Reasons for ordering an examination
There are a number of indications for prescribing the procedure. Diagnostics is carried out for the purpose of:
- studies of frequent acute respiratory infections, acute respiratory viral infections;
- identifying pathological disorders of the respiratory system with a prolonged cough, respiratory failure, sputum production, chest pain;
- identifying the causes of deviations in the gas exchange process;
- analysis of the relationship between pulmonary diseases and external respiration function, the effectiveness of therapeutic measures in their treatment;
- prevention and early detection of abnormalities in people with an increased risk of developing pathologies: smokers and people whose work activity is associated with harmful substances;
- monitoring the course of bronchopulmonary diseases: pneumonia;
- flu;
- bronchitis;
- asthma;
- chronic obstructive pulmonary disease;
- pulmonary tuberculosis, etc.;
For persons over 40 years of age, who have smoked for 10 years or more, and who have a chronic cough or shortness of breath, examination is mandatory.
Preventive medical measures are recommended for workers associated with the regular use of harmful chemicals.
Indications for spirometry
The doctor may prescribe a diagnosis if the patient has the following symptoms:
- There is a constant cough and severe shortness of breath.
- You can hear wheezing or even whistling in the lungs.
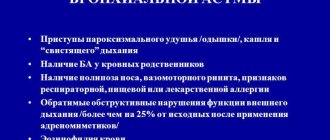
- If the patient has bronchial asthma.
- If there is a serious suspicion of pathology in the lungs.
- A spirometry study is prescribed if it is necessary to prepare for surgery.
- Obstructive pulmonary disease.
Spirometry can be performed frequently. It does not harm human health at all.
View gallery
This is especially recommended for people who work in difficult conditions that can be harmful to the body, as well as those who smoke for a long time or suffer from allergies.
What is spirometry, is it really necessary?
Pulmonary function testing should be performed when:
- symptoms of respiratory diseases;
- identifying sources of abnormal gas exchange;
- assessing the risk of the therapy used for the patient;
- determining physical condition;
- determining the level of bronchial obstruction, especially in COPD (chronic obstructive pulmonary disease).
The results will indicate the correct choice of tactics for treating pathologies of external respiration functions. Spirometry performed in the initial stages increases the patient's chances of recovery. This method will be useful for assessing the health of athletes and smokers.
Spirometry for bronchial asthma detects signs of the disease, and for patients with asthma it monitors the effectiveness of treatment. Timely diagnosis of COPD will allow treatment to begin and death to be avoided. To correctly assess pathologies, in addition to clinical tests, the doctor must examine the patient and listen to his complaints.

Spirometry - what is it?
For reference. Spirometry is a study of air flow that allows you to evaluate external respiratory function (RPF) according to many indicators.
Spirometry is carried out using a special device, represented by a computer with software and a functional part. The latter consists of a mouthpiece, an air-conducting part and air flow sensors.
The patient holds the mouthpiece in his mouth and breathes into it as the doctor says. Air passes through the conductive part and hits the sensor. The latter records the force, speed and volume of the flow, converting this data into various indicators. The computer records all the results, draws graphs and tables.
With the help of the data obtained, a general idea of physical activity is constructed.
For reference. The function of external respiration is the ability of the respiratory system to conduct air from the external environment into the lung tissue and in the opposite direction, as well as the possibility of diffusion of gases through the lung tissue.
Assessment of respiratory function is an important diagnostic and prognostic criterion, therefore spirometry is often performed in patients with lung diseases.
ESSENCE OF THE STUDY
What spirometry is becomes clear from the name of the procedure: spiro meter translates as “breathing measurement.” During the examination, the doctor determines the speed and volume of breathing using a spirometer.
To better understand the essence of the method, you need to turn to the anatomy of the respiratory system. Its 3 main elements are:
- The respiratory tract allows air to pass through.
- Lung tissue is responsible for gas exchange.
- The chest works like a pump.
If the functions of any department are disrupted, it upsets the functioning of the lungs. Spirometry evaluates breathing parameters, which makes it possible to identify respiratory diseases, learn about the severity of pathologies and the effectiveness of therapy.
In addition to the name “spirography”, “spirometry” is also used. This means the same study. These designations differ only in that doctors understand spirography as a method of examining the respiratory organs, and spirography as a graphical recording of measurements made by a spirograph.
Preparing for spirometry
Lung spirometry is performed in the morning on an empty stomach; a low-fat breakfast is allowed 2 hours before the procedure. To ensure the reliability of the test, you should adhere to the basic rules:
- quit smoking in a few hours;
- replace your morning coffee with a healthier drink, such as juice;
- in some cases, the attending physician can stop the patient from taking medications in a few hours;
- choose loose clothing that will make you as comfortable as possible.
