Allergic rhinoconjunctivitis is a pathology of the body that causes an inflammatory process that affects the nasal mucosa and conjunctiva of the eyes, manifested by obstruction of the nasal passages.
The main cause of the disease is the allergen. Allergy is one of the most common diseases among the population. Its diagnosis is considered difficult, since allergies are accompanied by other allergic abnormalities. If the body is sensitive to the action of an allergen, this can lead to many other pathologies: asthma, hay fever, dermatitis.
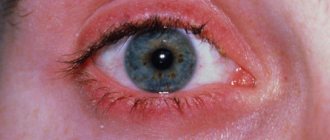
The first barrier that the allergen passes is the conjunctiva of the eye . With this type of allergy, there is itching in the nasal cavity, incessant sneezing, hyperemia, swelling of the conjunctiva of the eyes, lacrimation, sometimes rhinitis, and in rare cases, fear of light. Patients complain of whitish-yellow mucus discharge from the eye area. It gradually turns into a purulent state, which can lead to deterioration of vision.
As a rule, allergic rhinoconjunctivitis is one of the most common diseases.
Basically, the disease is seasonal (spring - summer).
During the flowering period, allergens are especially active. People who exhibit allergic reactions to pollen, dust, and weeds need to be extremely careful. At the first symptoms, the cause of the allergy must be eliminated. Try to have less contact with the allergen and take antihistamines. The disease must be cured completely, and treatment must not be suspended, otherwise the disease may become chronic.
- Drug-induced conjunctivitis is a pathology of the body, the allergen of which is drugs. It appears immediately after taking the medicine. In most cases, it occurs with prolonged use of a drug that causes an allergy. The patient can instantly observe swelling, erosion, and discharge from the eye area.
- Infectious-allergic rhinoconjunctivitis - manifests itself if there is prolonged contact with toxins, caused by fungi. Symptoms are mild and, as a rule, become chronic.
- Polinous rhinoconjunctivitis or hay fever is a pathology whose allergen is pollen from flowering plants. This type of allergy is characterized by immediate activity. The symptoms are clearly visible and are often combined with other allergic reactions.
- Large-papillary rhinoconjunctivitis is a pathology in which there is prolonged contact of the eye with a foreign body (contact lenses). Mostly itching, burning, and a sensation of a foreign body in the eye are observed.
Allergic conjunctivitis in modern society
The conjunctiva is a transparent thin membrane that lines the inside of the eyelid and covers the sclera of the eyeball.
Allergic conjunctivitis is an inflammatory disease of the conjunctiva of the eyes, which is caused by the body's responses to contact with an allergen. As a result, swelling and hyperemia (redness) of the mucous membrane of the eye, lacrimation, swelling and itching of the eyelids, as well as photophobia, develop. This pathology is otherwise called “red eye disease”, since red and swollen eyelids are the most characteristic symptom.
Allergic conjunctivitis is a fairly significant problem in modern ophthalmology and allergology. Allergic eye damage with the development of conjunctivitis occurs in approximately 90% of cases, less often it is accompanied by allergic blepharitis or keratitis, eyelid dermatitis, neuritis, and retinitis. It is also often combined with other allergic diseases (for example, bronchial asthma, rhinitis, atopic dermatitis). This pathology is observed mainly in young people of both sexes. Mostly allergic conjunctivitis in children manifests itself at the age of three to four years. Among schoolchildren it occurs in approximately 5% of cases.

