Emergency resuscitation during transportation
If there is an oxygen blanket in the house, use it.
If it is difficult for the patient to breathe on his own, “forced” breathing is performed - the chest is carefully compressed while exhaling, accelerating the process of releasing accumulated air. If medications are available, they must be used before providing qualified assistance, even if they do not objectively improve the general condition
Inhalations are carried out using the following means:
If medications are available, they must be used before providing qualified assistance, even if they do not objectively improve the general condition. Inhalations are carried out using the following means:
- Salbutamol;
- Berotek;
- Alupent;
- Ventolin;
- Ditek;
- Izadrin.
If the patient's condition allows, it is necessary to give him a lot of fluid to drink to thin the sputum.
After the ambulance arrives, the tactics of providing assistance depend on the type of asthmatic status.
Since beta-adrenergic receptors are blocked when the status develops, the basis for emergency care is the administration of Eufillin.
Algorithm for using the drug:
- Start with the minimum allowable dosage. In the first stage of the status, in most cases, Eufillin alone is sufficient. The drug is administered by infusion (intravenous drip along with saline solution).
- At the second stage, hormones (glucocorticosteroids) are added to Eufillin. Dosage of Prednisolone 2-3 mg/kg.
- In stage 3 status, the amount of hormonal drugs is increased to 3-4 mg/kg. Resuscitation measures are being intensively carried out.
If the patient has severe heart failure, glucose-based Strophanthin is administered intravenously. For status asthmaticus in children, the dosage of Eufillin is reduced by 20%.
Emergency care for status asthmaticus before hospitalization should be carried out by a specialized team.
Pre-hospital stage

Upon arrival to the patient, the doctor or paramedic assesses his condition (based on the history and physical examination). It is necessary to take into account the time that has passed since the onset of the attack, the probable factors of its development and the response to previous therapy. The severity of exacerbation is assessed clinically and based on functional methods (peak flowmetry).
The goal of treatment measures at the prehospital stage will be to reduce bronchial obstruction and restore patency of the respiratory tract. For status asthmaticus, the emergency care algorithm includes:
- Inhalation of humidified oxygen.
- Inhalation administration of salbutamol or Berodual.
- Glucocorticoids orally or intravenously (prednisolone, dexamethasone).
Alternatively, you can inhale drugs through a spacer or nebulizer (salbutamol, fenoterol, Pulmicort). If this is not possible, then aminophylline and prednisolone are sequentially administered intravenously. All this is carried out during the examination and during emergency transportation of the patient to the hospital.
Urgent Care
Asthmatic status.
— This is a syndrome of acute respiratory failure that developed in patients with bronchial asthma due to airway obstruction, resistant to bronchodilator therapy.
Frequent causes of status asthmaticus are excessive consumption of sleeping pills; sedatives; taking medications that cause an allergic reaction in the bronchi (salicylates, analgin, antibiotics, etc.); excessive intake of inhaled bronchodilators (more than 6 times a day); inflammatory diseases.
Stage I: suffocation increases, the attack is not controlled by inhaled antispasmodics or bronchodilators, pain in the heart and palpitations appear, and blood pressure rises. On auscultation there is an abundance of dry whistling rales.
Stage II: breathing becomes frequent, shallow, the amount of dry wheezing in the lungs decreases until they disappear (“silent lung”). Blood pressure decreases, bradycardia.
Stage III: the patient loses consciousness and falls into a coma (if treatment was inadequate)
1. Control of vital functions.
2. Give the patient a comfortable half-sitting position
3. Unbutton tight clothing and provide oxygen access
4. With preserved consciousness, inhalation of berodual + 30-40% humidified oxygen
5. Prepare everything necessary for IV administration: 5% glucose solution IV, 60-150 mg prednisolone IV, 2.4% aminophylline solution 10 ml drip in 20 ml 0.9% sodium chloride solution; in the absence of consciousness and respiratory depression: intravenous 0.18% adrenaline 0.3 ml every 20 minutes until a bronchodilator effect is obtained
6. Prepare an Ambu bag and ventilator.
Information: A patient with bronchial asthma suddenly developed an attack of suffocation. The patient sits with his hands on the back of the chair, wheezing, “distant” dry wheezing, cough with sputum difficult to separate. The chest is swollen, auxiliary muscles are involved in the act of breathing, rapid breathing, tachycardia.
