.
At the first appearance of an unusual reaction, it is necessary to collect an allergic history, establish all the symptoms and conduct a series of analyzes and tests.
When collecting anamnesis, you can pay attention to the fact that at the first stings the patient did not make any special complaints about a general deterioration in health. The severity of the reaction increased with each new episode of the bite.
Skin tests to determine the type of allergen are carried out no earlier than a month after the acute reaction has stopped.

It is strictly forbidden to perform a provocative bee sting, as this can be fatal to humans.
Differential diagnosis of insect allergies is carried out with:
- Toxic reaction. It is distinguished by the strong severity of symptoms when stung simultaneously by more than a hundred individuals. Certain changes are detected in the blood, indicating a hemolytic and hemorrhagic effect of the poison. With toxic damage there may be convulsions, hypersalivation, areflexia, and delirium.
- With cardiovascular failure, epilepsy, ectopic pregnancy in women, sun and heat stroke in children and adults. Sometimes a person loses consciousness before he has time to report that he has been stung by an insect, and in these cases differential diagnosis with these diseases is necessary, since they have some similar signs.
It is quite difficult to make the correct diagnosis for late allergic reactions. Especially if they occur with symptoms uncharacteristic of allergies.
Insect bites in a child
Insect allergies in children are quite common. The main treatment consists of the following activities:
- collecting an allergy history and visual examination of the child,
- if an allergic nature is detected, the specialist prescribes laboratory tests and scrubbing of the skin,
- during the initial examination, skin tests are required; this method allows you to differentiate insect allergies,
- To confirm insect allergies in children, blood tests are performed for the presence of IgE, followed by provocative testing.
Treatment of an allergic reaction to a hymenoptera sting
If an insect allergy occurs, assistance should be provided before medical personnel arrive. If the sting was caused by a bee, then it is necessary to remove its sting as quickly as possible.
POPULAR WITH READERS: Allergies in children - types, symptoms, treatment
The venom sac of the sting is emptied within 2-3 minutes after this organ remains in the human body.
Remove the sting using a sharp needle, but so as not to damage the entire stinging apparatus.
You can independently reduce the development of local allergy symptoms. Measures should be aimed at reducing vascular permeability, for this:
- A tourniquet is applied above the bite site. If the tourniquet is applied correctly, it blocks the spread of poison throughout the body.
- Coldness to the sting site. Applying a cold compress or frozen product leads to spasm of the superficial vessels, which also delays the absorption of the poison.
- Antihistamines are prescribed. It is necessary to use not only systemic agents, but also ointments with glucocorticoids - Locacorten, Flucinar.

- The blisters at the site of the sting are opened under aseptic conditions and treated using a solution of potassium permanganate.
- For severe pain, analgesics are selected.
- If the pathological process involves the lymph nodes and the body temperature rises, then a corticosteroid regimen is prescribed for several days.
- The patient is prescribed plenty of fluids and bed rest is recommended.
If anaphylactic shock develops after emergency treatment using medications, further treatment is carried out in a hospital.
The patient is usually observed for about a week after the acute process has stopped, during which time complications may appear or an additional late allergic reaction may develop.
Late allergic reactions are mainly treated with corticosteroids.
If an allergy to bee stings is established, patients are advised to follow preventive measures:
- During the summer season, aerosol insecticides should be kept in the house. When an insect appears, the product must be sprayed immediately.
- Go outside in clothes that cover the entire body as much as possible. It is better to choose light shades of fabrics, since dark and bright colors attract hymenoptera more.
- If an insect appears nearby, there is no need to wave your arms or make sudden movements.
- You should not walk barefoot on the grass, especially where clover grows. The smell of this plant attracts bumblebees and bees.
- Do not use propolis in everyday life or for the treatment of any diseases; it contains an antigen that causes allergies.
First aid
A person suffering from any type of allergic reaction needs emergency treatment.
To do this, you need to do the following:
- if a wasp has bitten you, remove the sting immediately, this must be done carefully using tweezers, without squeezing it out, so that no more poison gets into the body,
- an allergy sufferer must be given an injection of adrenaline; if it is not available, it is recommended to take an antihistamine,
- In any case, if you suspect an insect allergy, you should seek advice from a specialist.
After undergoing examinations, the patient is prescribed immunotherapy aimed at eliminating the underlying cause of the disease. This course of treatment is carried out under the supervision of a doctor.
Allergy to blood-sucking insect bites
Blood-sucking insects are divided into several orders.
Classification.
Order – Diptera (diptera).
Suborder long-whiskered dipterans (Nematocera):
- Family true mosquitoes (Culicidae). Genus – Anopheles, Aedes, Culex.
- Family of mosquitoes, bells (Chironomidae); biting midges (Ceratopogonidae); midges (Simuliidae); butterflies (Psychodidae). Genus mosquito (Phlebotomus).
Suborder straight-stitched short-whiskered (Brachycera-orthorrhapha):
- Horsefly family (Tabanidae).
Order: Hemiptera (hemiptera or bugs). Order: Siphonaptera (fleas). Order: Anoplura (lice).
Conventionally, the concept of “gnus”, widespread among the population, includes 5 families of insects that suck blood - biting midges, true mosquitoes, midges, horseflies, mosquitoes.
Only females lead a predatory lifestyle, that is, they drink blood. Males are needed to produce offspring.