Common forms of pathology
The development of the inflammatory process is possible for a variety of reasons. Depending on this, doctors distinguish several forms of pathology. These include:
- seasonal conjunctivitis – this form of pathology is also called hay fever or pollen allergy. An exacerbation of pathology is observed against the background of flowering plants and the release of pollen into the air. Typically, the peak of the disease occurs in the summer months, although some patients experience exacerbations in early autumn, during the flowering period of meadow grasses;
- The spring form is a fairly rare form of pathology. The reasons for its occurrence still remain poorly understood. In fact, this species has nothing to do with the time of year. The disease develops in adolescents during puberty and is most likely associated with fluctuations in hormonal levels;
- large-papillary form - in this case, the main reason for the development of pathology is the wearing of contact lenses and ocular prostheses. Constant contact of a foreign body with the mucous membrane provokes an inflammatory process. The disease can also be complicated by formations on the upper eyelid resulting from calcium deposits in the cornea;
- dosage form is a local allergic reaction that occurs in response to taking certain medications. Most often, pathology develops against the background of uncontrolled use of antibacterial ointments and eye drops;
- chronic form - occurs in more than 23% of cases of the total number of forms of allergic conjunctivitis. The disease is characterized by a long course and frequent alternation of periods of exacerbation and remission. Allergens in this case are usually house dust, animal hair, perfumes, cosmetics, household chemicals and much more. Often the chronic form is observed in patients with bronchial asthma.
Causes
The cause of any type of allergic conjunctivitis is undoubtedly contact with an allergen. The role of the latter can be substances of various natures.
Causes of year-round conjunctivitis
Year-round conjunctivitis is caused by the following factors:
- fur of pets (dogs, cats, rodents) and feathers of birds (canaries, parrots, etc.);
- various household chemicals;
- house dust, as well as dust mites contained in it;
- bacteria and fungal spores that appear due to high humidity in the house.
Irregular cleaning, dry air and insufficient ventilation in the room also contribute to the deterioration of the condition of a child with this type of conjunctivitis.
Infectious-allergic conjunctivitis can be caused by various microbial agents - viral, bacterial, fungal.
Causes of seasonal conjunctivitis
Seasonal allergic conjunctivitis occurs at certain times of the year and can be caused by several factors:
- Poplar fluff;
- pollen of flowering plants.

The contact type is caused by direct interaction with the allergen:
- cosmetics (cream, mascara, etc.);
- solutions for contact lenses;
- medicines - ointments, drops, gels, anesthetics (a reaction can occur to the active substance and to preservatives that are part of the drug).
This type can also include the so-called hyperpapillary conjunctivitis. It occurs when the eye is irritated by some foreign body (soft contact lenses, sutures, ocular prostheses).
Less commonly, allergic conjunctivitis can be caused by volatile compounds (paints, varnishes) or tobacco smoke. In addition, it may result from a reaction to foods (fruits, especially citrus fruits, chocolate, nuts, milk and honey), including pet food.
Pollen from the following indoor and wild plants is dangerous in the development of allergic conjunctivitis: lily, ragweed, wormwood, all types of geranium, ferns, rhododendron, oak, alder, poplar, birch.
Causes of the disease
As noted above, the disease can develop at any time of the year. There are three groups of allergens that can provoke the development of pathology. These include:
- household allergens - dust, feather particles from pillows, dust mites, etc.;
- pollen - usually distributed in strictly defined seasons, for example, spring or summer. In rare cases, it is possible to develop allergic conjunctivitis when indoor plants bloom;
- epidermal are allergens of natural origin. These include animal hair and dander, particles of bird feathers, remnants of pets’ natural excretions, etc.

After the allergen hits the mucous membrane, the body’s response occurs almost immediately. An unpleasant sensation of a foreign object appears in the eye, itching, burning and redness develop. In some cases, patients complain of dryness, although in the vast majority of cases, conjunctivitis is accompanied by lacrimation. In the absence of timely help, photophobia occurs, infection joins the inflammation and a purulent-inflammatory process develops. In this case, in addition to antihistamine therapy, antibiotics may be required.
Classification of allergic conjunctivitis
It is customary to distinguish several types of allergic conjunctivitis:
- year-round - can occur after just a few hours or days from the moment of contact with a certain allergen;
- seasonal (so-called hay fever) - develops as a consequence of a reaction to pollen; it is characterized by the fact that its symptoms appear strictly at the same time every year;
- conjunctivitis with papillary hyperplasia - the cause of its development is often the continuous or long-term use of contact lenses (protein compounds that are present in normal secretions accumulate on the inside of the lenses and change their structure; if a person has a tendency to allergies, it provokes development of a local immunological reaction in the form of the formation of papillae on the eyelids, namely their inner surface);
- vernal keratoconjunctivitis (the so-called spring catarrh) is most common in childhood and much less common in people over 20-25 years old, while the incidence is twice as high among boys; symptoms appear annually in warm weather, the total duration of the disease is from four to ten years; this type of allergic conjunctivitis in children is most dangerous because the pathological process can affect the cornea of the eye;
- atopic keratoconjunctivitis - this form is more typical for adults and manifests itself with a chronic course. It poses the greatest danger due to the high likelihood of complications (corneal ulcers, blepharitis and retinal detachment). This form of conjunctivitis is also characterized by the simultaneous development of allergic rhinitis.