Nurse tactics
| Actions | Rationale |
| 1. Call a doctor through a third party. | To provide qualified medical care |
| 2. Calm down, unfasten tight clothing, provide access to fresh air, give a comfortable position with emphasis on your hands. | Psycho-emotional relief, reduce hypoxia |
| 3. Monitoring blood pressure, respiratory rate, pulse. | Condition monitoring |
| 4. Give 30 - 40% humidified oxygen. | Reduce hypoxia |
| 5. Inhale Berotec (salbutamol): 1-2 breaths of metered-dose aerosol. | To relieve bronchospasm |
| 6. Before the doctor arrives, the patient should be prohibited from using his pocket inhaler. | To prevent the development of resistance to bronchodilators and the transition of an attack to status asthmaticus |
| 7. Give hot drinks, make hot foot and hand baths. | For reflex reduction of bronchospasm |
| 8. If the above measures are ineffective, administer parenterally as prescribed by a doctor: aminophylline 2.4% solution 10 ml; prednisolone 60-90 mg. | For relief of moderate and severe attacks |
| 9. Prepare for the doctor’s arrival: Ambu bag, ventilator. | To carry out resuscitation measures if necessary |
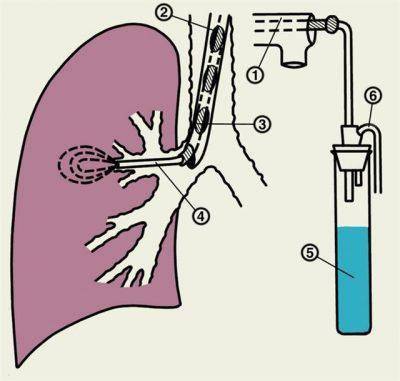
If there is no effect and signs of status asthmaticus appear, see emergency care. The patient is hospitalized for treatment in the intensive care unit (resuscitation). In the department, if necessary, the patient is given artificial ventilation (ALV). When performing mechanical ventilation, the nurse evacuates mucus from the respiratory tract with an electric suction every 30-40 minutes and irrigates them with an alkaline solution.
Manifestations
The classification of status asthmaticus is determined depending on the severity of the patient’s attack:
- Stage of relative compensation. The patient's consciousness is clear, perception is adequate. There may be signs of euphoria followed by fear. The patient takes a forced “coachman” position - a sitting position, resting his hands on a chair or bed. Central cyanosis of the skin and increased breathing up to 40 movements per minute are observed. Exhalation is difficult and impossible. When listening to the chest, dry whistling rales are clearly audible; they can be recognized at a distance. Auscultation of the heart determines muffled and increased frequency of sounds. The patient's blood pressure may increase. Rapid breathing
- Stage of decompensation. The patient's condition is assessed as serious. The patient is still conscious, but reacts inadequately to what is happening around him. Cyanosis of the body is pronounced, swelling of the veins of the neck is observed. Tachypnea - more than 40 respiratory movements per minute. The phenomenon of “silent lung” is noted - noisy breathing can be heard at a distance, but nothing can be heard on auscultation. Tachycardia is pronounced (110-120 beats), pulse is thread-like, pressure drops. The patient's heart sounds are barely detectable. The electrocardiogram shows typical signs of overload of the right side of the heart; atrial fibrillation or other types of heart rhythm disruption are possible. There is no effect from the use of bronchodilator medications.
- Hypoxemic or hypercapnic coma. The patient’s condition at this stage of the attack is extremely serious, there is no consciousness, but reflexes are preserved. Characterized by attacks of tonic and clonic convulsions. The pupils are wide, the light reaction is reduced. Tachypnea gives way to bradypnea. “Mute lung” is detected in all places of the chest. Heart rate is more than 140 beats per minute, pulse can be felt only in the carotid and femoral arteries. Heart sounds are dull. Blood pressure has been reduced to levels at which it is no longer detectable. Right ventricular failure develops. Dehydration sets in. If assistance is not provided, clinical death occurs.