20 minutes before the procedure, the patient will be asked to rest and restore respiratory functions while at rest. The doctor must find out whether the subject has diseases that may affect the study of pulmonary function (pneumothorax or myocardial infarction in the first two weeks of development). People after eye surgery or with hemoptysis should perform this test carefully, following the basic recommendations of a specialist.
How is spirometry performed?
The history of the technique begins in Ancient Rome: the Greek physician Galen studied the volumes of inhaled and exhaled air using simple bubbles. Today, a modern method of studying external respiration functions is popular.

Computer spirometry is a sterile procedure that begins with attaching a disposable mouthpiece to the device. After the patient has sat down, he is asked to press his mouth tightly against the disposable mouthpiece and follow the doctor’s recommendations: exhale as much as possible with or without effort, alternating with a calm exhalation. If you exhale at maximum speed for 15 seconds, then you should talk about lung pathologies. All indicators are recorded and performed 3 times. Then the most successful results are selected, with the help of which the pulmonologist makes a diagnosis or adjusts the therapy of an existing disease. The spirometer deciphers the data and automatically calculates respiratory function indicators.
Interpretation of results
Upon completion of data collection, they are analyzed in order to draw up a diagnostic conclusion. In the process of interpreting all the obtained indicators, an electronic spirogram is generated by a computer program. The following values are interpreted.
The number of respiratory movements in one minute is recorded. Its normal values do not exceed 16–17 times.
The volume of air filling the lungs with one breath is determined. Its normal values have a fairly wide range. The limits for healthy men can fluctuate between 300–1200 ml, and for healthy females values within the range of 250–800 ml are typical.
Shows the volume of air absorbed by the lungs in 1 minute. It also has a relatively large interval and ranges between 4–10 liters.
This value is studied when determining the maximum volume of air exhaled by the subject during a quiet exhalation after the deepest inhalation.
The maximum volume of air exhaled by the patient during the deepest (forced) exhalation after the same inhalation is diagnosed. Normally, for individuals this figure ranges from 2.5 to 7.5 liters.
The maximum volume of air exhaled by a person in 1 second during a deep exhalation after an extremely deep inhalation is determined. Its value is significantly influenced by the gender and age of the subject.
Tiffno Index (IT)
Its value is the ratio FEV1/FVC, and is expressed as a percentage.
https://www.youtube.com/watch?v=NOGN2kH8hYE
This value is obtained by multiplying the average amplitude of extreme respiratory excursions and their frequency in 1 minute.
This value looks like MVL/VC, and is indicated as a percentage.
Contraindications to spirometry
Spirometry has no strict contraindications. Mild dizziness, which may occur, passes quickly and does not pose a health hazard. Forced or strong deep inspiration causes a short-term increase in intracranial and intra-abdominal pressure.
The procedure should be carried out with caution or abandoned for the following indications:
- recent operations on the abdominal organs or ophthalmic surgical procedures (less than 2 months ago);
- myocardial infarction or stroke (depending on the patient’s condition, but not earlier than 3 months after);
- previous respiratory tract infections (at least 2 weeks after their supervision);
- a history of pneumothorax;
- arterial or aortic aneurysm;
- severe attacks of bronchial asthma;
- presence of pulmonary hemorrhages;
- epilepsy;
- hypertensive crisis and other pathologies associated with blood pressure disorders;
- increased blood clotting;
- mental disorders;
- pregnancy;
- Age restrictions: up to 5 and after 75 years.
Even in the absence of obvious contraindications, consultation with a specialist is necessary before the study.
Spirometry - explanation
When interpreting the results, two questions are answered: are there any changes in respiratory function and what type of changes occur, if any.
There are three types of respiratory dysfunction:
- Obstructive. Caused by blockage of the airways at any level. Characterized by a decrease in FEV1 and Tiffno index. It occurs most often in bronchitis, COPD and bronchial asthma.
- Restrictive. Caused by a decrease in functioning lung tissue. Characterized by a simultaneous decrease in FEV1, VC and FVC. The Tiffno index remains within normal values. Occurs in pulmonary fibrosis, sarcoidosis, pneumoconiosis, and inflammatory diseases of the lung tissue.
- Mixed. All indicators decrease, which indicates the simultaneous presence of an obstructive and restrictive component. Occurs with atelectasis.
A more detailed interpretation of all indicators and graphs drawn by a computer allows one to suspect a specific pathology.
Spirometry classification
The way the procedure is performed determines its type. Spirometric tests are performed during the following maneuvers:
- normal calm breathing;
- exhale with effort (forced);
- with maximum ventilation;
- with physical activity (before and after it) - dynamic spirometry;
- using special substances - functional and provocative spirometry: with bronchodilators that dilate the bronchi. The method helps to identify hidden bronchospasms, correctly diagnose the disease, determines the reversibility of disorders and the effectiveness of therapeutic techniques;
- with methacholine, which helps to definitively diagnose asthma, identify a predisposition to bronchospasm and hyperresponsiveness.