Causes that can cause allergic rhinoconjunctivitis
You can list for a very long time the list of allergens that can cause this disease. As already mentioned, for the summer-autumn period allergens are plant pollen; dust and even weeds can provoke this reaction. Temperature conditions may enhance these effects. In hot weather, allergens are more active.
For the year-round form, allergens are mites, dust mites, and mold fungi play a special role. There are several main causes that cause this disease:
- Household (dust, mites).
- Pollenaceae.
- Chemical. Such allergens include all washing and washing substances (powders, soaps, detergents), as well as cosmetics. To check if you are allergic to cosmetics, you need to apply the cosmetics to a small area of your wrist and wait 2 minutes. If you have redness or burning in this area, then cosmetics are clearly not suitable for you.
- Food. Recently, an increased amount of allergens has been observed in food products. The most common allergens are citrus fruits. Eating large quantities of such foods is not recommended.

Symptoms
Allergic conjunctivitis in a child appears quite quickly when an allergy occurs. This disease causes him quite a lot of discomfort. Often, no more than a day passes from the moment of contact with the allergen to the development of inflammation in the eyes. The severity of the pathological process primarily depends individually on the characteristics of the child’s body and on the form of the disease.
Allergic conjunctivitis affects both eyes at once. The inflammatory process always begins with increased lacrimation and photophobia.
Severe hyperemia (redness). The smallest vessels of the eye protrude greatly due to the inflammatory process. In severe cases, there may even be hemorrhages in the eyes, but they are quite rare. The process is always two-way. With allergic conjunctivitis, one eye is not affected.
Swelling of the eyelids. In addition to the mucous membrane, the allergic process generally affects all structures of the eye. The eyelids swell quite a lot, making it difficult for babies to open and close them, and attempts to do this bring severe pain.
Severe lacrimation occurs throughout the disease. As a rule, the discharge from allergic conjunctivitis is light and released in large quantities. In the classic version of the disease, there is no pus. It appears only when bacterial flora is attached.
The sensation of a foreign body or “sand” in the eyes is a fairly common symptom of allergic conjunctivitis. Sensing a foreign object, the child begins to blink more often in order to remove it. But this action brings him only temporary improvement.
Characteristic appearance. In children with an allergic reaction, facial features change significantly. It becomes puffy and takes on a red tint. Drooping, heavily swollen eyelids give a sullen appearance to the expression. Less commonly, swelling of the lips and tongue may even occur. In case of such development of the disease, the baby must be treated immediately. If his face is swollen, he must urgently call an ambulance.
Behavior change. During the acute period, children refuse their favorite foods and become very lethargic. Babies often cry and are very capricious, and the smallest children often ask to be held in their arms.

Diagnosis of allergic conjunctivitis
If an allergic disease of the conjunctiva of the child’s eyes is suspected, several doctors should examine:
- pediatrician;
- allergist-immunologist;
- pediatric ophthalmologist;
- otorhinolaryngologist (ENT).
The doctor talks with the parents, finds out the time of onset of the first symptoms and the nature of the disease. A very important point is to clarify whether the parents of the sick child suffer from any allergic reactions. Often, pronounced signs of allergic conjunctivitis allow doctors to make an accurate diagnosis quite correctly and quickly. However, in the case of an allergic reaction and inflammatory eye disease, additional laboratory tests are necessary.
A general blood test is one of the most important research methods. With its help, you can clarify the severity of the pathological process. An increase in eosinophil levels indicates an allergic reaction. This simple and at the same time informative test helps to distinguish allergies from viral or bacterial conjunctivitis.