Memo for the patient
The only person who can best care for a patient's condition is the patient himself. To prevent another attack from causing many difficulties and causing death, the patient must always have with him a certain set of medications and means for providing first aid. It is much easier to help a patient at home, since the patient is in his usual conditions, and the medications are nearby. But an attack can occur while walking in the park or while going to the store.
Emergency conditions for bronchial asthma do not pose a danger if the patient is prepared for them in advance. It is recommended to visit a doctor who will write out recommendations and prescribe the dosage of medications. Such drugs should always be nearby, which will repeatedly save the patient’s life.
In order for first aid during an attack to lead to a positive result, the patient’s first aid kit must necessarily consist of the following components:
- Solutions for injections.
- Hormonal and antihistamines.
- An aerosol is required for inhalation.
Particular attention is paid to inhalers, since they allow the drug to quickly enter the patient’s body. Conventional devices are represented by spacers
This model increases the likelihood of penetration of the drug component into the lungs. Special devices – nebulizers – are often used. They are a modern model of a spray device. The device converts the liquid component into a medicine in the form of a suspension, which will provide better atomization. The devices can only be used at home, so emergency care for bronchial asthma using these devices is performed at home. This is due to their size, since the dimensions do not allow for comfortable transportation of the device.
Assistance and diagnosis
In case of status asthmaticus, the patient must be subjected to a thorough step-by-step diagnosis in order to assess the need for emergency care. The list of measures taken for this includes: clarification of the details of clinical symptoms, a comprehensive examination by a pulmonologist. Next, it is necessary to determine the absence or presence of an effect from the medicinal components used. Symptoms will indicate the presence of status asthmaticus and when emergency treatment is needed.
In addition, modifications in the gas composition of the blood are identified, peak flowmetry (reduction in the volume of inhaled air) and consultation with a resuscitator are carried out. To clarify the nuances of the condition, it is recommended to conduct fluorography and chest x-ray.
Taking into account the diagnostic data obtained and the existing symptoms, the pulmonologist prescribes a rehabilitation course. It should be noted that it is advisable to carry out diagnosis at the initial stage of development of the pathology, as well as 1-2 times within 12 months. This will indicate the effectiveness of the restoration process, which previously could not be removed.
Diagnostics
Auscultation
- analysis of clinical features, careful collection of anamnestic data and physical examination (auscultation, palpation and percussion data) are the most important components of a correct diagnosis at the prehospital stage;
- In a hospital, the examination is supplemented by diagnostic laboratory and instrumental methods.
Laboratory
There is only one informative method in diagnosing an attack of status asthmaticus - an analysis to determine the acid-base balance of the blood (ABC). Using it, the following indicators are determined:
- oxygen level (hypoxia is pronounced);
- amount of carbon dioxide (hypercapnia is observed);
- pH (metabolic acidosis develops).
The analysis is necessary not only to establish a diagnosis, but also to assess the severity of the condition and monitor the effectiveness of treatment for an attack.
Analysis of the acid-base balance of the blood
A clinical blood test, in which mild eosinophilia is found, sputum examination and determination of immunoglobulin E, are uninformative. Sputum in status asthmaticus is scanty, and specific Charcot-Leyden crystals and Courshman spirals can be found in it.
In case of a severe ongoing asthma attack, an electrocardiogram must be performed and blood pressure measured.
Differential
The differential diagnosis of status asthmaticus should be carried out with several emergency conditions - more details in the table.
| Sign | Clinic | Anamnesis | Survey |
| Asthmatic status |
|
|
|
| Cardiac pulmonary edema |
|
|
|
| PE (Pulmonary embolism) |
|
|
|
| Pneumothorax |
|
| Auscultation – breathing is weakened or cannot be heard on the affected side. |
| General anaphylaxis |
| Contact with a potential allergen. | Auscultation and percussion are normal variants. |
| Foreign body |
|
| Auscultation and percussion are normal variants. |
In childhood, when diagnosing a severe, prolonged attack of bronchial asthma, it is necessary to differentiate it from acute bronchitis and pneumonia, since they occur with signs of severe respiratory failure.
Specifics of first aid
Most often, an asthma attack occurs in people who have bronchial asthma or regularly suffer from various forms of bronchitis. You can recognize the onset of an attack by some symptoms.