Modern spirometers make it possible to determine the level of diffusion capacity of the lungs - the gas exchange of oxygen and carbon dioxide between the respiratory organs and the blood.
Additional examination - bronchospirometry. Allows you to separately record indicators in different lobes of the lungs.
Additional study of lung diffusion function
Peak flowmetry norm
- with a persistent cough that does not go away for more than 3-4 weeks;
- shortness of breath, feeling of insufficient inspiration;
- pain in the chest, pressing in nature;
- periodic relapses of chronic bronchitis;
- checking the effectiveness of therapy for bronchial asthma;
- determining the type and degree of pulmonary insufficiency;
- monitoring the rate of disease progression;
- differentiation of pulmonary and cardiovascular failure;
- provocative tests to determine bronchial hyperreactivity;
- long-term smoking habit;
- labor activity in enterprises with polluted air or harmful substances;
- hereditary predisposition to diseases of the respiratory system and allergies.
Spirography is mandatory for military examination and performance tests in combination with other studies of clinical indicators. It is also carried out when performing bronchodilator (with drugs that dilate the bronchi) tests to determine the reversibility of obstruction.
These include:
- severe general condition of the patient;
- 3 degree of circulatory failure;
- severe pulmonary insufficiency;
- hypertensive crisis, angina pectoris;
- arterial hypertension;
- myocardial infarction;
- toxicosis during pregnancy.
Spirography should not be performed on patients with acute forms of cerebral circulatory disorders, such as hemorrhage and ischemic stroke, since even a slight effort can lead to their recurrence.
Modern spirometric devices allow additional testing of lung diffusion function. This applies to clinical diagnostic methods. The study involves assessing the qualitative characteristics of oxygen entering the blood and carbon dioxide released during inhalation and exhalation. If diffusion is reduced, this is a sign of serious pathologies in the function of the respiratory organs.
In the field of spirometry, there is another important test called bronchospirometry. This examination is carried out using a bronchoscope and allows you to evaluate the lungs and external respiration separately. During bronchospirometry, anesthesia must be administered. The examination helps to calculate vital capacity, minute volume of the lungs, respiratory rate, etc.
FEATURES OF SPIROMETRY IN CHILDREN
Spirometric testing is carried out in children from 5 years of age. It is not prescribed at a younger age, since the rules for performing the procedure require taking a maximum breath. Otherwise, spirometry interpretation will be inaccurate.
At the adult level, a child can be examined from the age of 9 years. Before this, you need to try to create a positive atmosphere - with toys, affectionate attitude.
It is better for young patients to undergo spirometry in children's centers, and conventional laboratories do not adapt to their characteristics. Before the procedure, the child should be told in simple language how to inhale and exhale. For intense forced exhalation, images are sometimes used - for example, showing a candle on the screen, asking it to be blown out. The doctor should ensure that the baby's lips are pressed tightly against the mouthpiece. The protocol then indicates the number of successful cycles. Spirometry results are adjusted for age.

RESEARCH RESULTS
Spirometry indicators are the main source of information for diagnosing pulmonary diseases. The norms are average values calculated based on the results of a survey of healthy people. They vary based on gender, age, height, weight and lifestyle.
Spirometry standards are given in the table:
| Parameter | Description | Average rate |
| vital capacity | Vital capacity of the lungs, the main static indicator. All the air from exhalation is at maximum exhalation after the same inhalation. | There is no norm for vital capacity; other parameters are calculated on its basis. |
| FVC | Forced vital capacity, the main dynamic indicator. The volume of air entering the lungs during intense exhalation. This is necessary to clarify the patency of the bronchi: as their lumen decreases, FVC also decreases. | 70-80% VEL. |
| BH | Respiratory rate, number of inhalations and exhalations at rest. | 10-20/min. |
| BEFORE | Tidal volume (from inhalation and exhalation in 1 cycle). | 0.3-0.8 l (15-20% vital capacity). |
| MAUD | Minute volume of respiration, that is, passed through the lungs in 1 minute. | 4-10 l/min. |
| District Department of Internal Affairs | The inspiratory reserve volume, that is, the maximum inhaled during a normal inhalation. | 1.2-1.5 l (50% vital capacity). |
| ROvyd | Expiratory reserve volume. | 1-1.5 l (30% vital capacity). |
| FEV1 | Forced expiratory volume in 1 second. | > 70% FVC. |
| JEL | Proper vital capacity for a healthy person, based on physical parameters. Men: 0.052 * height (cm) – 0.028 * age – 3.2 Women: 0.049 * height – 0.019 * age – 3.76 | 3-5 l. |
| OOL | Residual volume of the lungs, that is, remaining after exhalation. | 1-1.5 l or 20-30% VOL. |
| OEL | The total capacity of the lungs, or how much air can be held in the lungs after inhalation. It is calculated as follows: VOL + VEL. | 5-7 l. |
| Tiffno index | FEV1 (ml) / Vital capacity (ml) * 100%. | > 70-75 %. |
Ventilation failure can be obstructive or restrictive. The first develops due to a decrease in the lumen of the bronchi with an increase in resistance to air flow. The second occurs due to a decrease in the ability of lung tissue to stretch.