In order to accurately determine which allergen provokes the development of the disease, additional laboratory tests are required. Allergists most often use so-called prick tests. They can be used only a couple of weeks after the acute process has subsided. To do this, small cuts are made on the skin with a small sharp object (scarifier), and then several drops of different allergens are applied to them. If a child is allergic to any of them, then moderate redness will be observed at the site of such a scratch. The doctor analyzes the results and determines which allergen is most dangerous for the child. This procedure is painless and safe, so it is used for children of all ages.
Serological blood testing is currently one of the most reliable and informative tests. In this case, venous blood is taken for examination. As a rule, the results are ready within 3 to 5 days. This laboratory method with a probability of almost 95 - 98% will indicate the subject’s tendency to allergies caused by a specific provoking factor. This method can test almost all allergens that exist today.
In order to establish the cause of conjunctivitis, an elimination test is also carried out, when, against the background of symptoms, contact with the suspected allergen is excluded, as well as an exposure test, which consists of repeated exposure to a certain allergen after the symptoms have subsided.
Carrying out a full range of all diagnostic methods is an important condition for accurately identifying the cause of the allergic reaction. In case of allergic processes, therapy should be carried out immediately. And the slightest delay can greatly increase the development of dangerous complications.

Diagnostics
Diagnosis of allergic conjunctivitis is carried out simultaneously by an ophthalmologist and an allergist-immunologist, who should conduct treatment. It includes several stages:
- collection of information - complaints of mother and child, family history;
- identifying the exact causes of the disease - the connection between external irritating factors and the child’s reaction;
- clinical picture - examination;
- microscopic examination of discharge from the eyes, where eosinophils are always found during an allergic reaction;
- general clinical blood test, in which the level of eosinophils is also increased;
- blood test for specific immunoglobulin E;
- performing skin allergy tests (patch test, skin prick test, scarification test and scarification-patch test) in order to clarify the allergen - used only for children over 4 years of age;
- a blood test from a vein to determine the range of substances to which the child is allergic;
- nasal, conjunctival and sublingual tests are performed rarely and only during remission;
- accompanying examinations of the child’s gastrointestinal tract, stool testing for worm eggs and scrapings for enterobiasis.
Complications
Allergic conjunctivitis in children can not only develop into a chronic form, but can even provoke quite serious visual impairment. Some of them are practically untreatable. However, it is possible to reduce the likelihood of complications only with complete and timely therapy.
The consequences of allergic conjunctivitis can be the following conditions:
- addition of infection;
- significant visual impairment;
- retinal detachment;
- keratitis;
- corneal ulcer.
Treatment of allergic conjunctivitis
Treatment is carried out in two main stages. To begin with, it is necessary to identify the very allergen with which the child must be excluded from contact. After this, medications are prescribed to eliminate clinical manifestations and strengthen local immunity.
Drug therapy is prescribed in accordance with the severity of the symptoms of the pathological process, as well as the individual characteristics of the sick child’s body. The necessary medications should be selected exclusively by a doctor. Incorrect selection of medications can significantly reduce the effectiveness of treatment and even cause prolonged therapy.
Main groups of drugs
For allergic conjunctivitis, the following types of drugs can be prescribed:

- antihistamines (Loratadine, Zyrtec, Claritin);
- drops with a membrane-stabilizing effect (Ketotifen, Lecrolin);
- in the presence of dry eye syndrome, tear substitutes (Defislez, Inoxa) are used, and in case of corneal damage, drops with vitamins and dexpanthenol are used;
- histamine receptor blockers (Opatanol, Allergodil);
- mast cell stabilizers in the form of drops (Lodoxamide, Krom-Allerg);
- severe forms of the disease may require the prescription of non-steroidal anti-inflammatory drugs (eye drops with diclofenac), as well as corticosteroids (drops, ointments with dexamethasone or hydrocortisone);
- persistently recurrent conjunctivitis of allergic origin is an indication for specific immunotherapy.
Eye wash
In every case of treatment of allergic eye diseases, eye rinsing is used. This procedure should be repeated at least two to three times a day. If the child has severe lacrimation, the eyes should be washed much more often (as necessary).
Hypoallergenic diet
Compliance with a therapeutic hypoallergenic diet. For children who are prone to allergies, experts recommend mandatory adherence to such a diet throughout their lives. Avoiding foods that trigger allergic reactions helps prevent new cases of the disease. A diet enriched with protein and all necessary substances helps strengthen the baby’s immunity and has a positive effect on his growth.
Correct daily routine
During the acute period of the disease, you should not give the child heavy loads. It's better for him to gain strength and sleep more. During daytime sleep, children's allergy symptoms decrease, and the functioning of the immune and hormonal systems is normalized. When a child closes his eyes, the aggressive effect of sunlight on the affected mucous membrane weakens.