- suffocation;
- frequent, wheezing breathing;
- long exhalation of air;
- dyspnea;
- cyanosis of the skin;
- dry cough, sometimes with sputum.
In rare cases, a cough with a small amount of sputum may be observed. First aid should be provided in a timely manner during deterioration in which symptoms increase.
The consequences of this condition may be as follows:
- Pneumonia;
- Coma;
- Subcutaneous emphysema, after which suffocation and oxygen starvation develop.
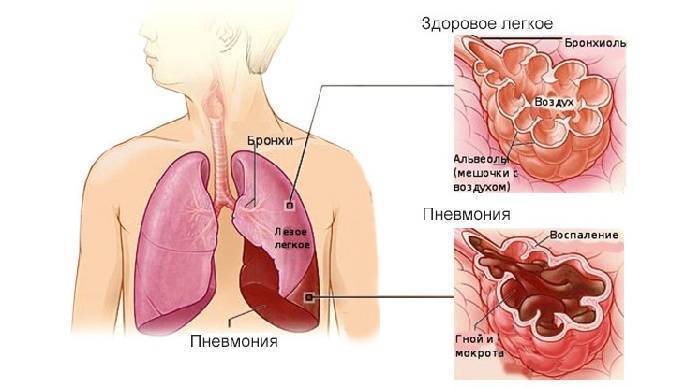
Inflammation of the lungs (pneumonia)
If a patient develops status asthmaticus, emergency care is vital: incorrect or untimely provision of first aid can lead to the patient dying. Therefore, it is so necessary to promptly diagnose the onset of status asthmaticus and quickly relieve the attack.
Pre-medical actions Algorithm for providing first aid during status asthmaticus before the doctor arrives:
- If a person has an asthma attack for a long time and symptoms increase, then first of all it is necessary to call a team of medical workers.
- After this, the person should be provided with peace and access to fresh air (open the window, step aside).
- If a person’s clothes are in the way, they should be unbuttoned or removed.
- In the event of an attack provoked by allergens, you must try to eliminate them (remove the animal, flowers or food that caused the exacerbation).
- You need to help the person take a comfortable position and give him an inhaler.
Such actions will alleviate the patient’s condition until the arrival of medical workers who will provide him with qualified emergency care.
Medical emergency
To provide emergency care, special knowledge is required, so these manipulations can only be carried out by people with medical education.
If status asthmaticus occurs, then emergency care involves the following algorithm of actions:
- The patient is placed in a comfortable position and his head and shoulders are elevated. This can be done with special beds or ambulance equipment.
- The patient is put on a nasal catheter or a mask through which humidified oxygen is supplied.
- The doctor conducts a survey of the patient’s relatives to clarify information about the therapy performed before the onset of status asthmaticus and the dosage of drugs.
- The patient is given inhalations through a mask or using special aerosols (Salbutamol, Berotek).
- Intravenous or intramuscular injections are required to administer adrenergic agonists (Bricanil, Terbutaline).
- If the patient behaves restlessly, he is given sedatives like Diazepam. In this case, children are injected with Sodium hydroxybutyrate into a vein.
A person with a seizure is transported to the hospital by ambulance as an emergency.
If the patient’s condition worsens, disappears or there is no reaction to the measures taken, then doctors ventilate the pulmonary system.
It is necessary in the following cases:
- rapid drop in blood pressure;
- loss of consciousness;
- the patient falls into a state of doubt;
- when a generalized type of cyanosis is detected;
- with weak respiratory activity.
Doctors' actions must be accurate and timely. This will help avoid complications and death.
Treatment methods for status asthmaticus
When choosing treatment, the form and severity of the attack are taken into account.

The main directions in resuscitation actions for metabolic status:
- drug therapy;
- infusion therapy;
- oxygen therapy.
Drug treatment involves the complete exclusion of adrenergic stimulants, the prescription of large doses of hormonal drugs, and the use of bronchodilators (Eufillin and its analogues).