When deciphering the results, the following parameters indicate the obstructive type:
- ELC is normal or higher;
- Tiffno index is underestimated;
- EOL increased.
- FEV1 decreased.
With restrictive insufficiency, TLC decreases.
Research methodology
- the patient sits down, a clamp is attached to his nose;
- A mouthpiece is placed in the patient’s mouth and he takes several breaths at a normal pace;
- inhale and exhale slowly;
- break 20 seconds;
- repeating inhalations and exhalations at a normal pace;
- quickly inhale through the chest and exhale.
To take a spirogram, the patient must be seated as comfortably as possible. His clothing should not compress the chest and interfere with free breathing. The seat on which the subject sits and the oral tube are installed in accordance with his height, so that he does not have to bend over or stretch his neck upward. You also need to control the position of your torso when exhaling - do not let your body lean forward.

When performing spirography, it is necessary to sit the patient so that it is comfortable for him to perform breathing tests
The test analyzes oral airflow measurements and requires the patient to use a nose clip and hold the mouthpiece tightly to prevent air leakage. If the subject has dentures installed, they cannot be removed, as this will disrupt the quality fixation of the mouthpiece.
First, several primary tests are carried out - measuring tidal volume (TI), which is calculated based on the average of six or more respiratory cycles at rest. Then, in a calm state, the respiratory rate (RR) is determined. The product of these values will give the minute volume of breathing. A new type of spirograph, equipped with software, automatically provides all calculations.
The spirograph processes information immediately during the study and produces a tape with recorded results. At the signal from the diagnostician, the examinee inhales as completely as possible, and then exhales as sharply and as long as possible. The exhalation time should take at least 6 seconds and the patient should maintain maximum effort throughout the exhalation until completion.
Often, individuals undergoing testing are unable to inhale and exhale properly the first time, so the test is carried out using several attempts under the control of a recorded curve. Then the subject needs to breathe with maximum depth and frequency for 12 seconds. In certain cases, in some patients, such tests can cause dizziness, “floaters” before the eyes or darkening and even fainting, but the latter conditions are diagnosed quite rarely.
CONTRAINDICATIONS
During the procedure, weakness and dizziness sometimes appear, which quickly disappear. An increase in pressure is also possible due to the load on the chest, since inhalation is made with effort.
Due to the possible deterioration of the patient's condition during spirometry, it is not prescribed in the following cases:
- operations on the eyes, sternum, and abdomen undergone during the last two months;
- pulmonary hemorrhage;
- metabolic disorders;
- heart attack or stroke that occurred less than a month ago;
- pneumothorax;
- uncontrolled hypertension;
- mental disorders;
- age less than 5 and more than 75 years.
The study is sometimes prescribed even if there are contraindications, but then doctors must be ready to provide emergency assistance to the patient.

IS IT POSSIBLE TO FICTION THE SpirOMETER?
To work in hazardous conditions, you must undergo a medical examination, including spirometry. The ability to continue working depends on whether the indicators are normal. In such cases, some try to deceive the device and the doctor, but this is not easy to do. During the procedure, the patient exhales 3 times, and if the specialist’s instructions are followed, this reduces the risk of errors to a minimum.
Inaccuracies in spirography occur when incorrect information about age, height and weight is provided in an attempt to obtain normal values, and also when the procedure is violated if the person breathes with insufficient intensity or takes a shallow breath.
Spirometry is a safe and informative method for diagnosing pathologies of the lungs and bronchi. During the examination, breathing parameters are measured, which allows you to identify the disease or find out the effectiveness of medications. By providing reliable information about weight, height, age and following the procedure, the results are accurate and the risk of errors is minimal.
SOURCE: https://proskopiyu.ru/metody/spirometriya.html https://tvojajbolit.ru/issledovaniya/spirometriya-spirografiya-chto-eto-takoe-pokazaniya-i-protivopokazaniya-rasshifrovka-rezultatov-fvd-funktsii-vneshnego -dyihaniya/ https://astmabronhit.ru/spirometriya-normalnie-pakazateli-tablitsa.html