Treatment

At the same time, the child is prescribed oral and local antihistamines. Treatment of allergic conjunctivitis should be carried out in three directions at once:
- immediate cessation of contact with the allergen;
- local therapy with antihistamines, and in severe cases, corticosteroids;
- immunotherapy.
In mild cases, only local treatment is prescribed, and in severe cases of the disease, complex therapy is necessary:
- locally – cold compresses on the eyelids;
- orally - antihistamines in the form of tablets and children's syrups (Claritin, Loratadine, Cetrin, Telfast, Zyrtec, etc.);
- antiallergic eye drops - Opatanol, Lecrolin, Allergodil, Histimet (it should not be prescribed to children under 12 years of age);
- antihistamine drops - histamine blockers: Hi-chrome (cannot be prescribed to children under 4 years of age), Lodoxamide, Krom-Allerg, Lecrolin, Cromohexal, Alokomide (contraindicated for children under 2 years of age);
- for dry conjunctiva, tear substitutes are prescribed - Oksial, Oftolik, Vidisik, Inox, Oftogel, Systane, Visin;
- if the cornea is damaged, drops with vitamins are indicated (Taufon, Quinax, Katachrom, Emoxipin, Catalin, Khrustalin, Vita-Iodurol, Ujala);
- in severe cases, when other drugs do not give the desired effect, the doctor prescribes eye drops and ointments with corticosteroids (Hydrocortisone and Dexamethasone);
- when a secondary infection occurs, the prescription of eye drops with antibiotics is indicated;
- in case of constant relapses of the disease, specific immunotherapy drugs are used, for example, Histaglobulin;
- There is also allergen-specific therapy, which consists of administering small doses of the allergen in increasing concentrations, which allows the body to become accustomed to it, and ultimately leads to a weakening or complete disappearance of allergy symptoms.
Treatment regimens for various types of allergic conjunctivitis:
- for hay fever conjunctivitis, Allergodil, Spersallerg help - 3-4 times a day at the beginning of the disease, then they switch to double instillation, and for a chronic course of the process - Cromohexal and Alomide 3-4 times a day;
- for chronic allergic conjunctivitis - Cromohexal, Alomide 2-3 times a day and Spersallerg 1-2 times a day;
- for spring catarrh, in addition to Alomide and Cromohexal, a drug with dexamethasone is prescribed - Maxidex, and also in acute conditions Allergodil 2 times a day; at the same time, you can prescribe antihistamines in tablets - Claritin, Cetrin, Zodak and immunotherapy - 6-10 injections of histaglobulin;
- drug allergic conjunctivitis begins to be treated by discontinuing the drug that caused such a reaction, then antiallergic drugs are prescribed internally - Loratadine, Claritin, Cetrin - 1 tablet per day, as well as eye drops - Spersallerg or Allergodil - 2-3 times a day; in case of subacute or chronic process, it is better to instill Cromohexal or Alomide 2-3 times a day.
In any case, you should not self-medicate or prescribe medications to your child without consulting a doctor.
Prevention of allergic conjunctivitis
In order to prevent this disease, it is necessary, if possible, to exclude the child from contact with known allergy-provoking factors. In case of seasonal forms, preventive courses of desensitizing therapy are necessary. Patients who suffer from allergic conjunctivitis should definitely be observed by an allergist and ophthalmologist.
It is no secret that any disease is much easier to prevent than to treat. That is why parents should carry out the activities listed below:
- frequent ventilation;
- regular wet cleaning of premises;
- exclusion from the child’s menu of foods that can cause allergies (chocolate, brightly colored fruits and vegetables, berries, honey, nuts), as well as products that contain dyes, preservatives or other chemicals;
- excluding contact of a sick baby with possible allergens - flowering plants, pets;
- if possible, abolishing household chemicals;
- strengthening the child’s immunity;
- preventive courses of desensitizing therapy;
- regular observation by an allergist-immunologist.