Treatment methods for stage 1 attack
Massive supply of glucocorticosteroids in status asthmaticus is aimed at reducing the inflammatory process and restoring receptor sensitivity. Drugs (Prednisolone, Dexazone) are prescribed intravenously at a dosage of 1-1.5 g per day for a body weight of at least 60 kg. Initially, 60-90 mg is administered, then 30 mg every 2-3 hours. This scheme allows you to quickly stop the signs of suffocation, make the cough effective (productive), cause the appearance of sputum, and restore the patency of the bronchial tree.
To enhance the effect, hormones are simultaneously prescribed for oral use (orally). After removing the patient from status asthmaticus, the number of intravenous infusions is reduced by 25%, and oral medications are taken according to the same regimen.
Eufillin is indicated for dilation of the bronchi. The initial single dose is 5-6 mg/kg. Maintenance therapy involves the use of 0.9 mg/kg 2-3 times a day, while the daily dose should not exceed 2 g.
Since the status indicates increased myocardial dynamics, patients are prescribed cardiac glycosides. They help normalize heart function and restore physiological blood circulation in the vascular bed.
To thin the mucus and remove it faster, the patient drinks a warm alkaline drink (mineral water) and undergoes a course of chest percussion massage (tapping).
Treatment necessarily includes oxygenation. An air mixture with an oxygen content of 30 to 40% is prescribed. A nasal cannula is inserted into the patient through the nasal passages and connected to the device. Feed rate 4 l/min. The duration of one oxygen therapy session is on average 15-20 minutes.
To replenish lost fluid and prevent dehydration, infusions are made with plasma exchange solutions to normalize blood properties - glucose, Poliglyukin, Reopoliglyukin. On the first day, 3-4 liters are administered intravenously. Heparin is additionally added to the system to thin the blood and improve its rheological properties.
Treatment methods for stage 2 and stage 3 status
In the second stage of status asthmaticus, the same drug treatment is indicated as described above. But at the same time the doses of hormonal drugs are increased. Glucocorticosteroids are administered at 90-120 mg every hour.
The patient is connected to a gas mixture supply apparatus: helium 75%, oxygen 25%.
The procedure is performed under anesthesia.
Treatment of patients in the third stage is carried out jointly with resuscitators. Patients with progressive respiratory failure and hypercapnic coma are connected to a ventilator. Oxygen is given after tracheal intubation. The endotracheal tube is washed every half hour to avoid infection and the development of an inflammatory process in the respiratory tract. The amount of systemic hormones is increased to 300 mg every 3-5 hours.
The development of status asthmaticus is an alarming signal that requires urgent help. Even after successful relief of an attack, an unfavorable outcome may occur over time. The status indicates a deterioration in general condition, progression of the disease and loss of asthma control.
Emergency care in a medical facility

Providing emergency medical care for bronchial asthma in a hospital setting is considered the most effective. The presence of qualified specialists and the necessary equipment in the clinic allows us to cope with even the most severe cases.
If after all treatment measures a positive result is observed, the patient is given recommendations and sent home. However, if the doctor doubts the stability of the patient’s condition, he is left in the hospital for further examination and observation.
Nursing assistance

Providing emergency care for an attack of bronchial asthma begins immediately upon arrival at the hospital. The patient’s medical record is first studied, which contains data on the course of the pathology, medications taken and substances that cause allergies.
Measures to provide assistance for bronchial asthma are taken by medical personnel. Before the arrival of a patient with symptoms of exacerbation, equipment for artificial lung ventilation and an Ambu bag should be prepared.
Before the patient is examined by a doctor, first aid for bronchial asthma is provided by a nurse. She must follow a certain algorithm of actions:
- Remove the patient's outer clothing and unfasten the collar. Make the patient sit more comfortably. Relaxation of muscles leads to easier breathing.
- Provide a flow of fresh air into the room. If necessary, use humidified oxygen.
- Prohibit the use of the inhaler while the patient has it (to prevent addiction to the drug). You need to use an aerosol based on salbutamol sulfate to relieve spasms.
- Give a warm drink, maybe just water.
While a specialist is examining a patient, a nurse remains nearby to administer medications or perform other medical orders.
First aid

When an acute attack of bronchial asthma occurs, it must be stopped quickly. A person is taken out of this state with the help of medications. All medications and their dosage are prescribed by a doctor. Treatment begins after examining the patient and determining the severity of the pathology.