Insects from the order Diptera can be carriers of infections.
Mosquitoes carry the pathogens of yellow fever, malaria, Japanese encephalitis, and encephalomyelitis.
Midges carry the pathogens of Japanese encephalitis and equine encephalomyelitis.
Midges can become a source of infection with anthrax, glanders, plague, and tularemia.
Mosquitoes transmit cutaneous and visceral leishmaniasis, pappataci fever. Get anthrax and polio.
Blood-sucking insects are distributed throughout the globe. They live not only in natural areas, but also in big cities.
Etiology and pathogenesis
The saliva of blood-sucking parasites contains toxic, anticoagulant and anesthetic substances.
After a bite, itching and pain occurs in the damaged area within a few minutes.
If you take a skin biopsy within 12 minutes to two days after an insect bites a person, you can determine the inflammatory reaction through histological examination.
It occurs in three phases. Initially, leukocyte infiltration occurs, it is replaced by an accumulation of histiocytes, then the number of lymphocytes increases.
The saliva of some species of midges is particularly poisonous.
People have different sensitivities to blood-sucking bites. The local population is usually the least susceptible, while visitors may experience severe insect allergies after being bitten.
High severity of symptoms is also typical for children. Towards the end of the season, as a rule, resistance increases.
Atypical manifestations of bite symptoms are recorded. This can be a giant infiltration of the bitten area of the body, which lasts up to 4 weeks.

Systemic manifestations and asthma attacks are noted.
It has been established that allergenic activity is already present in the tissues of the formed insect pupa. In an adult mosquito, allergenic activity is highest in the salivary glands, less in the tissues of the chest and head.
When bitten by an insect from the order of fleas, bedbugs, or lice, allergic reactions usually develop at the local level and occur in the urticarial and erythematous type.
Diagnostics

When diagnosing insect allergies, specialists conduct a comprehensive examination: visual and systemic (general condition).
During a visual examination, doctors find out:
- location of the bite, changes on the skin, type of insect,
- degree of manifestation of the reaction (year-round, seasonal),
- the patient being in contact with insects (the presence of allergic particles in the living room, at the workplace, on vacation),
- the presence of a hereditary factor or other forms of allergies in the patient.
For a more accurate diagnosis, specialists prescribe additional laboratory tests:
- radioimmune testing to determine the amount of IgGc,
- radioallergosorbent testing, which determines specific IgEc,
- enzyme immunoassay testing.
Allergy tests are also carried out for the presence of insect venom. These studies are carried out exclusively in allergological laboratories.
There are contraindications to such tests. These include:
- tuberculosis,
- rheumatism,
- pregnancy, lactation,
- infectious diseases,
- autoimmune diseases,
- mental disorders or their exacerbations,
- age up to three years.
Differential diagnosis of the patient is carried out based on his condition:
- examine neurovegetative symptoms: nausea, anxiety, dizziness, rapid heartbeat,
- Typical allergic manifestations are examined: skin redness, lacrimation, swelling, rhinitis.
Clinical picture
In the clinical picture of insect allergy to the bites of blood-sucking insects, in contrast to the reaction to stings, local symptoms predominate.
The nature of local manifestations is close to the delayed or immunocomplex type.
There is a certain pattern in the development of skin changes depending on the type of biting insect.
If a person is bitten by a mosquito, then when an allergy develops, the rash is papular, less often vesicular.
Its recurrent course is noted, that is, periods of exacerbation and disappearance of rashes, which can last up to 2 months.
If you are bitten by a midge, a local reaction can manifest itself in three types of rash:
- Acute erythematous reaction. It looks like erysipelas, but there is no fever.
- Vesicular bullous rash.
- Necrotic with transition to the formation of scar tissue.

After bites from blood-sucking parasites, general reactions develop only in a small proportion of people.
They occur relatively easily, usually the patient complains of headache, nausea, weakness, upset stool, and there may be fever and bronchospasm.
Types of insectid reactions
Allergy to insect bite: swelling of the skin.
In the clinic, insect reactions are distinguished as follows:
- skin hyperemia and rash. Such slight changes in the skin occur as a result of the bite;
- worsening general condition, nausea and dizziness;
- severe conditions in which bronchospasms and rapid heartbeat are observed;
- anaphylactic shock. The most severe complication of insect allergy, in which there is a sharp decrease in blood pressure and loss of consciousness. The consequence of this condition can be death. Statistics record more than 10% of deaths due to anaphylactic shock. Most of these cases are recorded in elderly people.
Diagnosis
Diagnosis of locally manifested insect reactions is difficult, since toxic reactions have similar symptoms.
Allergy history data are taken into account (whether there were previous reactions to bites, and whether antiallergic therapy helped), and symptoms of skin lesions.
Skin tests are performed using allergens from midges, mosquitoes, and mosquitoes.
Intradermal testing is carried out in special centers. A concentrated solution of the allergen is used - from 10~3 to 10 PNU.
Skin changes are assessed after 20 minutes, then after 6 hours and every other day.
If the reaction appears after 20 minutes, then it belongs to the immediate type, after 6-12 hours to the immunocomplex type, and after 24 hours to the delayed type.
Treatment
Therapy for local reactions to bites by blood-sucking insects is identical to that for allergies to stinging hymenoptera. However, given the prevalence of delayed-type reactions and tissue damage in this form of allergy, calcium and rutin preparations are added to the treatment regimen to reduce vascular permeability, and glucocorticosteroid therapy is intensified. The doses of drugs administered depend on the severity of the reaction.
Pre-season specific hyposensitization with insect allergens for allergies to insects of the order Diptera is carried out according to the same principle as for allergies to stinging Hymenoptera.