Providing first aid for an attack of bronchial asthma includes the following actions:
- A subcutaneous injection is given for bronchial asthma. Adrenaline is usually used in the form of a solution or aqueous suspension. After the injection, the muscles relax and the bronchi expand. The drug is not recommended for persons with diseases of the cardiovascular system.
- Drug treatment for an asthma attack includes intravenous corticosteroids. These hormonal drugs relieve swelling and have antihistamine properties.
- To relieve bronchospasm, drugs from the xanthine group are administered intravenously.
- Steam oxygen inhalations are effective. They thin out mucus and facilitate the removal of mucus from the bronchi.
How does status asthmaticus develop - what is the nature of the asthma attack?

For prerequisites to arise, the influence of negative factors is necessary. These may be viral and bacterial infections, disruption of the process of cleansing the bronchi from mucous secretions, or congestion in the lungs. It is very important to note that status asthmaticus can develop gradually, against the background of a regular progressive increase in asthma attacks. At the same time, the patient is forced to increasingly resort to using an inhaler with a bronchodilator.
This leads to a decrease in the effectiveness of the pharmacological agent. The negative side effect of these drugs causes atrophy of the ciliated epithelium lining the bronchi. This circumstance contributes to the disruption of the cleansing function, a gradual accumulation of sputum occurs, and a change in drainage capacity.
It is not uncommon for the uncontrolled use of certain groups of medications to lead to the development of status asthmaticus. For example, in a number of patients the development of suffocation is preceded by the use of acetylsalicylic acid, certain groups of synthetic antibiotics, vitamin-mineral complexes, and non-steroidal anti-inflammatory drugs. It is worthwhile to carefully approach the period of preparation for seasonal and routine vaccination. A vaccine made from chicken protein should be of particular concern.
Let's consider what is the nature of an attack of suffocation in this condition, what provokes these changes and what processes occur in the bronchial and pulmonary tissue. Before status asthmaticus develops in its clinical picture, various changes begin to occur in the patient’s body long before this moment.
It all starts with immunological changes that adjust the entire response system to perceive any allergen as a shock to the target organ. In the case of bronchial asthma, this is the bronchial tree and the lungs, or rather their mucous membranes, suffering from a colossal release of histamines from mast cells under the influence of a trigger.
This response mechanism is gradually consolidated and subsequently, upon any contact with the allergen, the release of mediators occurs, provoking the reaction of mast cell decay. This stimulates the production of large amounts of sputum. The response mechanism of adrenergic receptors that regulate the state of the ciliated epithelium is blocked. As a result of an increase in the concentration of carbon dioxide in the blood, acid-base shifts begin. This increases swelling of the mucous membranes, and suffocation intensifies. And with the subsequent accumulation of carbon dioxide, a spasm of muscle fibers in the intercostal spaces begins. At a certain stage, the patient will no longer be able to take a breath on his own.
Broncho-obstructive syndrome is combined with the accumulation of viscous sputum and hemodynamic disturbances, leading to serious ventilation pathologies. It is this factor that determines the resistance of the bronchial mucous membranes to the effects of bronchodilators and further direct-acting steroid drugs.
In later stages, collapse of small bronchi and bronchioles may occur, which provokes an increase in thoracic internal pressure and reactive pulmonary hypertension. This could trigger a chain reaction. In the cardiovascular system.
Acidemia and hypocapnia are typical for the initial stage of status asthmaticus - hypoventilation of the lungs leads to the accumulation of carbon dioxide in the blood, which can provoke severe suffocation, dizziness, and loss of consciousness. Approximately 20% of patients suffer from an increase in hematocrit and a typical increase in blood viscosity, leading to the formation of thrombi in the pulmonary venous system.
| Clinical manifestations | PaCO level | |
| 1st stage of compensation | obstruction of the bronchial tract | 60/70 mm Hg. Art. |
| Stage 2 progressive | pulmonary ventilation impairment occurs | 50/60 mmHg Art. |
| Stage 3 hypercapnic coma | minimal gas exchange in the lungs, loss of consciousness, lack of spontaneous breathing | PaO = 40/55 mmHg. Art. |
General information
Status asthmaticus is a severe attack of bronchial asthma that lasts for 24 hours or more. It is characterized by severe obstruction of the respiratory tract (due to swelling, spasm, mucus accumulation), increasing respiratory failure and resistance to previous treatment. The main causes of status asthmaticus are:
- Inadequate therapy.
- Constant contact with allergens.
- Respiratory diseases.
- Taking certain medications (beta blockers, non-steroidal anti-inflammatory drugs, antibiotics).
The clinical picture is determined by the severity of respiratory failure and can vary from a prolonged attack of suffocation (with expiratory shortness of breath and wheezing) to a coma. Therefore, status asthmaticus poses a real threat to life and requires urgent measures.
Urgent Care
How can loved ones help?
A patient in status asthmaticus requires qualified medical care. He will not be able to get out of this state on his own. Therefore, relatives of the victim must be able to recognize approaching symptoms and know how the disease develops.
At the first suspicion of a complication of the disease, act immediately.
- The first thing you have to do is call an ambulance. While the doctors are traveling, measures should begin to save the patient.
- An asthmatic needs an influx of fresh air; the windows in the room need to be opened. All clothing that restricts the chest must be removed or unbuttoned. The patient should take a comfortable body position in which it will be easier for him to breathe. Close people should help him with this.
How can a doctor help?
A patient in status asthmaticus needs emergency care. The faster it is provided, the higher the chance of saving a person. Medical care is provided according to a special algorithm:
- The patient should take a comfortable body position. If the patient is lying down, the upper body should be elevated.
- The lack of oxygen is compensated with the help of oxygen therapy; through a mask, the patient receives an additional dose of humidified oxygen from an oxygen cylinder.
- Andrenomimetics are administered subcutaneously or intravenously; this group includes drugs such as Eufillin, Terbutaline, Bricanil.
- In some particularly severe cases, prednisone administration will be required.
- A patient in a state of status asthmaticus is subject to urgent hospitalization. Treatment will continue in the intensive care unit of the hospital.
The further algorithm of actions will be aimed at taking measures that will promote relaxation and expansion of the bronchi. This effect is achieved through drug therapy. The patient is prescribed:
- inhalation through a nebulizer using Salbutamol, Atrovent, Berodual;
- Eufillin is administered intravenously by drip, this medicine reduces swelling in the lungs and relieves bronchospasms;
- severe attacks are relieved with glucocorticoid drugs, this includes prednisolone, or a complex of hydrocortisone and dexamethasone.
If medications fail to alleviate the patient's condition, artificial ventilation will be required. This measure is resorted to extremely rarely, in especially severe cases.
Hospital stage

Further therapy for patients with status asthmaticus is carried out in the hospital. In extremely serious condition, the patient is hospitalized in the intensive care unit and transferred to artificial ventilation. In each case, vital signs of the body are constantly monitored (pulse and respiration rates, gas composition and blood electrolytes, peak expiratory flow). Emergency care for status asthmaticus at this stage consists of the following measures:
- Continuous oxygen therapy (maintaining blood oxygenation at least 92%).
- Inhalation administration of fenoterol (salbutamol, Berodual) through a nebulizer with oxygen (during the first hour every 20 minutes, then every 60 minutes until 4 hours).
- Further use of salbutamol (fenoterol) with ipratropium bromide or Berodual with corticosteroids (methylprednisolone, prednisolone, hydrocortisone) intravenously or orally.
- Nebulizer therapy with budesonide (Pulmicort) three times a day.
If after 4–6 hours there is no effect from the measures taken, then aminophylline is administered by intravenous infusion (drip). Additionally, if there is resistance to bronchodilators, magnesium sulfate can be administered. And in some and extremely severe cases (very carefully), adrenaline is used, administered by subcutaneous injection.
Aspirin-induced asthma requires the use of dexamethasone or triamcinolone. Antibacterial drugs are used only in situations where the corresponding origin of the infection has been proven (macrolides, fluoroquinolones, and latest generation cephalosporins are preferred). In case of status asthmaticus, the following medications should be avoided:
- Sedatives and narcotics.
- Long-acting beta-agonists.
- Antihistamines.
- Mucolytics.
- Plant origin.
Drugs that do not play a significant role in stopping a severe attack should not be used, avoiding polypharmacy (prescribing a large number of drugs). If all of the above measures are ineffective, the patient is connected to a ventilator.
The algorithm of actions for providing care at the hospital stage includes various options for drug support, taking into account the severity of the pathology.
The criteria for discharge from the hospital are complete relief of asthmatic status and weakening of the severity of exacerbation. If ventilation rates are below normal (from 40 to 60%), then patients require further outpatient therapy with constant medical supervision. But in any case, it is important to understand that only strict adherence to medical recommendations and long-term use of basic medications will allow you to achieve control of bronchial asthma and avoid its severe exacerbations.
Source: elaxsir.ru
Principles of inpatient treatment of status asthmaticus

In general, the relief of AS in a hospital does not differ from the manipulations carried out by EMS representatives. The patient is prescribed short-acting beta-agonists, glucocorticosteroids, and methylxanthines. At the beginning, the drugs are administered intravenously; after the bronchospasm is relieved, the patient’s usual inhalation administration is possible. In order to correct the water-electrolyte balance and blood pH, infusion therapy is prescribed. The level of oxygenation is increased by using an oxygen-helium mixture or supplying 40-50% oxygen through an endotracheal tube.
Note: in the presence of severe hypoxia (SpO2 less than 80%), 100% oxygen can be administered for a short time. The use of this mode is allowed for 3-5 minutes. After this, the O2 concentration in the mixture should be reduced to 40%, and after normalization - to 25-30%.
How to help a patient
In medicine, manifestations of a serious condition that occurs during the progression of the disease are distinguished by stages of severity and principles of first aid.
Clinical symptoms:
- At the first stage, problems arise with exhalation, the patient assumes a peculiar body position, the lips become bluish, a strong dry cough without discharge is tormented, and strong wheezing is heard in the chest. At stage 1, the patient can be helped on an outpatient basis.
- Stage 2 makes itself felt by lethargy and swelling of the chest, cyanosis is concentrated in the fingers and lips, blood pressure drops, pulse rates decrease, and oxygen deficiency occurs.
- At stage 3, the patient suffers from convulsive seizures, the heart rhythm becomes thread-like, and the patient feels a severe lack of oxygen.
Asthmatic type of disease of the second and third degree requires urgent medical attention. The situation is aggravated by the fact that alarming symptoms progress very sharply and if primary signs occur, you need to urgently call an ambulance. Amateur action in this situation is unacceptable, because every minute in such a state counts.
Providing assistance for various forms of asthma
Status asthmaticus can be of allergic or anaphylactic origin. The latter is characterized by spontaneous onset and rapid progression. This condition requires urgent medical attention. Otherwise, the condition will reach respiratory arrest and death. The condition is caused by bronchial spasm, which is almost impossible to stop.
Allergic complications develop gradually. At the same time, attacks of shortness of breath become more regular, and the interval between them becomes shorter. Breathing is not restored between attacks, and the patient experiences a loss of sensitivity to drugs that are indicated to relieve attacks. Therefore, treatment and nurse support can be carried out in stages.
Post-emergency measures
Therapy after first aid is combined and is performed using various medications intended for emergency treatment. The list of necessary drugs includes:
- hormonal agents designed to stimulate bronchial patency and relieve swelling. Used in the form of capsules and injections;
- an additional remedy to the first are methylxanthines, which are intended to improve bronchial patency;
- glucose solutions and other liquids that are used to restore fluid deficiency;
- use of oxygen for therapy.
If a patient with asthma has been diagnosed with status asthmaticus, then additional recovery measures must be taken. These measures include respiratory ventilation, antibiotic drugs, inhalations, and bronchodilators.
The last two types are used after relief of the patient’s condition as emergency medical care. They improve well-being and can be used for life.
The age of the patient is of great importance. Thus, therapeutic tactics in children involve taking medications with a minimal list of side effects. When the doctor has fully studied the patient’s medical history, he selects the optimal technique that helps improve the patient’s condition. At the same time, attention is drawn to the severity of the pathological process.
You should avoid taking sedative medications. These medications make breathing worse. Moreover, long-term use of pharmacological drugs suppresses the cough reflex, and health significantly worsens.